Case 15
HISTORY AND PHYSICAL EXAMINATION
An electrodiagnostic (EDX) examination was performed.
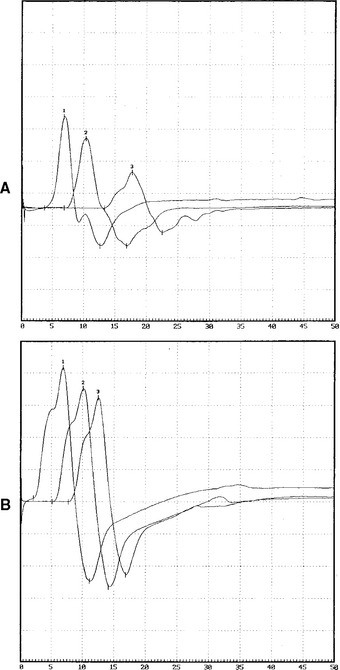
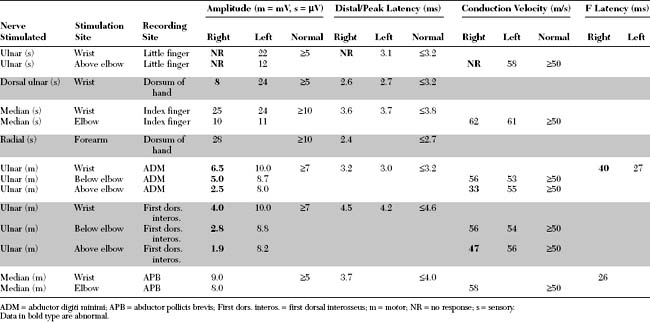
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
The EDX findings in this patient include:
DISCUSSION
Applied Anatomy
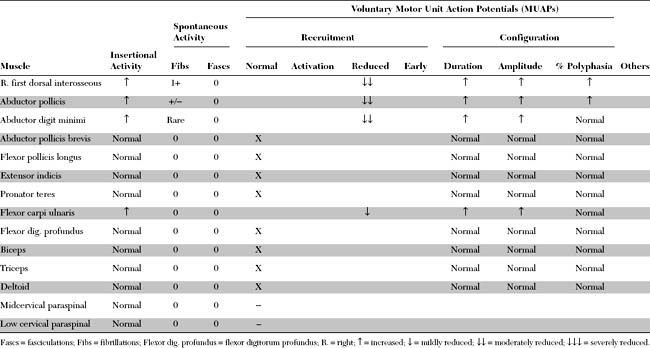
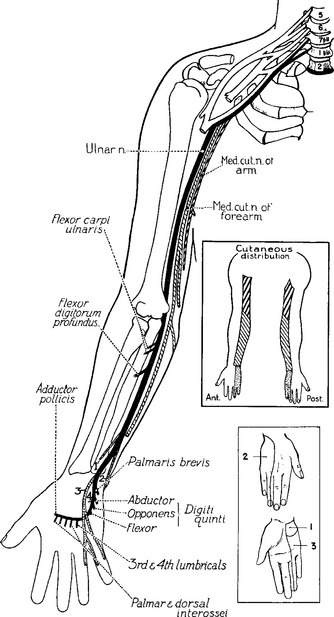
The ulnar nerve sensory and motor fibers are derived from the spinal nerves C8 and T1. Before arising from the plexus in the proximal axilla, the ulnar nerve fibers pass through the lower trunk and the medial cord of the brachial plexus (Figure C15-2). In the axilla and proximal arm, the ulnar nerve is closely related to the radial and median nerves and the brachial artery. Around the midarm, the ulnar nerve pierces the intermuscular septum and lies in close contact with the medial head of the triceps and humerus. The ulnar nerve develops no branches in the arm.
