Case 27
HISTORY AND PHYSICAL EXAMINATION
| Right | Left | |
|---|---|---|
| Shoulder abduction | 5/5 | 5/5 |
| Elbow flexion | 5/5 | 5/5 |
| Elbow extension | 2/5 | 5/5 |
| Pronation | 0/5 | 2/5 |
| Finger flexion (digits 1, 2, and 3) | 0/5 | 0/5 |
| Finger flexion (digits 4 and 5) | 0/5 | 4+/5 |
| Wrist flexion | 0/5 | 2/5 |
| Wrist extension | 0/5 | 5/5 |
| Finger extension | 0/5 | 4+/5 |
| Finger abduction | 0/5 | 4+/5 |
| Right | Left | |
| Hip flexion | 5/5 | 5/5 |
| Hip extension | 5/5 | 5/5 |
| Knee extension | 4+/5 | 4+/5 |
| Knee flexion | 4+/5 | 4+/5 |
| Foot dorsiflexion | 0/5 | 4−/5 |
| Toe dorsiflexion | 0/5 | 0/5 |
| Plantar flexion | 0/5 | 4/5 |
| Ankle inversion | 0/5 | 0/5 |
| Ankle eversion | 0/5 | 0/5 |
Sensation revealed a stocking glove distribution bilaterally with no clear asymmetry. There was no clear sensory loss in the left median distribution compared to the ulnar distribution on formal testing. The deep tendon reflexes were +2 at the biceps bilaterally, +2 at the left triceps, and absent at the right triceps, and absent at the brachioradialis bilaterally. The knee jerks were +1 bilaterally, while the ankle jerks were absent. Plantar responses are both flexors. Gait was not examined.
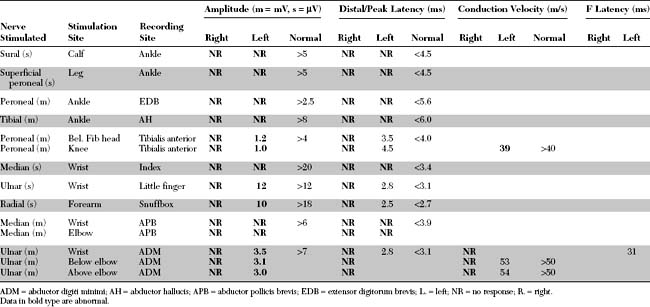
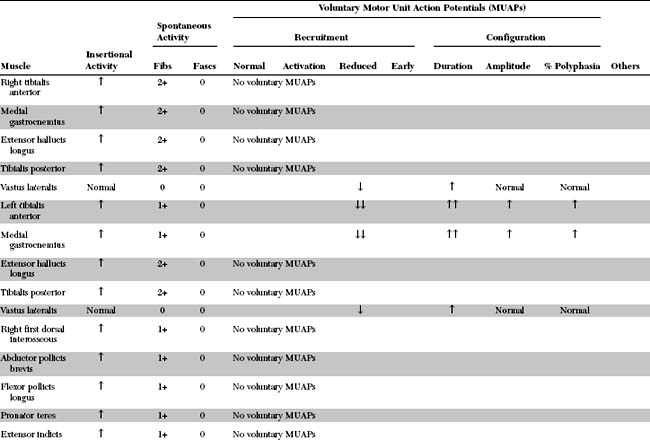
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
The relevant EDX findings in this case include:
In summary, this EDX study reveals an asymmetrical sensorimotor polyneuropathy superimposed on multiple and asymmetrical mononeuropathies. This is most consistent with an axon-loss mononeuritis multiplex becoming incompletely confluent. This case is most suggestive of a vasculitic neuropathy resulting in multiple nerve ischemia, which forms the basis for this disorder.
