56 Caudal Epidural Block
The sacral hiatus is the caudal termination of the sacral canal. The volume of the epidural space within the sacral canal is highly variable, with estimates ranging from 10 to 26 mL in adults (Table 56-1).1 In this study of 37 adults (23 female, 14 male), the sacrococcygeal membrane was significantly thicker in females than in males (mean values, 3.6 and 2.5 mm, respectively).1 The sacral canal volume was significantly smaller in females than in males (mean values 13.2 and 16.5 mL, respectively).1 Because the sacral canal volume varies, the dose required to achieve a given level of caudal epidural block varies from individual to individual.
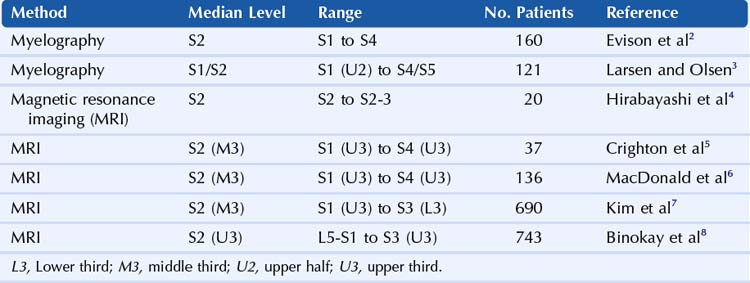
Table 56-1 Magnetic Resonance Imaging Estimates of Caudal Space Anatomy in Adults
| Mean Value | Range | |
|---|---|---|
| PATIENT DATA | ||
| Height (cm) | 168 | 150-183 |
| Weight (kg) | 72 | 49-120 |
| SACROCOCCYGEAL MEMBRANE | ||
| Absence (%) | 10.8 | |
| Thickness (mm) | 3.2 | 1-5 |
| SACRAL CANAL | ||
| Maximum anteroposterior diameter (mm) | 4.6 | 1-8 |
| Angle (degrees) | 57.9 | 40-74 |
| Volume (mL) | 14.4 | 9.5-26.6 |
| DURAL SAC | ||
| Shortest distance from sacrococcygeal membrane to dural sac (mm) | 60.5 | 34-80 |
Adapted from Crighton IM, Barry BP, Hobbs GJ. A study of the anatomy of the caudal space using magnetic resonance imaging. Br J Anaesth 1997;78:391–5.
In adults, the dural sac of the subarachnoid space ends between the S1 and S2 sacral segments.1 In this study, the distance between the dural sac and sacrococcygeal ligament ranged from 34 to 80 mm. The S5 and coccygeal nerves normally exit the sacral canal through the sacral hiatus. The sacral and coccygeal cornua (horns) articulate to form an archlike structure. Table 56-2 summarizes the estimates of the level of the caudal termination of the dural sac in adults gathered from several studies.
Variations in sacral anatomy are relatively common. A number of conditions can make caudal block difficult, including narrowing or complete absence of the sacral hiatus.9,10 These conditions occur in 3% to 6% of anatomic specimens. The sacral cornua are prominent (>3 mm of bony prominence on each side) in only 21% of adult sacrums,9 and therefore assessment by palpation is problematic.
The sacral epidural space is highly vascular. Inadvertent intravenous injection is relatively common during caudal block, occurring in about 5% to 10% of these procedures.11
Landmarks for caudal block are traditionally assessed by palpation. The posterosuperior iliac spines (the superolateral sacral crests of the sacrum) form an equilateral triangle with the sacral hiatus.10 Although this approximation is accurate, the clinical assessment of landmark position can be difficult. Traditional techniques also rely on tactile sense of needle entry into the caudal space. However, the sacrococcygeal ligament is soft in children and may therefore not be easy to detect manually by needle advancement.12
Ultrasound can be used to guide caudal blocks in pediatric and adult patients.13,14 Sonography can determine the location and size of the sacral hiatus for needle tip placement. In addition, ultrasound can be used to image the distribution after caudal epidural injection. However, the bone of the sacrum prevents ultrasound imaging of most of the sacral canal. One concern is that acoustic shadowing from the overlying bone can prevent detection of intravascular injection during caudal blocks, particularly in adults. Ultrasound imaging may be of particular utility in guiding caudal injections in patients with spinal dysraphism.15
Suggested Technique
Caudal block with ultrasound is optimally performed in prone position with sterile transducer cover and skin preparation. The wide variety of transducer selections for caudal block depend on patient size.11 In thin adult patients, a 5- to 10-MHz small-footprint “hockey-stick” transducer is appropriate. Average-sized adults image well with a standard linear transducer for the procedure. For obese patients, a lower frequency curvilinear array is optimum.
