Case 3
HISTORY AND PHYSICAL EXAMINATION
An electrodiagnostic (EDX) examination was performed.
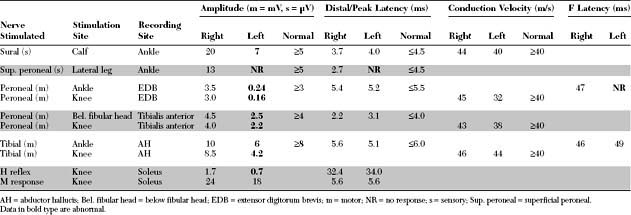
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
Pertinent EDX findings include:
DISCUSSION
Applied Anatomy
The sciatic nerve (Figure C3-1) leaves the pelvis via the sciatic notch and then passes, usually, under the piriformis muscle, which is covered by the gluteus maximus. In healthy individuals, the sciatic nerve passes underneath the piriformis muscle in 85 to 90+ of cases, while in the rest, the peroneal division only passes above or through the muscle. Rarely (1 to 2+ of persons), the entire sciatic nerve pierces the piriformis muscle.
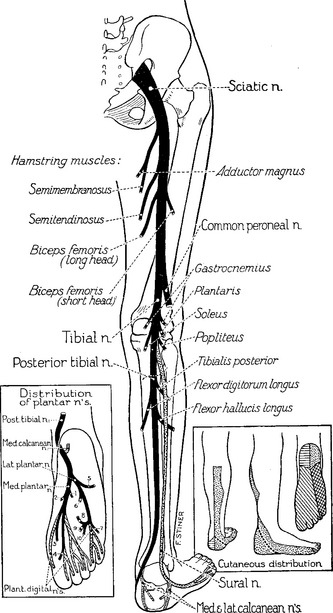
Figure C3-1 The sciatic nerve and its main branches.
(Reprinted with permission from Haymaker W, Woodhall B. Peripheral nerve injuries: principles of diagnosis. Philadelphia, PA: WB Saunders, 1953.)
The superior gluteal nerve, which innervates the gluteus medius and minimus and tensor fascia lata, branches off the sciatic trunk before the piriformis. However, the inferior gluteal nerve, which innervates the gluteus maximus, passes under the muscle (Figure C3-2). In the thigh, the tibial nerve innervates most hamstring muscles (semitendinosus, semimembranosus, and the long head of the biceps femoris), except the short head of the biceps femoris; the latter is the only hamstring muscle innervated by the common peroneal nerve. Also, the tibial nerve contributes, with the obturator nerve, to innervation of the adductor magnus muscle.
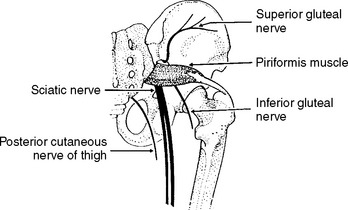
Figure C3-2 The nerve of the sciatic notch and the piriformis muscle.
(Reprinted from Stewart JD. Focal peripheral neuropathies, 2nd ed. New York: Raven Press, 1993, with permission.)
The sciatic nerve divides into its two terminal branches near the midthigh, although this is extremely variable and the separation may be as low as the popliteal fossa. In the popliteal fossa and before it winds around the fibular neck, the common peroneal nerve gives off first the lateral cutaneous nerve of the calf, which innervates the skin over the upper third of the lateral aspect of the leg. At the fibular neck, the common peroneal nerve lies in close contact with the bone, and passes through a tendinous tunnel, sometimes referred to as the fibular tunnel, which is formed between the edge of the peroneus longus muscle and the fibula. Near that point, the common peroneal nerve divides into superficial and deep branches (see Figure C8-3, Case 8). The superficial peroneal nerve innervates the peroneus longus and brevis, as well as the skin of the lower two-thirds of the lateral aspect of the leg and the dorsum of the foot. The deep peroneal nerve is primarily a motor nerve; it innervates the ankle and toe extensors (the tibialis anterior, extensor hallucis, extensor digitorum longus, and brevis) and the peroneus tertius, in addition to a small area of skin in the web space between the first and second toes.