DISCUSSION
Definition and Classification
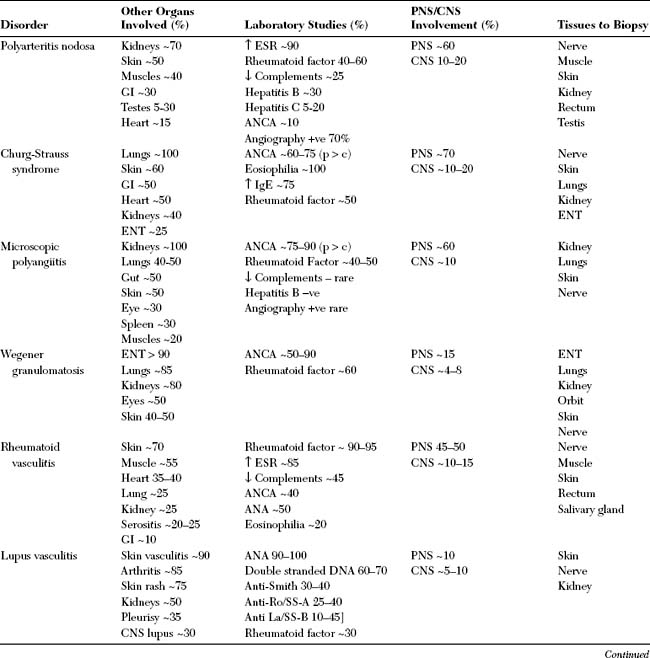
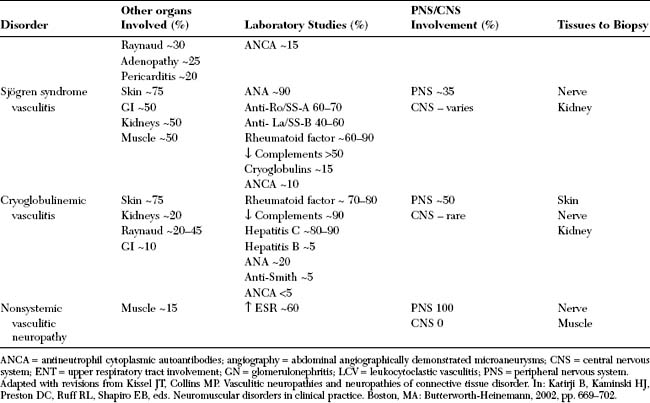
The vasculitides are group of disorders that are defined by the presence of inflammatory cells in the vessel wall with reactive damage to mural structures that compromises the lumen and leads to tissue ischemia or, occasionally, hemorrhage. They are classified based on the predominant size of the most commonly affected blood vessels (Table C27-1). The vasculitides may occur as a primary process where vasculitis is the defining feature of the illness (such as polyarteritis nodosa) or may be secondary to another underlying disease such as any connective tissue disease, infection, or drug exposure. Affected organs may become symptomatic either in isolation or in combination.
ANCA = antineutrophil cytoplasmic autoantibodies; HIV = human immunodeficiency virus.
The clinical manifestations of vasculitis are extremely variable due to the wide range of organs involved. The diagnosis is often delayed since the disorders mimic a large number of other illnesses such as atherosclerotic vascular disorders, systemic embolization, infection, and malignancy. A high index of suspicion is necessary and appropriate testing rendered as soon as possible. However, there is no single uniform method of evaluating patients suspected with vasculitis, since the work-up depends on the type of vasculitis suspected and the organs involved. Tests that are very useful in the diagnosis of vasculitis are listed in Table C27-2. Biopsy of nerve and muscle is often informative, but may occasionally not be necessary if there is histopathologic or angiographic evidence of vasculitis in other organs.
Table C27-2 Diagnostic Laboratory Tests in the Evaluation of Patients With Suspected Vasculitis in General and Vasculitic Neuropathy in Particular
Vasculitis that affects the peripheral nerves may be a feature of a systemic disorder or represent an isolated peripheral nervous system vasculitis that possesses no clinical or laboratory evidence of other organ system involvement. This isolated vasculitis is usually referred to as nonsystemic vasculitic neuropathy. Nonsystemic vasculitic neuropathy constitutes about 30 to 40% of all cases of vasculitic neuropathies, while the majority of the remaining cases are peripheral nerve manifestations of a systemic disorder, mostly polyarteritis nodosa, ANCA-associated small vessel vasculitis, or rheumatoid arthritis (Table C27-3).
Clinical Features
Mononeuropathy multiplex is defined as nerve lesions in two or more named nerves in separate parts of the body. It is usually a manifestation of vasculitis, granulomatous diseases, infiltrative neoplastic conditions, infections, diabetes, and multiple entrapment neuropathy as seen in hereditary neuropathy with liability to pressure palsy (Table C27-4). Mononeuropathy multiplex is the most specific manifestation of vasculitic neuropathy, and is often referred to as mononeuritis multiplex. The typical presentation is acute or subacute onset of multifocal mononeuropathies with weakness, sensory loss, and pain. Among peripheral nerves involved, the peroneal nerve is affected in more than three-quarters of patients presenting as mononeuritis multiplex. Other nerves affected in order of frequencies are the tibial, ulnar, radial, and median nerves. In contrast to common belief, only about half of the patients with vasculitic neuropathy present with mononeuropathy multiplex. The other half of the patients manifest with either an asymmetrical or symmetrical polyneuropathy that may be difficult to distinguish from other polyneuropathies such as metabolic or toxic polyneuropathies. It is likely that the polyneuropathy presentation of vasculitis is the result of disease progression where additional nerves are involved and become overlapped, leading to an increasingly symmetric or confluent polyneuropathy.