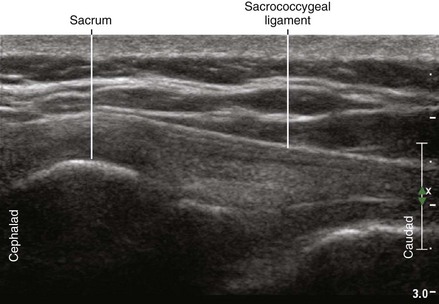
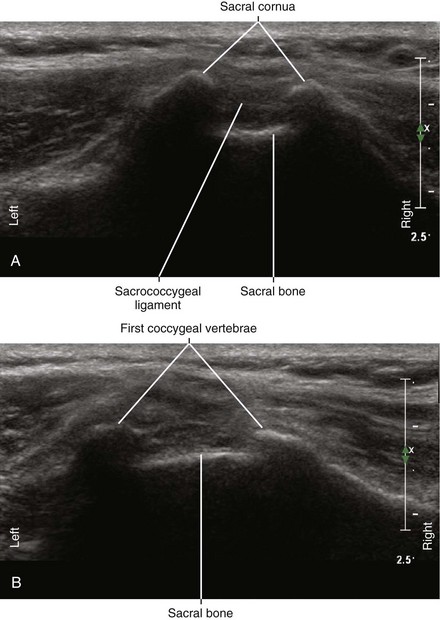
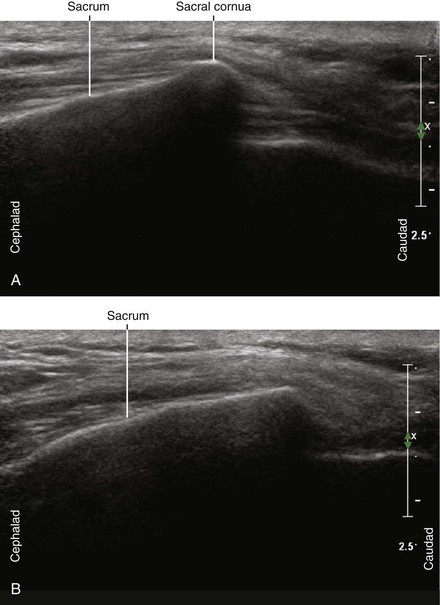
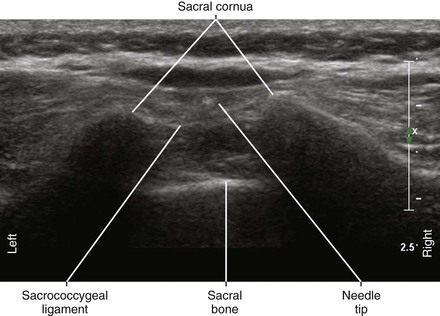
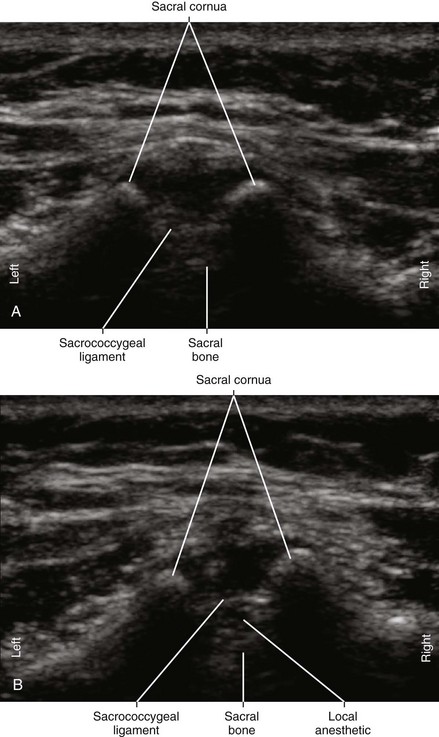
The sacral hiatus is easiest to image in transverse view over the midline.14 The sacral cornua appear as two reverse U-shaped hyperechoic structures. The sacrococcygeal ligament and base of the sacrum appear as two parallel bandlike structures between the cornua. The sacral hiatus lies between these two hyperechoic bands.