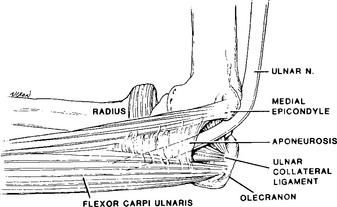
At the elbow level, and in contrast to most major human peripheral nerves, the ulnar nerve traverses the extensor, rather than the flexor, surface of the elbow joint. This renders the nerve more vulnerable to trauma around the elbow. At the elbow, the ulnar nerve crosses the ulnar groove (also called the condylar or retroepicondylar groove) behind the medial epicondyle and then passes the aponeurotic arch of the FCU to enter the cubital tunnel (Figure C15-3). This tunnel, also called the humeroulnar arcade, Osborne ligament, or arcuate arcade, is formed by the attachment of the muscle to the olecranon and medial epicondyle. Its proximal edge is variable but usually is approximately 1 cm distal to an imaginary line drawn between these two insertional points. With flexion of the elbow, the distance between the olecranon and medial epicondyle increases by approximately 1 cm, which results in tightening of the FCU aponeurosis over the nerve. In addition, the medial elbow ligament bulges, flattening the concave surface of the ulnar groove.
In the forearm, the ulnar nerve gives off its first branches. These are the motor branches to the FCU and FDP. These branches arise approximately 10 cm distal to the medial epicondyle. The ulnar nerve continues in the forearm deep to the FCU but superficial to the FDP to become superficial in the distal forearm, lying between the tendons of these two muscles. Two cutaneous sensory branches arise in the forearm, without passing through Guyon canal at the wrist, to innervate the skin in the hand. The first is the palmar ulnar cutaneous branch, which takes off at midforearm and innervates the proximal part of the ulnar border of the palm. The second is the dorsal ulnar cutaneous branch, which arises 6 to 8 cm proximal to the ulnar styloid, winds around the ulna, and innervates the dorsal surfaces of the little finger and half of the ring finger, along with the ulnar side of the dorsum of the hand (Figure C15-4).
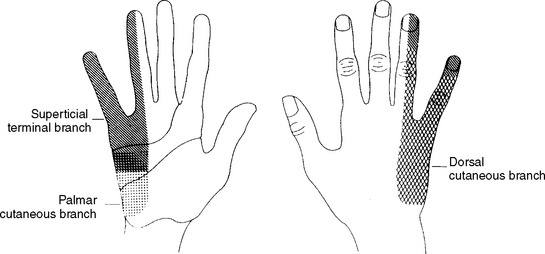
Figure C15-4 The cutaneous distribution of the three sensory branches of the ulnar nerve.
(From Stewart JD. The variable clinical manifestations of ulnar neuropathies at the elbow. J Neurol Neurosurg Psychiatry 1987;50:252–258, BMJ Publishing Group.)
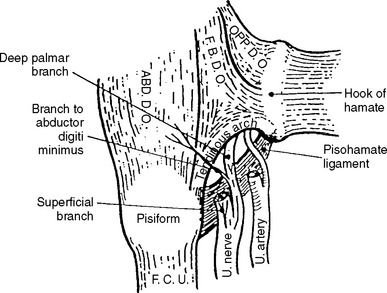
At the wrist, the ulnar nerve enters the distal ulnar tunnel (Guyon canal), where it divides into superficial (primarily sensory) and deep palmar (pure motor) branches (Figure C15-5). The superficial branch innervates the palmaris brevis muscle and the palmar aspects of digit V and half of digit IV. The deep branch innervates the hypothenar muscles, including the ADM, and travels through the palm to the dorsal and palmar interossei, the third and fourth lumbricals, the adductor pollicis, and a portion of the flexor pollicis brevis.
Figure C15-5 Anatomy of the ulnar nerve within Guyon canal at the wrist. 1 = ulnar artery, 2 = superficial branch of the ulnar nerve, 3 = hamulus, 4 = fibrous arch of the hypothenar muscles (see also Figure C15-2), 5 = pisiform, 6 = transverse carpal ligament, 7 = palmaris brevis, 8 = palmar carpal ligament.
(From Gross MS, Gelberman RH. The anatomy of the distal ulnar tunnel. Clin Orthop 1985;196:238–247, with permission.)
The flexor brevis digiti minimi (or quinti), a hypothenar muscle, has two separate attachments, at the hook of the hamate and at the pisiform bone. These musculotendinous attachments form a fibrous arch and create the superficial boundary of the pisohamate hiatus (PHH), an opening through which the deep motor branch of the ulnar nerve passes. The posterior boundary of the PHH, the pisohamate ligament, extends from the pisiform bone to the hook of the hamate (Figure C15-6). The origin of the major motor branch to the ADM is proximal to this hiatus in the majority of hands.
