Carpal Tunnel Release
Linda de Haas, Diane Coker and Kyle Coker
Carpal tunnel syndrome (CTS) continues to be one of the most significant upper extremity (UE) injuries, with more than 500,000 procedures performed each year.1 It results from compression of the median nerve as it crosses the wrist and is characterized by numbness, tingling, pain, and complaints of weakness in the hand. The symptoms of CTS can range from mild to severe. They may have far-reaching effects on a person’s job, hobbies, and activities of daily living (ADL).2
CTS is also the most common entrapment neuropathy of the UE.1 Paget described the complex of symptoms caused by median nerve entrapment at the wrist in 1854, and Moersch gave the syndrome its name in 1938. Brain, Wright, and Wilkerson published the first series of carpal tunnel releases by division of the transverse carpal ligament (TCL) in 1947. Since that time, a number of variations of this procedure have been developed, all of which involve division of the TCL.
The prevalence in the United States of self-reported CTS is approximately 1 to 3 cases per 1000 subjects per year in the adult (working and nonworking) population.3–5 CTS affects people during their most productive years. Its prevalence peaks between the ages of 35 and 44 years for both men and women. Women are three times more likely to be affected than men.6
The Bureau of Labor Statistics tracks CTS under work-related musculoskeletal disorders. In 2008, 3.1% of 384,480 musculoskeletal disorders were CTS cases.7,8 These data demonstrate the importance of clinicians fully understanding the prevention and treatment of CTS.
Surgical Indications and Considerations
Causes
The onset of CTS can be classified into two categories: (1) acute and (2) chronic. Acute CTS is associated with a traumatic event, such as blunt trauma to the wrist, wrist fracture, infections, vascular disorders, rheumatologic disorders, hemorrhagic problems, burns, and high pressure injection injuries.1 These traumas produce a sudden and sustained increase in interstitial pressure within the carpal tunnel, resulting in a median nerve conduction block from intracompartmental and intraneural ischemia. This form of CTS is a medical emergency and requires immediate carpal tunnel decompression.
Chronic CTS is the result of an insidious rise of the interstitial pressure in the carpal tunnel and is classified as early, intermediate, or advanced. Patients with early CTS experience mild, intermittent symptoms that have been present less than 1 year. Intermediate CTS is characterized by more constant symptoms, including numbness and paresthesia, usually worse at night, with little or no atrophy of the thenar muscles. Surgery performed at this time uncovers a nerve that has undergone chronic changes, including epineural and intrafascicular edema. If decompression is performed at this time, then the neural changes are frequently reversible, although night symptoms may take a year to resolve. Advanced CTS is characterized by progressive paresthesia, atrophy of the thenar muscles, and pinch and grip weakness. Even after a successful surgical decompression, the chronic changes in the median nerve may be permanent.9
CTS can affect anyone, although females tend to have a higher incidence. Medical and ergonomic histories have been identified as independent risk factors in developing CTS, although controversy exists as to the contribution of work activities to the development of CTS.10–12 Recent studies have looked at obesity as defined by body mass index; other biologic factors, such as genetics or structural make-up; and wrist anthropometrics as possible contributing factors.13–18 There are some strong associations between CTS and age, gender, and female hormonal status as seen, for instance, during menopause or pregnancy.12 Pregnancy can precipitate CTS by causing edema around the structures traversing the carpal canal. During pregnancy the symptoms of CTS tend to occur in the last trimester, secondary to fluid retention. The condition usually resolves within 6 to 12 weeks after delivery.9
CTS can also be associated with a number of other disease processes, including thyroid disease, rheumatoid arthritis, and diabetes, as well as with various anatomic anomalies such as a persistent median artery, median nerve variations, extramuscle bellies, and extratendinous slips.15,18–20 Tumors and ganglions of the wrist, although rare, can precipitate CTS as the lesion occupies space within the carpal canal.21 Wrist trauma can cause CTS because of the resulting edema and hematoma surrounding the median nerve. Variations in lumbrical origin, length, or width can increase carpal tunnel pressure as dynamic lumbrical incursion into the CT can occur during finger flexion movements.22