While in the calf, the tibial nerve innervates the gastrocnemius, soleus, tibialis posterior, flexor digitorum profundus, and flexor hallucis longus. At the medial aspect of the ankle, the tibial nerve passes through the tarsal tunnel and divides at, or slightly distal to, the tunnel into its three terminal branches (see inset of Figure C3-1): (1) the calcaneal branch, a purely sensory nerve that innervates the skin of the sole of the heel; (2) the medial plantar nerve, which innervates the abductor hallucis, the flexor digitorum brevis, and the flexor hallucis brevis, in addition to the skin of the medial sole and, at least, the medial three toes; and (3) the lateral plantar nerve, which innervates the abductor digiti quinti pedis, the flexor digiti quinti pedis, the adductor hallucis, and the interossei, in addition to the skin of the lateral sole and two lateral toes.
Clinical Features
Table C3-1 lists the common causes of sciatic mononeuropathy. Total hip joint replacement is currently a leading cause of such lesions, and sciatic nerve injury is the most common neurologic complication of total hip arthroplasty, particularly with revisions or procedures requiring limb lengthening, and in patients with congenital hip dislocation or dysplasia. The estimated incidence of sciatic nerve lesion following total hip replacement is about 1–3+, although EDX studies may detect subclinical signs of sciatic nerve damage in as many as 70+ of patients. The sciatic nerve lesion is due to direct intraoperative stretch injury, but occasionally is caused by hemorrhage, prosthetic dislocation, migrating trochanteric wire, or leaking cement (methylmethacrylate) used in the arthroplasty. The manifestations of the sciatic nerve injury are acute and often noted in the immediate postoperative period. Occasionally, the onset of symptoms is delayed for several years, and the injury is due to prosthetic dislocation, osseous formation, or migrating trochanteric wire. Hip fracture or dislocation, or femur fracture may also result in sciatic nerve injury, which may also occur during closed reduction or internal fixation. External compression of the sciatic nerve is the second common cause of sciatic nerve lesions at the hip. This usually occurs in the setting of unattended coma (such as with drug overdose), but occasionally follows operative positioning in the sitting position (such as with craniotomy), poor positioning of unconscious patient (such as in the intensive care unit), or prolonged sitting (“toilet seat” and “lotus” neuropathies). Mass lesions in the buttock or thigh, such as malignant or benign tumors, persistent sciatic artery, or enlargement of the lesser trochanter (possibly from frequent sitting on hard benches), may compress the sciatic nerve. Open injuries of the sciatic nerve are usually caused by gunshot wounds, knives, or other sharp objects. Hemorrhage within the gluteal compartment is sometimes associated with sciatic nerve lesions. This may occur during anticoagulant therapy, in hemophiliacs, or following rupture of an iliac artery aneurysm or hip surgery. Intramuscular gluteal injections, not administered properly in the upper outer quadrant of the buttock particularly in thin patients or children, may damage the sciatic nerve or its peroneal component exclusively. This often occurs soon after the injection of a large quantity of a neurotoxic drug but may be delayed following repeated injections or due to fibrosis. Menstruating women with endometriosis may have cyclic radicular pain (i.e., sciatica) or overt sciatic mononeuropathy. Typically, the symptoms start few days before menstruation and stop after menses end. With progression of disease, the manifestations of endometriosis become more constant, though often worse during menses. Ischemia resulting in sciatic nerve injuries may be due to vasculitis involving the vasa nervorum, or occlusion of the iliac or femoral artery such as during intra-aortic balloon pump therapy with a catheter placed through the ipsilateral femoral artery. Occasionally, a slowly progressive sciatic mononeuropathy is idiopathic and no identifiable cause is identified despite imaging studies and surgical exploration.
Table C3-1 Common Causes of Sciatic Mononeuropathy (Listed in Descending Order of Frequency)
Severe or complete sciatic nerve lesion is associated with weakness of all the muscles below the knee and the hamstrings with sensory loss below the knee that spans both the peroneal and tibial distributions but spares the saphenous nerve distribution (the medial leg). In contrast, a partial sciatic nerve lesion usually affects the peroneal more than the tibial division, and mimics a common peroneal nerve lesion at the fibular neck. It usually presents with foot drop and sensory loss mostly in common peroneal nerve distribution. This lesion may be difficult to differentiate from peroneal mononeuropathy, lumbosacral radiculopathy, and lumbosacral plexopathy. Table C3-2 lists some clinical hints that cast doubt on a peroneal nerve lesion at the fibular head in patients presenting with footdrop, while Table C3-3 (A) lists the differential diagnoses of patients with footdrop. Note that dysesthetic, sometimes disabling, pain is common in sciatic mononeuropathy but is rare in peroneal nerve lesions around the fibular neck.