Clinical Features
Ulnar mononeuropathy across the elbow is a common entrapment neuropathy. It is second only to carpal tunnel syndrome in the incidence of entrapment neuropathy in general. Ulnar neuropathies across the elbow are usually caused by compression, although isolated ulnar mononeuropathy resulting from nerve infarction (such as in vasculitic neuropathy) or associated with leprosy, may occur infrequently. Causes of compressive ulnar lesions across the elbow are shown in Table C15-1. Compression of the ulnar nerve in the elbow region occurs frequently at one of the two following sites: the ulnar (condylar) groove or cubital tunnel (humeroulnar (arcuate) aponeurotic arcade). In some patients with unequivocally ulnar nerve lesions around the elbow, it is difficult to identify the exact cause, even during surgery. Most surgeons presume that the lesion is within the cubital tunnel and treat it as such.
Table C15-1 Causes of Compressive Ulnar Nerve Lesions Across the Elbow
Modified from Dimitru D. Electrodiagnostic medicine. Philadelphia, PA: Hanley and Belfus, 1995.
Patients with ulnar mononeuropathy at the elbow usually present with numbness and tingling of the little and ring fingers and variable degrees of hand weakness. Less commonly, patients present with weakness and wasting, with no clear sensory symptoms. Elbow pain, particularly around the medial epicondyle, is not uncommon. Weakness of hand with loss of dexterity and pinch strength are common symptoms in moderate entrapment. Patients may report that their little finger gets caught when trying to put their hand in their pocket (due to weakness of the third palmar interosseous muscle). Occasionally, patients may present because of intrinsic muscle hand atrophy.
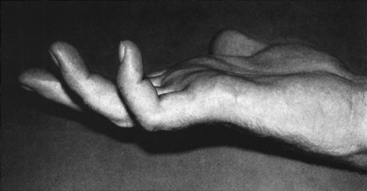
Inspection of the hand at rest in patients with moderate or severe ulnar mononeuropathy may reveal ulnar clawing. An ulnar claw hand, also called Benediction posture (Figure C15-7), is caused by: (1) hyperextension of the metacarpophalangeal joints of the little and ring fingers caused by weakness of the third and fourth lumbricals, thus allowing the extensor digitorum communis to exert an unopposed pull; and (2) flexion of the interphalangeal joints of the same fingers resulting from an inherent flexion muscle tone of the FDP and superficialis muscles, whose tendons are stretched over the metacarpophalangeal joints because of the above hyperextension. In ulnar lesions, this clawing is more noticeable when the FDP is spared. The Wartenberg sign is recognized as abduction of the little finger at rest due to weakness of the third palmar interosseous muscle.
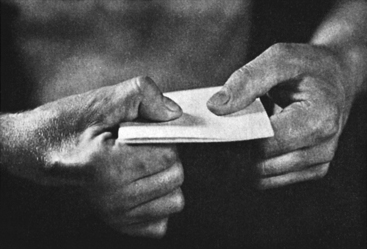
Weakness of ulnar-innervated muscles in the hand predominates in ulnar nerve lesions across the elbow; the forearm muscles are affected less often. Weakness of the FDP to the fourth and fifth digits is assessed by flexion of the distal interphalangeal joints of these digits. Positive Froment sign is helpful in the clinical diagnosis of ulnar neuropathy because it shows the weakness of the adductor pollicis (ulnar muscle) and the normal flexor pollicis longus (median muscle), both of which are innervated by the C8/T1 roots via the lower plexus. This sign is assessed by asking the patient to grasp a piece of paper between the thumb and second digit. Because of weakness of the adductor pollicis, the patient uses the flexor pollicis longus as a substitute in an attempt to keep the paper from sliding (Figure C15-8).
