Case 10
HISTORY AND PHYSICAL EXAMINATION
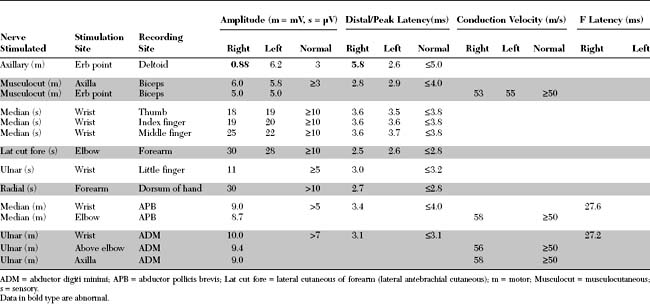
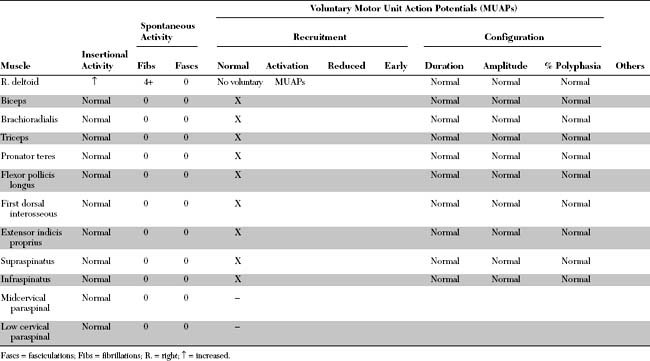
Please now review the Nerve Conduction Studies and Needle EMG tables.
QUESTIONS
EDX FINDINGS AND INTERPRETATION OF DATA
Pertinent electrodiagnostic (EDX) findings include:
DISCUSSION
Applied Anatomy
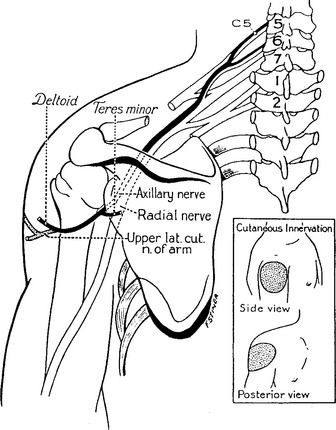
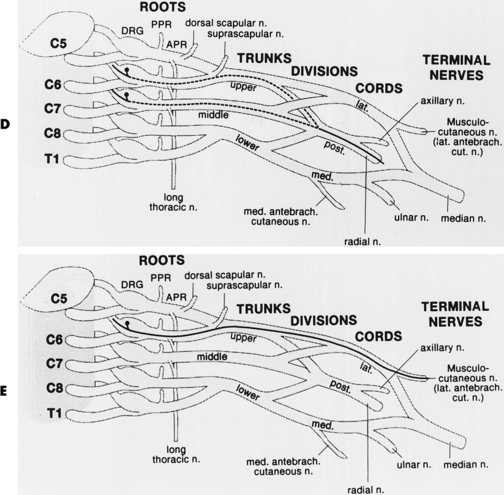
The axillary nerve (also called the circumflex nerve) arises from the posterior cord of the brachial plexus near the shoulder joint. Its fibers originate from the C5 and C6 roots and travel through the upper trunk to the posterior cord. The nerve has a very short path. It courses posteriorly, inferior to the shoulder joint where it traverses the quadrilateral space, bounded superiorly by the teres minor muscle, inferiorly by the teres major muscle, medially by the long head of the triceps muscle, and laterally by the humeral neck. At this point, the axillary nerve gives branches to the teres minor muscle and then it curves around the neck of the humerus, under the deltoid muscle. There, it terminates into two branches, one posterior and the other, anterior; both innervate the deltoid muscle. The upper lateral cutaneous nerve of the arm, which innervates the skin overlying the deltoid muscle (Figure C10-1), originates from the posterior branch.
Clinical Features
Injury of the axillary nerve is associated most often with shoulder trauma or surgery around the shoulder joint; or, it may be a component of idiopathic brachial plexitis (Table C10-1). Axillary mononeuropathy is a common complication of shoulder dislocation, especially among the elderly. Also, the axillary nerve may be injured individually during an episode of acute brachial plexitis (neuralgic amyotrophy); alternatively, this may occur with the suprascapular, long thoracic, or anterior interosseous nerve (refer to Case 16).
Axillary nerve lesion causes weakness of shoulder abduction and extension, and a patch of sensory loss and paresthesias over the lateral deltoid (see Figure C10-1). Deltoid atrophy becomes predominant later resulting in flattening of the shoulder. Weakness of the teres minor is seldom clinically significant since the supraspinatus muscle performs similar functions.