Table C3-2 Helpful Clues Suggesting That Footdrop is Not Caused by an Isolated Peroneal Nerve Lesion
Electrodiagnostic Studies
Since the sural nerve receives a major contribution from the common peroneal nerve in the popliteal fossa in 40 to 80+ of individuals, this communication may contribute to the antidromic sural SNAP, stimulating at the calf and recording at the ankle. Hence, an abnormally low amplitude sural SNAP does not automatically indicate involvement of the tibial nerve.
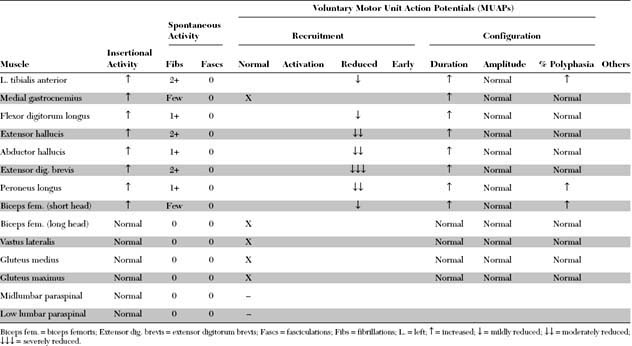
Sciatic nerve lesions, particularly when partial and mild to moderate, must be distinguished from peroneal neuropathy, lumbar plexopathy, and lumbosacral radiculopathy. Table C3-3(B) lists the electrodiagnostic features of common causes of footdrop.
On rare occasions, the common peroneal component of the sciatic nerve is the only one injured, both clinically and electrophysiologically. When this occurs, the H reflex, tibial motor NCS, and all tibial innervated muscles above and below the knee are normal. These cases are purely axonal and mimic a peroneal mononeuropathy at the fibular head. Thus, sampling the short head of the biceps femoris is mandatory in all patients with peroneal mononeuropathy, especially those due to axon loss that cannot be localized by NCS because of the lack of conduction block (or focal slowing). On clinical examination, this muscle cannot be evaluated satisfactorily in isolation. Even when it is denervated completely, its lack of function during hamstring strength testing is concealed by the normal contractions of the other three hamstring muscles, all of which are innervated by the tibial nerve.
The Piriformis Syndrome
The piriformis syndrome was first described by Yeoman in 1928 and subsequently refined by Freiberg in 1937. He described a triad of symptoms: tenderness at the sciatic notch, positive Lasègue sign and improvement with conservative therapy. Later, in 1947, Robinson coined the term “pyriformis syndrome” and set six criteria for diagnosis (Table C3-4). The syndrome became less popular after the description of nerve root compression by herniated nucleus pulposus as a common cause of sciatica. This was enhanced by the development of imaging techniques, including myelography, CT, and MRI, that could demonstrate these disc herniations and other spondylotic spine changes that encroaches on spinal roots in the lumbar canal. However, there is a recent resurgence of increasing interest in the piriformis syndrome in an attempt to explain the cause of sciatica and buttock pain in patients with no demonstrable nerve root compression on imaging studies.
* Occasionally gluteal atrophy with inferior gluteal mononeuropathy.
† Occasionally anomalous vessel or fibrous band close to the sciatic nerve.
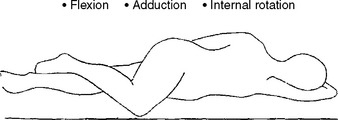
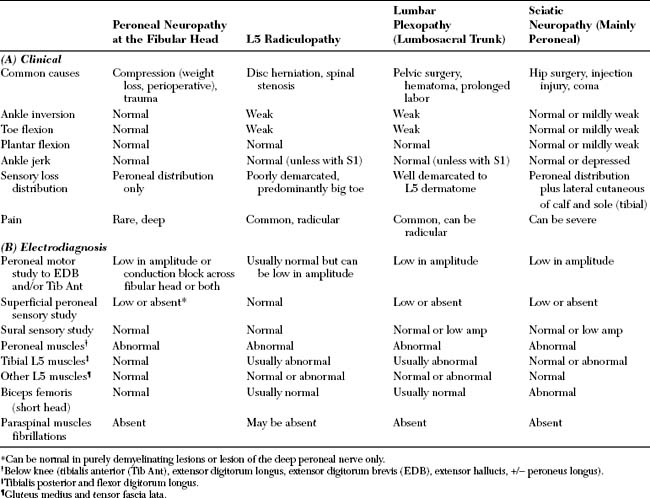
Figure C3-3 Adduction, internal rotation, and flexion (AIF) test in the diagnosis of piriformis syndrome.
