Case 8
HISTORY AND PHYSICAL EXAMINATION
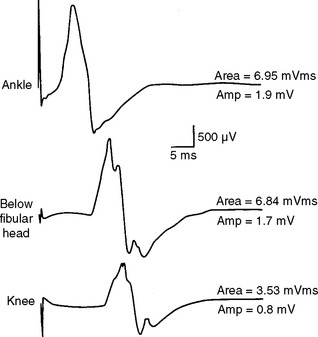
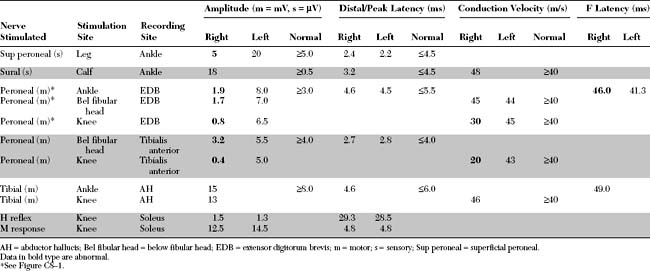
Please now review the Nerve Conduction Studies (NCS) and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
Relevant electrodiagnostic (EDX) findings in this case include the following:
DISCUSSION
Applied Anatomy
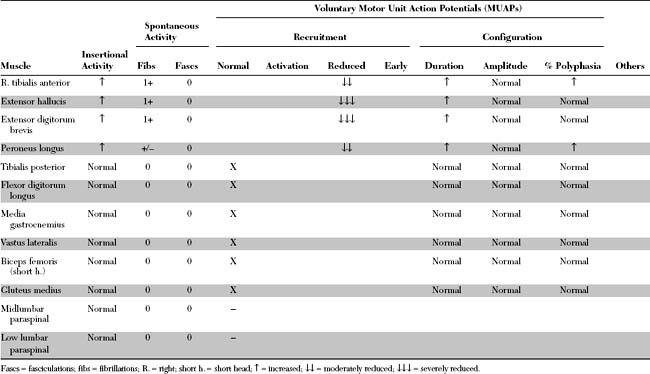
The common peroneal nerve (also called the lateral popliteal nerve) shares a common sheath with the tibial nerve (also called the medial popliteal nerve) to form the sciatic nerve. The common peroneal nerve innervates the short head of biceps femoris only, via a motor branch that exits the nerve close to the gluteal fold. All the other hamstring muscles (long head of biceps femoris, semitendinosus and semimembranosus) are innervated by the tibial nerve. The complete separation of the common peroneal nerve from the tibial nerve is variable, but is usually at the popliteal crease or up to 10 cm above it (Figure C8-2).
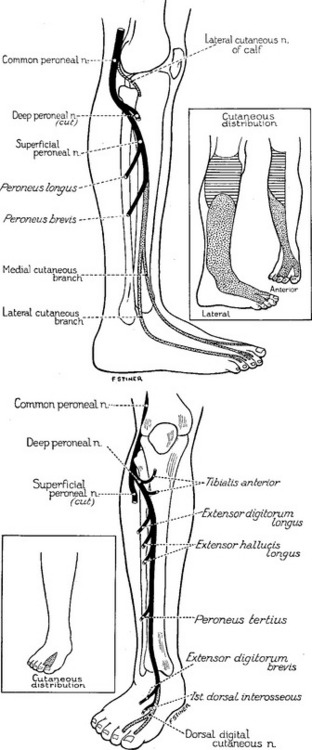
Soon after separating from the tibial nerve in the popliteal fossa, the common peroneal nerve gives off first the lateral cutaneous nerve of the calf, which innervates the skin over the upper third of the lateral aspect of the leg (Figure C8-3, top inset). It also gives the peroneal communicating nerve which joins the sural nerve in midcalf. Then, the common peroneal nerve winds around the fibular neck, where it lies in close contact with it, and passes through a tendinous tunnel between the edge of the peroneus longus muscle and the fibula, sometimes referred to as the fibular tunnel.