From the ergonomic side, CTS is often seen in patients who perform repetitive activities in their work or hobbies. One study of computer workers demonstrated that the angle of wrist extension (more than 20°) was associated with developing CTS.23
The diagnosis of CTS can usually be made based on a thorough history and careful physical examination. In cases in which the diagnosis is uncertain, electrodiagnostic studies can be helpful in either confirming or ruling out the disorder.24
In general, patients who are diagnosed with early stage CTS are initially treated without surgery. Nonsteroidal antiinflammatory drugs, although often prescribed, have not been shown to be effective in any controlled study to date25,26 In some patients with recently developed CTS (less than 1 year), local injection of steroid medication into the carpal canal or oral steroids can significantly, although temporarily, reduce the symptoms of median nerve compression (Fig. 12-1). It has not been shown that a steroid injection can actually alter the progression of the disorder.5,27

The best evidence-based conservative physical therapy treatments for CTS include splinting, deep pulsed ultrasound (US), nerve-gliding exercises, carpal bone mobilization, and yoga.26,28 Splinting the patient’s wrist can be very helpful in controlling nighttime pain symptoms.29 The wrist is splinted in a neutral position that maximizes the carpal tunnel space30 and minimizes the carpal tunnel pressure.31 The splint is chosen based on the patient’s needs and comfort. The metal stay of a prefabricated wrist splint is easily replaced with a custom-molded thermoplastic stay to position the wrist in neutral. A positive Berger test (the patient holds a full fist position for 30 to 40 seconds, with a positive test reproducing paresthesia) result would suggest that the metacarpal phalangeal joints should also be immobilized in the splint, as the lumbricals can descend into the carpal tunnel with active finger flexion and cause further space compromise of the carpal tunnel contents.10,32 All patients should sleep in their splints. Patients who have constant or activity-induced paresthesia may also wear their splints during the day.30 When such conservative measures fail to resolve symptoms, surgery is indicated.
Classic CTS symptoms include the following5:
1 Numbness and tingling in the median nerve distribution in the hand
Sensory changes are commonly the first symptoms noted. The patient typically reports paresthesia and numbness of the digits served by the sensory branches of the median nerve and in the tips of the thumb, index finger, middle finger, and radial half of the ring finger, although both sides of the ring finger can be affected. Sensory symptoms may also be restricted to a single digit, or even involve the entire hand.1 Sensibility in the thenar eminence is usually unaffected as this area is innervated by the palmar cutaneous branch of the median nerve, which branches proximal to the carpal tunnel, entering the hand volar to the TCL.
The onset of pain is most often the primary reason a person with chronic CTS seeks medical attention. The pain associated with CTS tends to begin in the latter aspects of the early and then into the intermediate stages. The patient complains of an intermittent, vague, dull aching in the wrist or forearm. Less common is pain radiating to the elbow and even the shoulder. Night pain is a common complaint most likely caused by congestion of the venous system during sleep.33 Neurologic muscle weakness associated with CTS occurs late in the disease process. In advanced cases, atrophy of the thenar musculature can be seen. The unlucky patient with symptoms progressed to this state is at high risk for permanent nerve damage and may require a tendon transfer to substitute for the loss of palmar abduction.
The clinician must be able to visualize the anatomic structures that make up the carpal tunnel. The carpal canal is bounded by the TCL volarly, the scaphoid tuberosity and the trapezium radially, the hook of the hamate and the pisiform ulnarly, and the volar radiocarpal ligament and volar ligamentous extensions between the carpal bones dorsally.19,34 The carpal canal is traversed by the median nerve, the four flexor digitorum profundus tendons, the four flexor digitorum superficialis tendons, the flexor pollicis longus tendon, and the surrounding synovial membranes. Any condition that causes enlargement of the contents of the carpal canal (such as inflammation or edema) or occupies space within the canal (such as a tumor or hematoma) compresses the median nerve. This occurs because the structures that make up the carpal canal are relatively inelastic and do not expand as the contents of the canal enlarge. The resulting pressure compromises circulation within the substance of the nerve, leading to nerve ischemia, which in turn leads to the symptoms and signs seen in CTS.