Ultrasound imaging can be used to assess the injection distribution for caudal block.13 Some investigators have favored a transverse view to assess the test injection distribution.16 With the probe in transverse position, it is possible to observe bilateral spread. Anterior displacement of the posterior dura occurs in more than 90% of caudal epidural injections.15 Turbulence of the injection, as manifested by a mosaic pattern on color Doppler, also indicates successful injection. Longitudinal paramedian view can be advantageous for assessing the level of injection in adults with the sacrum in the field as a reference point.
Clinical Pearls
Caudal Epidural Anatomy
• The sacral canal is a continuation of the vertebral canal that terminates as the sacral hiatus. The sacral hiatus is formed by nonfusion of the fifth sacral vertebral arch and is covered by the sacrococcygeal membrane. There is wide variation in the anatomy of the sacrum, particularly in pediatrics.17,18 The caudal canal is narrowest at the sacral hiatus. Sonography can be used to determine whether the sacral hiatus is patent.
Caudal Epidural Ultrasound Anatomy
• The sacrococcygeal ligament can be visible as one or two layers in transverse view. These layers are much less echobright than the underlying bone of the sacral canal.
• The transducer must be tilted to enhance echoes from the sacrococcygeal ligament because it exhibits a high degree of anisotropy. For this same reason it is difficult to visualize the sacrococcygeal ligament along its entire length.
• In longitudinal view, the caudal epidural space appears as hypoechoic and tapering underneath the fibrillar sacrococcygeal ligament.
Needle Angle
• A shallow angle of approach is essential to place the needle within the epidural space of the sacral canal.
• The optimal angle for needle insertion, defined by the base of the sacrum and the skin surface, is about 21 degrees in children.12
• In adults, the angle of the sacral canal varies with gender. This angle is about 20 degrees in men and 30 to 45 degrees in women.
Needle Advancement
• Because the sacrococcygeal ligament is thick (≈3 mm in adults),1 the needle should be advanced after visible and tactile sense of tent and recoil so that the entire bevel opening is within the caudal epidural space.19,20
Injection
• Because caudal epidural injections have low resistance, the visible color distribution should fill the entire epidural space within the field of view.
• Caudal epidural injections can appear similar to intravascular injections with ultrasound imaging.
• Tenting of the sacrococcygeal ligament and caudal displacement of the canal are signs of correct caudal epidural injection.
• One dominant color indicates successful caudal epidural steroid injection.19
Clinical Assessment
• The lateral aspect of the foot is reliably innervated by S1 for cutaneous assessment of the upper extent of sacral caudal block.
• Narrow sacral canal has been associated with failure of caudal epidural injections. Specifically, no patients with sacral canal diameters less than 2 mm (as measured at the apex of the sacral hiatus) had successful blocks in one clinical series.22
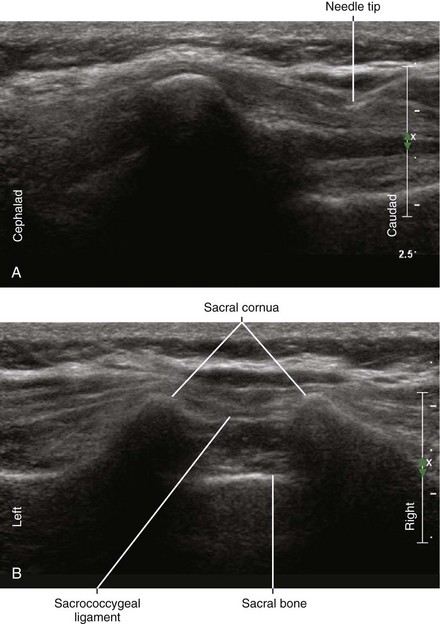
FIGURE 56-4 Longitudinal in-plane approach to caudal epidural block (A). The corresponding transverse view is shown (B).