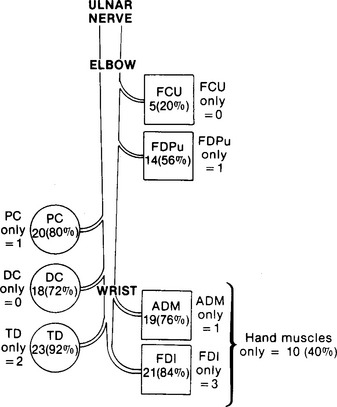
Many patients with ulnar nerve lesions at the elbow have variable weakness and numbness distally. This is explained by the propensity for partial focal lesions to affect fascicles differentially within that nerve. This fascicular phenomenon is common in ulnar nerve lesions across the elbow and is demonstrated in Figure C15-9. Atrophy of ulnar muscles in the hand is common with long-standing lesions and is most apparent in the interossei, particularly the first dorsal interosseous (see Figure C15-8).
Treatment of ulnar neuropathy at the elbow may be conservative or surgical. Identification and reversal of the cause of repetitive compression is essential. Many patients with mild symptoms and signs who demonstrate evidence of slowing or conduction block on nerve conduction studies may be treated successfully using conservative approaches (Table C15-2). Patients with substantial weakness, particularly when progressive or associated with evidence of axonal loss or ongoing denervation, benefit from surgery. There is no clear consensus on the optimal surgical procedure. Simple decompression of the cubital tunnel may be ideal for patients with cubital tunnel syndrome, while medial epicondylectomy or submuscular transposition of the ulnar nerve are more suitable for compression at the ulnar groove. Submuscular transposition has a higher success rate but is a more complex surgery and carries a risk of nerve devascularization and ischemia.
Table C15-2 Conservative Measures in the Treatment of Mild Ulnar Neuropathy at the Elbow
|
While sitting, the arm should not be crossed, but the elbow should be straightened and the arm rested on thigh
|
Adapted with revision from Dellon AL, Hament W, Gittelshon A. Nonoperative management of cubital tunnel syndrome: an 8-year prospective study. Neurology 1993;43:1673–1677.
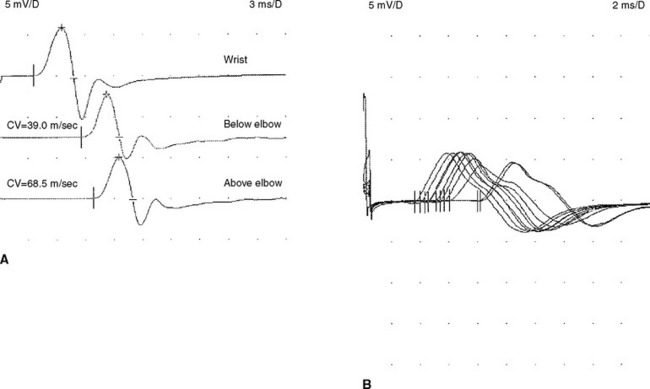
Electrodiagnosis
Although it is the second most common site of peripheral nerve entrapment, electrodiagnostic localization of ulnar mononeuropathy at the elbow is controversial and challenging because of anatomic, technical, and pathophysiologic factors. The pathophysiologic process of ulnar nerve lesions at the elbow is extremely variable. In contrast to carpal tunnel syndrome, in which slowing across the carpal tunnel is the hallmark of the disease, ulnar mononeuropathy across the elbow may present with focal slowing, conduction block, differential slowing, axon loss, or, more frequently, any combination of the above. Although acute lesions generally present with conduction block and/or axon loss, and chronic lesions usually present with focal slowing and/or axon loss, many ulnar lesions across the elbow do not comply with this rule.