The diagnosis of the piriformis syndrome is a clinical one with the EDX and imaging studies playing an important role, mostly in excluding lumbar spine disease, hip pathology, or mass lesions compressing the sciatic nerve. In almost all cases of piriformis syndrome, the EDX studies (NCS and needle EMG) are normal. Rarely, there are mild chronic denervation and reinnervation changes on needle EMG, often with normal sensory and motor NCS which renders these changes difficult to distinguish from lumbosacral radiculopathy. In these cases, the pattern of denervation is useful; the gluteus medius and tensor fascia lata, both innervated by the superior gluteal nerve, which branches from the sciatic trunk before the piriformis muscle, are normal. However, the sciatic-innervated muscles (particularly the hamstrings, gastrocnemius, and peroneal-innervated muscles) and, sometimes, the gluteus maximus (innervated by the inferior gluteal nerve) are abnormal because these nerves usually pass under the piriformis muscle (see Figure C3-2). A single study of the H reflexes done at rest and during the AIF maneuver reported an asymmetrical delay of the H reflex latency during such a procedure in patients with the piriformis syndrome. Imaging of the sciatic notch may reveal hypertrophy of the piriformis or help in identifying abnormal vessels or bands in the region of the piriformis muscle. However, these findings are also common on the asymptomatic side of patient with sciatica and in control subjects. Relief of symptoms by a CT-guided nerve block in the region of the sciatic notch is considered a diagnostic confirmation of the piriformis syndrome.
FOLLOW-UP
Although the patient’s foot weakness improved over time, she developed severe allodynia, with trophic skin changes of the foot. She responded temporarily to sympathetic block. During the next 2 years, the pain was controlled partially by a combination of a tricyclic, an anticonvulsant, and relaxation therapy.
Barton PM. Piriformis syndrome: a rational approach to management. Pain. 1991;47:345-351.
Fishman LM, Zybert PA. Electrophysiologic evidence of piriformis syndrome. Arch Phys Med Rehabil. 1992;73:359-364.
Freiberg AH, Vinke TH. Sciatica and the sacro-iliac joint. J Bone Joint Surg. 1934;16:126-136.
Hughes SS, et al. Extrapelvic compression of the sciatic nerve. J Bone Joint Surg. 1992;74A:1533-1559.
Katirji MB, Wilbourn AJ. High sciatic lesions mimicking peroneal neuropathy at the fibular head. J Neurol Sci. 1994;121:172-175.
Parziale JR, Hudgins TH, Fishman LM. The piriformis syndrome. Am J Orth. 1996;25:819-823.
Rodrigue T, Hardy RW. Diagnosis and treatment of piriformis syndrome. Neurosurg Clin N Am. 2001;12:311-319.
Schmalzried TP, Amstutz HC, Dorey FJ. Nerve palsy associated with total hip replacement. Risk factors and prognosis. J Bone Joint Surg (Am). 1991;73:1074-1080.
Stookey B. Gunshot wounds of peripheral nerves. Surg Gynecol Obstet. 1916;23:639-656.
Sunderland S. The relative susceptibility to injury of the medial and lateral popliteal divisions of the sciatic nerve. Br J Surg. 1953;41:300-302.
Sunderland S. Nerves and nerve injuries. Baltimore, MD: Williams & Wilkins, 1968.
Synek VM. The piriformis syndrome: review and case presentation. Clin Exp Neurol. 1987;23:31-37.
Weber ER, Daube JR, Coventry MB. Peripheral neuropathies associated with total hip arthroplasty. J Bone Joint Surg (Am). 1976;58:66-69.
Yeoman W. The relation of arthritis of the sacro-iliac joint to sciatica, with analysis of 100 cases. Lancet. 1928;2:1119-1122.
Yuen EC, Olney RK, So YT. Sciatic neuropathy: clinical and prognostic features in 73 patients. Neurology. 1994;44:1669-1674.
Yuen EC, So YT, Olney RK. The electrophysiologic features of sciatic neuropathy in 100 patients. Muscle Nerve. 1995;18:414-420.