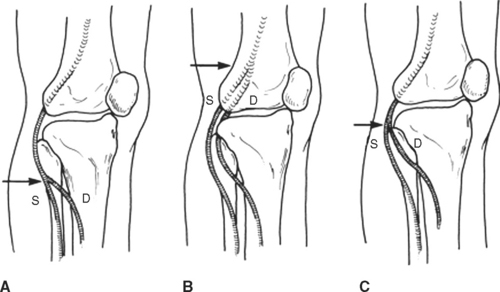
The common peroneal nerve divides into superficial and deep terminal branches usually near the fibular neck but sometimes more proximally (Figure C8-4). The common peroneal nerve around the fibular neck has a topographical arrangement where the fibers to the superficial branch are placed laterally while those destined to the deep peroneal nerve are located medially in close contact with the fibular bone. This renders the deep peroneal nerve more susceptible to compression at the fibular neck than the superficial nerve.
The superficial peroneal nerve innervates the peroneus longus and brevis and the skin of the lower two thirds of the lateral aspect of the leg and the dorsum of the foot (see Figure C8-3, top). The deep peroneal nerve is primarily motor; it innervates all ankle and toe extensors (the tibialis anterior, the extensor hallucis, and the extensor digitorum longus and brevis) and the peroneus tertius, in addition to the skin of the web space between the first and second toes (see Figure C8-3, bottom).
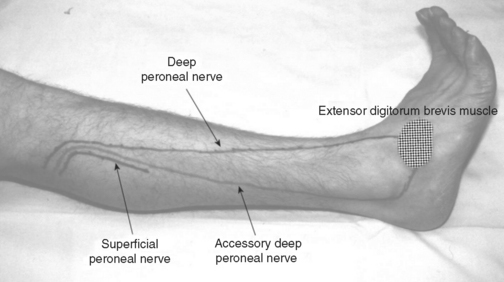
The accessory deep peroneal nerve is a common anomaly of the peroneal nerve. It is present in about 20+ of the population and sometimes bilaterally. The nerve arises as a motor branch of the superficial peroneal nerve, usually a continuation of the muscular branch that innervates the peroneus brevis muscle. The accessory deep peroneal nerve traverses along the posterior aspect of the peroneus brevis muscle, and then, accompanied by peroneus brevis tendon, passes behind the lateral malleolus near the sural nerve to reach the foot. There, it sends branches to the lateral part of extensor digitorum brevis, ankle joint, and ligaments (Figure C8-5).
Clinical Features
Peroneal mononeuropathy usually presents with a foot drop, defined as severe weakness of ankle dorsiflexion (extension) with intact plantar flexion. Foot drop should be distinguished from flail foot which, in contrast, is characterized by no or minimal ankle and foot movements in all directions, including severe weakness of ankle dorsiflexion, plantar flexion, and intrinsic foot muscles. Voluntary movement at or distal to the ankle occur in foot drop due to intact plantar flexion and intrinsic foot muscles, but are absent in flail foot. Table C8-1 lists the common causes of unilateral and bilateral footdrop, starting caudally and progressing cephalad along the neuraxis.
* Including the Markesburry-Udd, Welander, Nonaka, and Liang types.
Peroneal mononeuropathy is the most common compressive mononeuropathy in the lower extremity. All age groups are equally affected but the disorder is almost three times more common in men. Most peroneal nerve lesions are unilateral, and affect the right and the left side equally. Bilateral lesions constitute about 10+ of cases. In most cases, it results from prolonged compression of the peroneal nerve at the fibular neck between an external object and the rigid bone. Table C8-2 lists the causes of peroneal mononeuropathy at the fibular head.
Table C8-2 Causes of Peroneal Nerve Lesions at the Fibular Neck
Adapted with revision from Katirji B. Compressive and entrapment mononeuropathies of the lower extremity. In: Katirji B, Kaminski HJ, Preston DC, Ruff RL, Shapiro BE, eds. Neuromuscular disorders in clinical practice. Boston, MA: Butterworth-Heinemann, 2002.