1 Crighton IM, Barry BP, Hobbs GJ. A study of the anatomy of the caudal space using magnetic resonance imaging. Br J Anaesth. 1997;78:391–395.
2 Evison G, Windsor P, Duck F. Myelographic features of the normal sacral sac. Br J Radiol. 1979;52:777–780.
3 Larsen JL, Olsen KO. Radiographic anatomy of the distal dural sac. A myelographic investigation of dimensions and termination. Acta Radiol. 1991;32:214–219.
4 Hirabayashi Y, Shimizu R, Saitoh K, et al. Anatomical configuration of the spinal column in the supine position. I. A study using magnetic resonance imaging. Br J Anaesth. 1995;75:3–5.
5 Crighton IM, Barry BP, Hobbs GJ. A study of the anatomy of the caudal space using magnetic resonance imaging. Br J Anaesth. 1997;78:391–395.
6 MacDonald A, Chatrath P, Spector T, et al. Level of termination of the spinal cord and the dural sac: a magnetic resonance study. Clin Anat. 1999;12:149–152.
7 Kim JT, Bahk JH, Sung J. Influence of age and sex on the position of the conus medullaris and Tuffier’s line in adults. Anesthesiology. 2003;99:1359–1363.
8 Binokay F, Akgul E, Bicakci K, et al. Determining the level of the dural sac tip: magnetic resonance imaging in an adult population. Acta Radiol. 2006;47:397–400.
9 Sekiguchi M, Yabuki S, Satoh K, et al. An anatomic study of the sacral hiatus: a basis for successful caudal epidural block. Clin J Pain. 2004;20:51–54.
10 Senoglu N, Senoglu M, Oksuz H, et al. Landmarks of the sacral hiatus for caudal epidural block: an anatomical study. Br J Anaesth. 2005;95:692–695.
11 Klocke R, Jenkinson T, Glew D. Sonographically guided caudal epidural steroid injections. J Ultrasound Med. 2003;22:1229–1232.
12 Park JH, Koo BN, Kim JY, et al. Determination of the optimal angle for needle insertion during caudal block in children using ultrasound imaging. Anaesthesia. 2006;61:946–949.
13 Rapp HJ, Grau T. Ultrasound imaging in pediatric regional anesthesia. Can J Anaesth. 2004;51:277–278.
14 Chen CP, Tang SF, Hsu TC, et al. Ultrasound guidance in caudal epidural needle placement. Anesthesiology. 2004;101:181–184.
15 Roberts SA, Guruswamy V, Galvez I. Caudal injectate can be reliably imaged using portable ultrasound: a preliminary study. Paediatr Anaesth. 2005;15:948–952.
16 Schwartz D, Raghunathan K, Dunn S, et al. Ultrasonography and pediatric caudals. Anesth Analg. 2008;106:97–99.
17 Adewale L, Dearlove O, Wilson B, et al. The caudal canal in children: a study using magnetic resonance imaging. Paediatr Anaesth. 2000;10:137–141.
18 Beek FJ, Bax KM, Mali WP. Sonography of the coccyx in newborns and infants. J Ultrasound Med. 1994;13:629–634.
19 Yoon JS, Sim KH, Kim SJ, et al. The feasibility of color Doppler ultrasonography for caudal epidural steroid injection. Pain. 2005;118:210–214.
20 Broadman L, Ivani G. Caudal blocks. Tech Reg Anesth Pain Med. 1999;3:150–156.
21 Ghia JN, Arora SK, Castillo M, et al. Confirmation of location of epidural catheters by epidural pressure waveform and computed tomography cathetergram. Reg Anesth Pain Med. 2001;26:337–341.
22 Chen CP, Wong AM, Hsu CC, et al. Ultrasound as a screening tool for proceeding with caudal epidural injections. Arch Phys Med Rehabil. 2010;91(3):358–363.