In general, the prognosis for axillary nerve lesions is relatively good because of the short distance required for reinnervation to the target muscle (deltoid). Unfortunately, adhesive capsulitis of the shoulder develop in many patients, which, by itself, has a negative effect on final functional outcome. Thus, an aggressive stretching and range-of-motion program should be initiated as soon after diagnosis as possible.
Electrodiagnosis
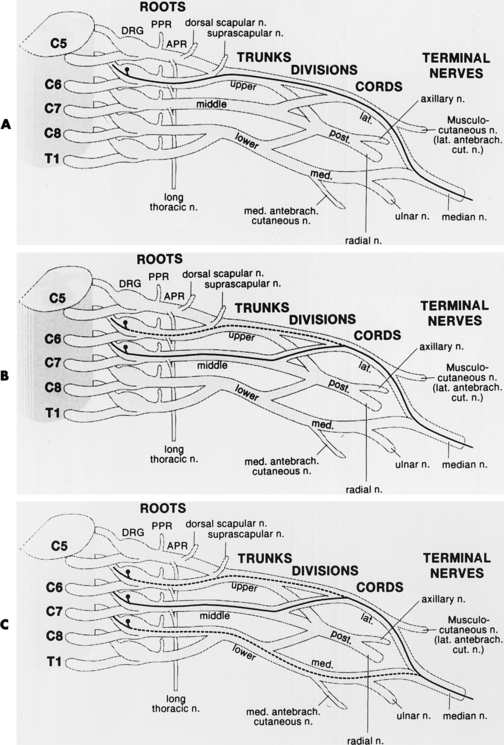
The main purpose of the EDX studies in patients with suspected axillary mononeuropathy is to confirm that the abnormalities are restricted to the axillary nerve distribution and to exclude a brachial plexopathy, particularly of the upper trunk or posterior cord, and a cervical radiculopathy, mostly of the C5 and C6 roots. The sensory nerve conduction studies are extremely useful in these cases because they usually are abnormal in relatively mild plexus lesions, assisting in the diagnosis of brachial plexopathy that sometimes could not be detected on clinical evaluation. Among various studies in the upper extremity, the following SNAPs should be normal in isolated axillary nerve lesions (Figure C10-2):
In cases of suspected axillary nerve lesions, the role of motor nerve conduction studies is twofold. First, they confirm what is seen on the needle EMG, such as normal musculocutaneous CMAP with normal needle EMG of the biceps muscle. The second, and perhaps more important, role is prognostic; the CMAP amplitude is the best semiquantitative and objective measure of axonal loss. Thus theoretically, and extrapolating from other proximal nerves for which only a single site of stimulation is possible (such as the femoral or facial nerve), a low axillary CMAP, stimulating Erb point and recording the deltoid muscle, is consistent with a severe axonal loss lesion and a protracted recovery. However, Erb point stimulation is supraclavicular and is likely to result in widespread stimulation of the brachial plexus, including the posterior cord and the proximal axillary nerve. Hence, it is conceivable that a demyelinative axillary nerve lesion around the head of the humerus (i.e., distal to the stimulation point) may result in distal conduction block, thus leading to a low axillary CMAP. Therefore, caution should be used when making definitive prognostication in cases of axillary nerve lesion.
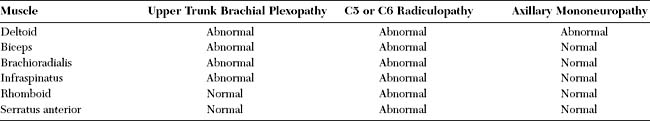
On needle EMG, certain muscles are essential for accurate localization of the lesion (Table C10-2). These muscles are listed in order of their importance:
Berry H, Bril V. Axillary nerve palsy following blunt trauma to the shoulder region: a clinical and electrophysiological review. J Neurol Neurosurg Psychiatry. 1982;45:1027-1032.
Blom S, Dahlback LO. Nerve injuries in dislocations of the shoulder joint and fractures of the neck of the humerus. J Bone Joint Surg. 1965;47B:9-22.
Cahill BR, Palmer RE. Quadrilateral space syndrome. J hand Surg. 1983;8:65.
Ferrante MA, Wilbourn AJ. The utility of various sensory nerve conduction responses in assessing brachial plexopathies. Muscle Nerve. 1995;18:879-889.
Francel TJ, Dellon AL, Campbell JN. Quadrilateral space syndrome: diagnosis and operative decompression technique. Plast Reconstr Surg. 1991;87:911-916.
Liveson JA. Nerve lesions associated with shoulder dislocation: an electrodiagnostic study of 11 cases. J Neurol Neurosurg Psychiatry. 1984;47:742-744.
Paladini D, Dellantonio R, Cinti A, et al. Axillary neuropathy in volleyball players: Report of two cases and literature review. J Neurol Neurosurg Psychiatry. 1996;60:345-347.