Most cases of peroneal mononeuropathy present with acute footdrop. However, footdrop develops in some patients subacutely over days or even weeks. The precipitating factors vary according to the mode of onset (acute versus nonacute). Figure C8-6 shows the relative frequency of the precipitating factors in relation to the mode of onset. Perioperative compression and trauma are the two most common causes of acute peroneal mononeuropathy at the fibular head. However, weight loss and prolonged hospitalization are the two major precipitating factors for peroneal nerve lesions with subacute or gradual onset. Extrinsic masses (osteomas, ganglia, lipomas, Baker cysts), or intrinsic nerve sheath tumors usually present with a slowly progressive footdrop.
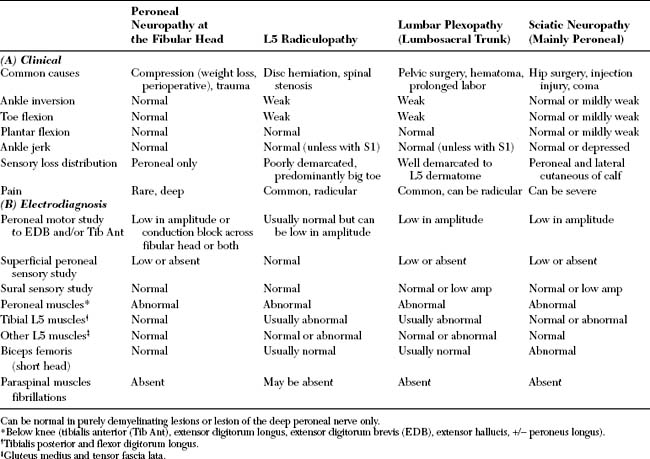
Although the deep peroneal nerve is more frequently affected than the superficial nerve (as in this patient), selective deep peroneal nerve involvement is not uncommon. Peroneal neuropathies in the thigh (i.e., sciatic nerve lesions affecting the common peroneal nerve exclusively) are rare, accounting for less than 5+ of all peroneal mononeuropathies. Table C8-3(A) reveals the most helpful clinical distinctions between peroneal mononeuropathy, lumbar plexopathy, L5 radiculopathy, and sciatic mononeuropathy. In short, weakness of ankle inversion, toe flexion, or plantar flexion, and absent or depressed ankle jerk are findings that are not consistent with a selective peroneal nerve lesion.
In the management of acute compressive lesions, patients should be treated in a way that allows for improvement by either remyelination or reinnervation. As can be seen in this patient, conduction block lesions (due to segmental demyelination) recover spontaneously within 2 to 3 months as long as further compression is prevented. Proper padding of beds, prevention of leg crossing, and attempts to arrest or reverse weight loss should be initiated promptly. Ankle bracing is important when the footdrop is profound, to prevent ankle contractures and sprains. Surgical intervention is indicated (1) when the nerve is lacerated; (2) when clinical and/or EMG evidence for reinnervation cannot be established in the anterior compartment muscles (the tibialis anterior and the peroneus longus) 4 to 6 months after injury; and (3) in slowly progressive peroneal mononeuropathies.
Electrodiagnosis
Electrodiagnostic Strategy
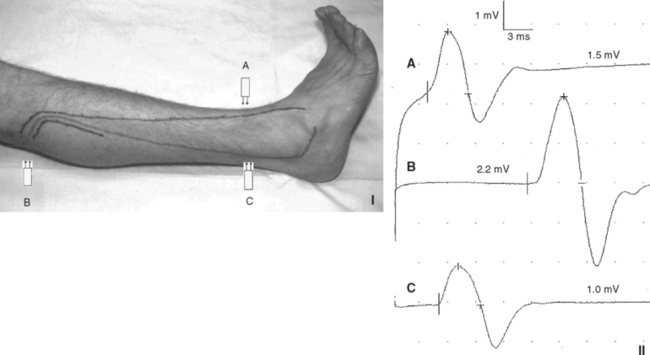
A technical pitfall may arise during peroneal motor NCS recording EDB if there is an associated accessory deep peroneal nerve anomaly. The peroneal CMAP amplitude is larger stimulating proximally than distally since the anomalous fibers are not present at the ankle. This anomaly can be confirmed by stimulating behind the lateral malleolus (Figure C8-7). This yields a CMAP (not present in normal situations) that, when added to the distal CMAP, is approximately equal or higher than the CMAP obtained with proximal peroneal nerve stimulations.
