76 Carpal tunnel syndrome
Salient features
History
• Ask the patient about nocturnal pain (commonest cause of hand pain at night). Often the pain wakes up and shakes the hand to ameliorate symptoms: ‘wake and shake’.
• Pain, tingling, burning, numbness or some combination of these symptoms on the palmar aspect of the thumb, index finger, middle finger and radial half of the ring finger (no such symptoms affect the fifth finger even on detailed questioning).
• History of oral contraceptives, rheumatoid arthritis, myxoedema, acrogmegaly, chronic renal failure or sarcoidosis.
• Take a family history (abnormally small size of carpal tunnel runs in families).
Examination
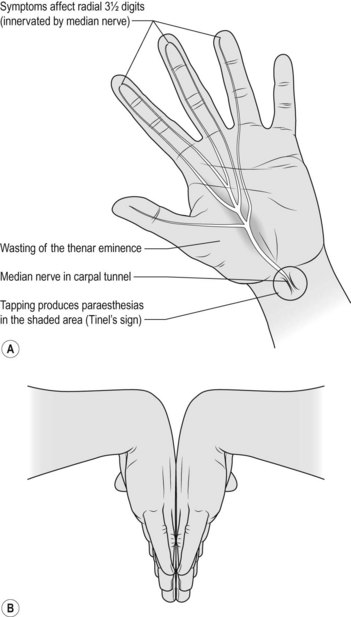
• Wasting of the thenar eminence (Fig. 76.1A)
• Weakness of flexion, abduction and opposition of thumb
• Diminished sensation over lateral three and half fingers
• Ask the patient, ‘What do you actually do with your hand(s) when symptoms are at their worst?’ If the patient makes flicking movement of the wrist and hand, similar to that employed in shaking down a clinical thermometer (the ‘flick sign’), this had both a sensitivity and a specificity >90% in one study (J Neurol Neurosurg Psychiatry 1984;47:870–2).
• Look carefully for scar of previous surgery (hidden by the crease of the wrist).
• Percuss over the course of the median nerve in the forearm: patient may experience tingling (Tinel’s sign (Fig. 76.1A). The sensitivity of Tinel’s sign ranges from 25 to 60%, although its specificity is higher (67 to 87%).
• Ask the patient to hyperextend the wrist maximally for 1 min; this may bring on symptoms (dysaesthesia over the thumb and lateral two and half fingers): Phalen’s test (Fig. 76.1B).
Questions
How would you treat this condition?
• Diuretics, NSAIDs, steroids have been studied in small trials but were not efficacious
• Wrist splint in neutral posture rather than in extension (80% report that a wrist splint alleviates symptoms, usually within days). Splinting also reduces sensory latency, suggesting that it may alter the underlying course of carpal tunnel syndrome. Ultrasound treatment (BMJ 1998;316:731–5)
• Local steroid injection should be given proximal to the carpal tunnel (not into the tunnel because it may damage the nerve) (BMJ 1999;319:884–6)
• Alternative therapies. Data are limited: acupuncture, yoga-based stretching, strengthening and relaxation (greater improvement in grip strength and reduction of pain than with splinting), chiropractic therapy (was as effective for pain as splints and medication).
Advanced-level questions
Mention a few clinical diagnostic tests
• Wrist extension test: the patient is asked to extend the wrists for 1 min; this should produce numbness or tingling in the distribution of the median nerve.
• Phalen’s test: the patient is asked to keep both hands with the wrist in complete palmar flexion for 1 min; this produces numbness or tingling in the distribution of the median nerve (Fig. 76.1B). Sensitivity and specificity ranges widely from 40 to 80%.
• Tourniquet test: the symptoms are produced when the BP cuff is inflated above the systolic pressure.
• Pressure test: pressure placed where the median nerve leaves the carpal tunnel causes pain.
• Luthy’s sign: is regarded as positive if the skinfold between the thumb and index finger does not close tightly around a bottle or cup because of thumb abduction paresis.
• Durkan’s test: direct pressure over the carpal tunnel (the carpal compression test); this is more sensitive and specific than Tinel’s and Phalen’s signs.
Mention other entrapment neuropathies
• Meralgia paraesthetica: lateral cutaneous nerve of the thigh trapped under the inguinal ligament
• Elbow tunnel syndrome: ulnar nerve trapped in the cubital tunnel (p. 290)
• Common peroneal nerve trapped at the head of the fibula (p. 294)
• Morton’s metatarsalgia: trapped medial and lateral plantar nerves causing pain between third and fourth toes
• Tarsal tunnel syndrome: trapped posterior tibial nerve
• Suprascapular nerve trapped in the spinoglenoid notch
• Radial nerve trapped in the humeral groove
• Anterior interosseous nerve trapped between the heads of the pronator muscle.