Sensory NCS
Motor NCS
Ulnar Motor Conduction Studies, Recording the Hypothenar Muscles (ADM)
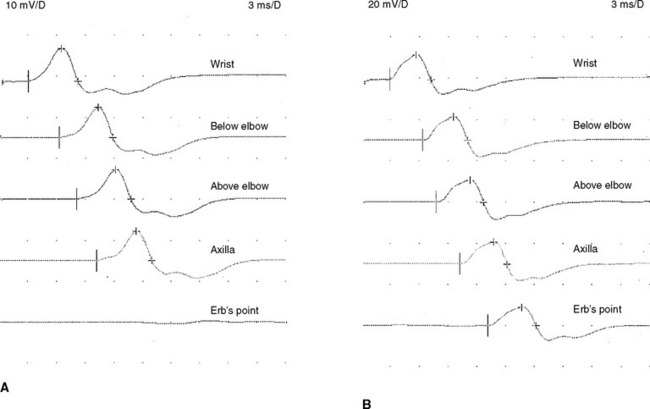
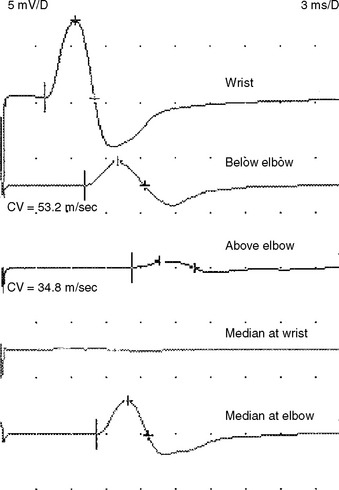
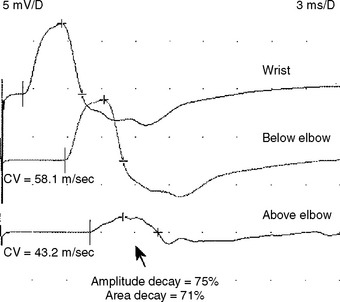
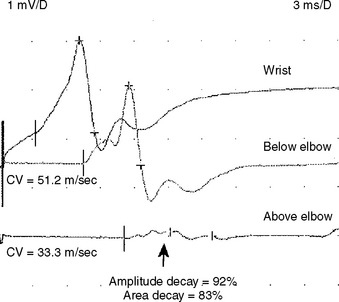
This is a routine motor conduction study that is performed in many laboratories. The nerve is stimulated at the wrist, below the elbow, and above the elbow. Stimulation at the axilla also is sometimes useful because it allows comparison of two segments (forearm and arm) to the across-elbow segment and also evaluate for rare ulnar nerve lesions in the arm. Erb point (supraclavicular) stimulation is also occasionally helpful in excluding a high ulnar nerve lesion (Figure C15-10). The conduction abnormalities observed across the elbow are:
Needle EMG
Needle examination is useful in confirming an ulnar nerve lesion and in excluding a C8/T1 root lesion or a lower brachial plexopathy. It is important to establish that the C8/T1 muscles innervated by the median nerve (such as the abductor pollicis brevis or the flexor pollicis longus) and radial nerve (such as the extensor indicis proprius) are normal. In addition, in purely axonal lesions of the ulnar nerve, needle EMG is crucial in localizing the lesion to a particular segment of the nerve, which it does by establishing that muscles distal to the lesion are abnormal and muscles proximal to it are normal. Unfortunately, there are limitations to the accurate localization by needle EMG in patients with axonal ulnar neuropathies:
Electrodiagnostic Controversies
In Which Position Should the Elbow Be Placed During Performance of Ulnar Nerve Conduction Studies (Extension or Degree of Flexion)?
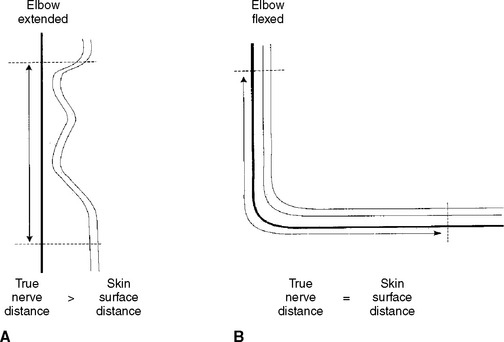
Hence, surface measurements of the ulnar nerve while the elbow is extended do not reflect the true extent of the underlying nerve. In fact, the distance measured over the skin is shorter than the true length of the nerve. Hence, the conduction velocity is spuriously slowed because the impulses travel longer distances than can be estimated on skin measurement (Figure C15-14). On the other hand, surface measurements of the ulnar nerve while the elbow is hypreflexed more than 90° may be longer than the true nerve length (due to potential nerve subluxation) resulting in artifactually fast conduction velocity.
How Much Slowing of Motor Fibers Across the Elbow is Needed to Make a Diagnosis of Ulnar Mononeuropathy?