Electrodiagnostic Findings in Peroneal Mononeuropathies
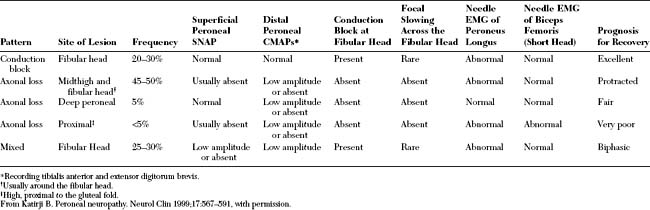
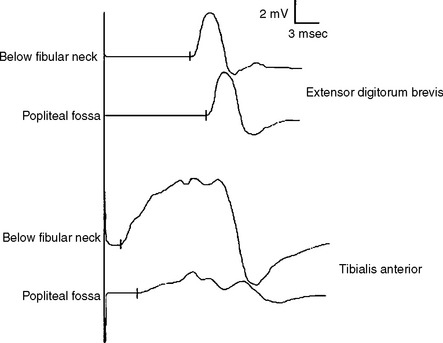
The findings on nerve conduction studies in peroneal mononeuropathies are extremely helpful in establishing a correct diagnosis and excluding other causes of foot drop, particularly L5 radiculopathy or sciatic mononeuropathy (see Table C8-3(B)). The EDX findings in peroneal mononeuropathies can be divided into several patterns (Figure C8-8 and Table C8-4):
Conduction block lesions are due to segmental demyelination and carry excellent prognosis with expected recovery in two to three months provided the cause of compression is eliminated. In contrast to carpal tunnel syndrome and ulnar neuropathy across the elbow, peroneal motor conduction velocities are usually normal and focal slowing across the fibular head is not a common feature of peroneal mononeuropathy. When present, it is always associated with a localizing conduction block, and it may be seen during the recovery phase of these lesions.
In mixed common peroneal nerve lesions at the fibular head, it is not uncommon to find low-amplitude peroneal CMAP, recording EDB, without conduction block, along with a definite conduction block across the fibular head, while recording tibialis anterior. This is extremely helpful prognostically, since conduction block due to segmental demyelination carries an excellent prognosis for recovery, while axonal lesions require much longer time for reinnervation.
Aprile I, Caliandro P, Giannini F, et al. Italian multicentre study of peroneal mononeuropathy at the fibular head: study design and preliminary results. Acta Neurochir Suppl. 2005;92:63-68.
Berry H, Richardson PM. Common peroneal nerve palsy: a clinical and electrophysiological review. J Neurol Neurosurg Psychiatry. 1976;39:1162-1171.
Devi S, Lovelace RE, Duarte N. Proximal peroneal nerve conduction velocity: recording from anterior tibial and peroneus brevis muscle. Ann Neurol. 1977;2:116-119.
Jabre JF. The superficial peroneal nerve revisited. Arch Neurol. 1981;38:666-667.
Katirji B. Peroneal neuropathy. Neurol Clin N Am. 1999;17:567-591.
Katirji MB, Wilbourn AJ. Common peroneal mononeuropathy: a clinical and electrophysiologic study of 116 lesions. Neurology. 1988;38:1723-1728.
Katirji MB, Wilbourn AJ. High sciatic lesions mimicking peroneal neuropathy at the fibular head. J Neurol Sci. 1994;121:172-175.
Marciniak C, Armon C, Wilson J, et al. Practice parameter: utility of electrodiagnostic techniques in evaluating patients with suspected peroneal neuropathy: an evidence-based review. Muscle Nerve. 2005;31:520-527.
Pickett JB. Localizing peroneal nerve lesions to the knee by motor conduction studies. Arch Neurol. 1984;41:192-195.
Sourkes M, Stewart JD. Common peroneal neuropathy: a study of selective motor and sensory involvement. Neurology. 1991;41:1029-1033.