Surgical Procedure
The surgical treatment for carpal tunnel dates back to the 1940s.35,36
The condition could be thought of as a compartment syndrome affecting the median nerve within the carpal canal.37 As such, the intracompartmental pressure surrounding the median nerve exceeds the local capillary pressure, thus preventing blood flow. Surgical treatment is directed at increasing the volume of the carpal canal and reducing the pressure within. Most methods rely on the release of the TCL, which forms the soft tissue roof of the carpal canal. There are three general surgical approaches to the release of the TCL.
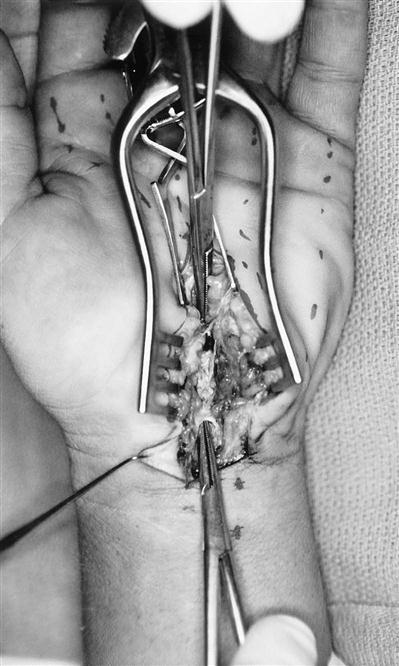
The first surgical approach is the classic open technique in which an incision starting in the proximal third of the palm is made that extends proximally along the axis of the ring metacarpal to the wrist flexion crease (Fig. 12-2). Keeping to the ulnar side of the median nerve reduces the risk of injury to its motor branch, which will occasionally arise on the ulnar side of the nerve and cross superficially over to the thenar muscles. The incision is then continued proximally across the volar flexion creases in a zigzag fashion to avoid hypertrophic scarring. The incision is kept to the ulnar side of the palmaris longus tendon to avoid injury to the palmar cutaneous nerve. This incision gives complete exposure to the area of constriction (Figs. 12-3 and 12-4). The thick portion of the TCL between the trapezium and scaphoid tubercle radially and the hook of the hamate and pisiform on the ulnar side is divided under direct vision and extended to the superficial palmar arch distally and approximately 4 to 5 cm proximal to the volar flexion crease of the wrist. The advantage of this approach is the direct exposure to the median nerve along its entire length within the suspected area of constriction. In addition, the contents of the carpal canal can be thoroughly explored for masses, excessive synovial tissues, and bone spurs. If indicated, synovectomy or tenolysis can be performed. Disadvantages of this approach include an increased incidence of pillar pain, prolonged healing, prolonged weakness of grip because of scar tenderness, and destabilization of the flexor tendons and the pulley effect provided by an intact TCL.
The second and less invasive procedure could be referred to as a limited open palm technique. By this method a smaller incision is made in the palm following the same course as the palm segment of the classic open technique but avoids crossing the volar flexion crease of the wrist. The distal portion of the TCL is incised under direct vision and retractors are used to complete the division proximal to the volar flexion crease. With more specialized instruments and retractors, the palmar incision can be kept quite small. The advantage of this procedure is to minimize injury to the overlying skin and cutaneous nerves, thus reducing the chance of a tender scar. Since there is less destabilization of the flexor tendons, there is less potential for prolonged weakness of grip. The disadvantage of this technique is the limited exposure and visualization of potential pathologic conditions, such as space occupying lesions within or just proximal to the carpal canal.
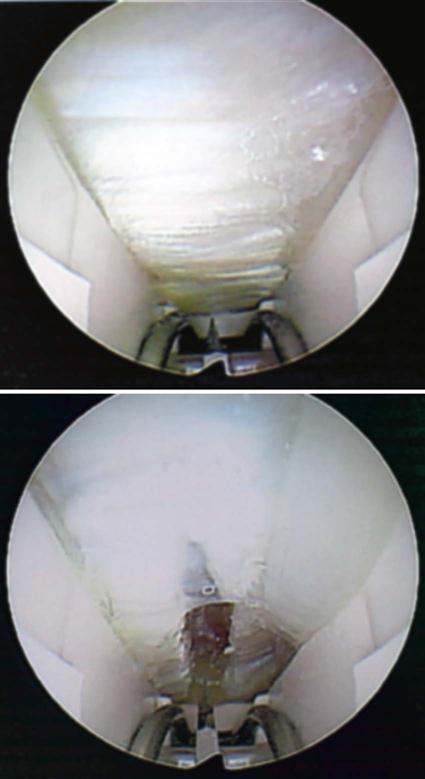
The third technique is endoscopic carpal tunnel release (ECTR). There are several variations of this technique including one or two portals—either one proximal to the wrist crease, one in the mid palm, or both. ECTR was introduced by Okutsu and Chow in 1989.38,39 Chow’s technique, which has become popular in the United States, employed two portals to pass the endoscope and instruments under the TCL. Agee later introduced a single proximal portal technique that employed an integrated instrument incorporating the scope and surgical knife.40 There have since been minor modifications in technique and instrumentation for Chow’s technique, but the principles remain the same.