Measurement of conduction velocities is subject to error. This error is largely the result of inaccurate measurement of distance between the sites of stimulation. Because the error may involve many millimeters, using short distances between stimulation sites results in a relatively large percentage of error in the measurement of distance and, hence, in the assessment of conduction velocity. In other words, conduction velocities of longer nerve segments are more accurate and subject to less human error than velocities of shorter segments.
Based on this principle, the following is recommended:
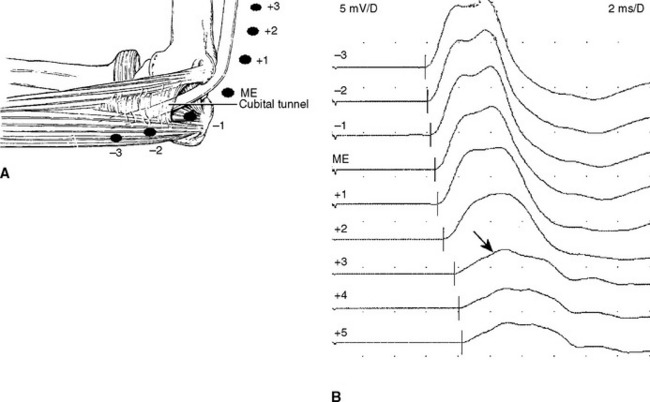
Are Short Segment Incremental Studies (“Inching”) Required for Accurate Diagnosis?
The stimulation site is moved progressively along the nerve across the elbow, in several equal steps (usually 1–2 cm), between the below and above elbow (over about 6–8 cm span) and CMAP amplitude, latency or morphology are recorded. This study should be done meticulously since it is subject to measurement error and volume conduction. An abrupt change in CMAP amplitude, morphology or latency (>0.5 ms) is noted (Figure C15-15). The short increment technique could also be used to point localize lesions in other segments of the ulnar nerve, such as the arm or forearm (Figure C15-16).
Bielawski M, Hallet M. Position of the elbow in determination of abnormal motor conduction of the ulnar nerve across the elbow. Muscle Nerve. 1989;12:803-809.
Campbell WW, et al. Intraoperative electroneurography: management of ulnar neuropathy at the elbow. Muscle Nerve. 1988;11:75-81.
Campbell WW, Pridgeon RM, Sahni KS. Short segment incremental studies in the evaluation of ulnar neuropathy at the elbow. Muscle Nerve. 1992;15:1050-1054.
Checkles NS, Russakov AD, Piero DL. Ulnar nerve conduction velocity: effect of elbow position on measurement. Arch Phys Med Rehabil. 1971;53:362-365.
Dellon AL, Hament W, Gittelshon A. Nonoperative management of cubital tunnel syndrome: an 8-year prospective study. Neurology. 1993;43:1673-1677.
Eisen A, Danon J. The mild cubital tunnel syndrome. Neurology. 1974;24:608-613.
Jabley ME, Wallace WH, Heckler FR. Internal topography of the major nerves of the forearm and hand. J Hand Surg. 1980;5:1-21.
Katirji MB, Katirji PM. Proximal ulnar mononeuropathy caused by conduction block at Erb’s point. Arch Neurol. 1988;45:460-461.
Kincaid JC. The electrodiagnosis of ulnar neuropathy at the elbow. Muscle Nerve. 1988;11:1005-1015.
Kothari MJ, Preston DC. Comparison of the flexed and extended elbow positions in localizing ulnar neuropathy at the elbow. Muscle Nerve. 1995;18:336-340.
Miller RG. The cubital tunnel syndrome: diagnosis and precise localization. Ann Neurol. 1979;6:56-59.
Payan J. Electrophysiological localization of ulnar nerve lesions. J Neurol Neurosurg Psychiatry. 1969;32:208-220.
Peterson AR, et al. Variations in dorsomedial hand innervation. Electrodiagnostic implications. Arch Neurol. 1992;49:870-873.
Stewart JD. The variable clinical manifestations of ulnar neuropathies at the elbow. J Neurol Neurosurg Psychiatry. 1987;50:252-258.
Ventakesh S, Kothari MJ, Preston DC. The limitations of the dorsal ulnar cutaneous sensory response in patients with ulnar neuropathy at the elbow. Muscle Nerve. 1995;18:345-347.