The diagnosis of vasculitic neuropathy often requires a high index of suspicion by relying on manifestations that are common to the vasculitides (Table C27-5). Cutaneous nerve biopsy is often necessary for final diagnosis. The yield of nerve biopsy in identifying vasculitic findings improves when nerve sampling is guided by the clinical and EDX findings and when a muscle biopsy is also obtained. Commonly biopsied nerve and muscle combinations include the sural nerve and gastrocnemius muscle or the superficial peroneal nerve and peroneus brevis muscle.
Table C27-5 Manifestations That May Suggest the Presence of a Vasculitis in Patients With Peripheral Neuropathy
Electrodiagnosis
The aim of the EDX studies in patients with suspected vasculitis is to confirm the multifocal nature of the disorder, establish what nerves are involved, and guide the treating physician to the most appropriate nerve to biopsy. Confirming the presence of axon-loss multiple mononeuropathies (mononeuritis multiplex) is the most specific finding that is highly suggestive of vasculitic neuropathy; however, other disorders such as granulomatous diseases, infiltrative neoplastic conditions, infections, or diabetes may present in a similar fashion. The EDX study also confirms the axonal loss nature of the disorder, thus eliminating other causes of predominantly demyelinating mononeuropathy multiplex such as seen with entrapment neuropathies, hereditary neuropathy with liability to pressure palsy, Lewis-Sumner syndrome, or multifocal motor neuropathy (see Table C27-4).
FOLLOW-UP
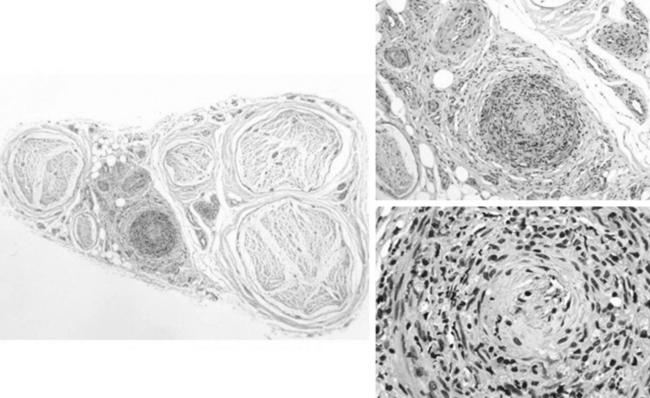
The patient underwent a sural nerve biopsy which showed prominent necrotizing vasculitis of epineurial arterioles with fibrinoid necrosis and inflammatory infiltrates in all arteriole vessel wall layers (Figure C27-1). Immunosuppressive drugs were held because of concerns about excessive hepatitis B viral replication which may cause fulminant liver failure. The patient was given three doses of intravenous methylprednisolone and was then started on a combination of lamivudine, oral corticosteroids, and plasma exchange for three months or until hepatitis B antibody seroconversion occurs.
Collins MP, Mendell JR, Periquet MI, et al. Superficial peroneal nerve/peroneus brevis muscle biopsy in vasculitic neuropathy. Neurology. 2000;55:636.
Collins MP, Periquet MI. Non-systemic vasculitic neuropathy. Curr Opin Neurol. 2004;17:587.
Davies L, Spies JM, Pollard JD, et al. Vasculitis confined to peripheral nerves. Brain. 1996;119(Pt 5):1441.
Dyck PJ, Benstead TJ, Conn DL, et al. Nonsystemic vasculitic neuropathy. Brain. 1987;110(Pt 4):843.
Guillevin L, Lhote F, Cohen P, et al. Polyarteritis nodosa related to hepatitis B virus: a prospective study with long-term observation of 41 patients. Medicine. 1995;74:238-253.
Guilleven L, et al. Short-term corticosteroids then lamivudine and plasma exchanges to treat hepatitis b virus-related polyarteritis nodosa. Arthr Care Res. 2004;51:482-487.
Jamieson PW, Guiliani MJ, Martinez AJ. Necrotizing angiopathy presenting with multifocal conduction blocks. Neurology. 1991;41:442-444.
Jennette JC, Falk RJ. Small-vessel vasculitis. N Engl J Med. 1997;337:1512.
Kissel JT, Slivka AP, Warmolts JR, et al. The clinical spectrum of necrotizing angiopathy of the peripheral nervous system. Ann Neurol. 1985;18:251-257.
Mathew L, et al. Treatment of vasculitic peripheral neuropathy: A retrospective analysis of outcome. Q J Med. 2007;100:41-51.
Olney RK. Neuropathies in connective tissue disease. Muscle Nerve. 1992;15:531.
Pagnoux C, Guillevin L. Peripheral neuropathy in systemic vasculitides. Curr Opin Rheumatol. 2005;17:41.