The endoscopic techniques were developed to minimize recovery and absence from work. To this end the concept has been successful. Many studies have reported this in both the workers compensation population and the nonwork related groups.39,40 Several studies comparing recovery rates between open carpal tunnel release and ECTR indicate that the advantages of ECTR diminish over time and there is very little difference at 3 months follow-up (Fig. 12-5).41
Surgery for carpal tunnel is not risk free.42 Complications include:
• Injury to the median nerve including the motor branch
• Injury to digital nerves; most often the common digital nerve to the third web space
• Complex regional pain syndrome
Lesser complications that usually resolve with time include: hematoma, wound dehiscence, pillar pain, and weakness of grip.
The literature reports an overall higher rate of all of these complications with the endoscopic technique by a factor of two to four times. However, most of these were reports from the early and late 1990s, and although the specific techniques were rarely reported, they were probably referring to the earlier two portal techniques. There have not been any direct comparisons between the two portal and single portal techniques that compare complication rates.
Postoperatively, most surgeons will splint wrists following the open technique to allow soft tissue healing and to position the wrist in extension to prevent bowstringing of the flexor tendons, which might push the medial nerve into the area of the healing TCL. Although this was the early rationale for postoperative splinting, more recent studies have shown splinting to be less important than previously believed.43 Wrists are often not splinted following endoscopic release, although time must still be allowed for internal healing.
Pillar Pain
Pillar pain is cited as a common postoperative complication and is a frequent reason to send the patient for postoperative therapy.44 It is described as pain over either the thenar or hypothenar eminence or both. These areas correspond to the scaphoid tubercle and hook of the hamate distally, and trapezium and pisiform proximally, forming a rectangle. The three thenar muscles are anchored to the scaphoid tubercle and trapezium, and the three hypothenar muscles are anchored to the hook of the hamate and pisiform. The TCL ties the two columns together and acts as a pulley to guide the nine flexor tendons. The cause is still unclear, possibly because several different symptoms have been called pillar pain. It is unclear if the pain represents deep scar tissue, injury to sensory nerves in the TCL, loss of stability of the attached muscles, or alteration of the carpal arch. Whatever the cause, there appears to be a lowered incidence with ECTR compared with limited open releases, which further improve on the full open incision. In all cases the pain tends to resolve in 3 months.44,45
Failed Carpal Tunnel Surgery
Carpal tunnel surgery is highly successful in relieving the symptoms caused by compression on the median nerve at the wrist. Failures can be grouped into two categories: recurrent symptoms and residual symptoms. Both can result from incomplete or inadequate release of the TCL, progression of the underlying disease, or misdiagnosis.
Whereas the TCL is seen in its entirety in the open carpal tunnel release, it may not be when doing the ECTR. In fact, in the case of the open technique, the TCL is allowed to open widely as much as 1 to 2 cm. The limited incision technique opens to a lesser degree and the ECTR by only a few millimeters. This latter technique is usually enough to decompress the median nerve, but there have been reports of both early and late failures that were relieved by reoperation using the open procedure.
Early return of symptoms following initial relief might be caused by tight bandages or excessive stretch on the nerve from improper splinting, hematoma, or excessive scar tissue.
Late recurrences can also result from incomplete or even full open release if the underlying condition continues to progress. Enlarging masses, trauma, edema, inflammatory conditions causing synovitis, or simply the aging process might be to blame.
Residual symptoms following carpal tunnel surgery are common, but in one of the author’s experience, true recurrences and failed surgeries are very rare. Although symptoms of CTS vary depending on the individual, age, and duration of symptoms, the most common symptom of carpal tunnel is numbness in the distribution of the median nerve, which is worse at night. This is usually confirmed by evidence of significant slowing of the nerve conduction through the carpal canal. When patients with residual symptoms are properly questioned, they usually recall that they did in fact have relief of their nocturnal numbness following release of the TCL. This indicates a successful treatment of their CTS; however, they may still be dissatisfied with the result if they still have symptoms that brought them to the physician in the first place. These symptoms might include arm pain, arm numbness and tingling, shooting pains into various parts of the arm and hands, and weakness. The symptoms might be reproducible when attempting to perform specific activities, giving rise to the notion that their condition is a repetitive motion injury. In the experience of the authors of this chapter, the vast majority of these patients are no longer suffering from CTS but rather have a more proximal nerve entrapment. There are several potential points of entrapment of the median nerve at the elbow, including pronator syndrome. If cervical radiculopathy can be ruled out, the problem may be attributed to compression at the level of the brachial plexus, the so-called thoracic outlet syndrome. This diagnosis is often made by exclusion and then treated with a trial of therapy to address the thoracic outlet. Within a few weeks the patient will often notice a significant decrease in pain and an increase in strength.46,47
Therapy Guidelines for Rehabilitation
Postoperative Rehabilitation
The frequency and duration of treatment is highly variable after a carpal tunnel release. In most cases minimal therapy is required, with key contributions to postoperative care being wound/scar management and proper instructions in exercises to enhance tendon gliding, obtain full active range of motion (AROM), and minimize edema. The patient may need guidance on ergonomics and other principles to facilitate full return to work or other activities.10 All patients referred to therapy are instructed in a home exercise program appropriate to the phase of recovery and their individual needs.
In general, patients tend to do quite well after carpal tunnel release. However, because the extent of the damage to the median nerve cannot fully be known before surgery, predicting the exact outcome of carpal tunnel release is difficult. Patients with mild to moderate symptoms can expect full recovery of sensation and resolution of the numbness and tingling caused by entrapment of the nerve. Patients with more advanced disease who have significant sensibility loss and muscle weakness usually achieve significant improvement of their condition. Patients with muscle atrophy can expect a halt to progression of muscle wasting and in some cases can regain muscle mass.
The recovery of the median nerve directly relates to the success of the surgery. Ultrasonography postoperatively may be helpful in identifying the initial beneficial morphologic changes. Nerve conduction studies could take as long as 3 to 6 months to change.48 Patients must understand that they may have some element of incisional pain after surgery, which can last as long as 3 to 6 months. They must also be informed that they will temporarily lose some strength in the hand, which usually improves after 3 to 6 months.
Postoperative Evaluation
In general, patients may be referred to therapy anywhere from 1 to 3 weeks postoperatively. The timing of the first visit will dictate which tests are appropriate to perform and which should be deferred until a later time. The initial evaluation after carpal tunnel release includes the following:
After 3 weeks postoperatively, in addition to the above measurements, the evaluation can include:
The patient’s history is obtained by patient interview. Information to be noted in the history includes age, gender, hand dominance, cause of CTS, type and date of the carpal tunnel release, occupation, avocational interests, onset and description of symptoms before surgery, and notes regarding whether symptoms were unilateral or bilateral. The patient should be screened for medical or systemic problems that might contribute to the persistence of symptoms.
The patient is asked to quantify the pain on a scale from 0 (representing no pain) to 10 (indicating severe pain requiring medical attention). The patient is asked to rate the pain both at rest and with use. The quality of the patient’s pain is obtained by documenting the descriptive terms the patient uses when discussing the symptoms.49
Edema of the hand is recorded either by volumetric circumferential or figure of eight measurements. If edema is profuse throughout the hand, then volumetric measurements can be taken provided that stitches have been removed and the patient has no open wounds. The volumetric assessment should be administered following the American Society of Hand Therapists (ASHT) guidelines. If edema is minimal or the stitches have not yet been removed, then circumferential measurements recorded in centimeters should be obtained at the distal wrist crease and the distal palmar crease (DPC). The figure of eight method for assessing hand edema has been shown to be as reliable and valid as the volumetric method, and may be easier to perform in a busy clinic than the volumetric method.50
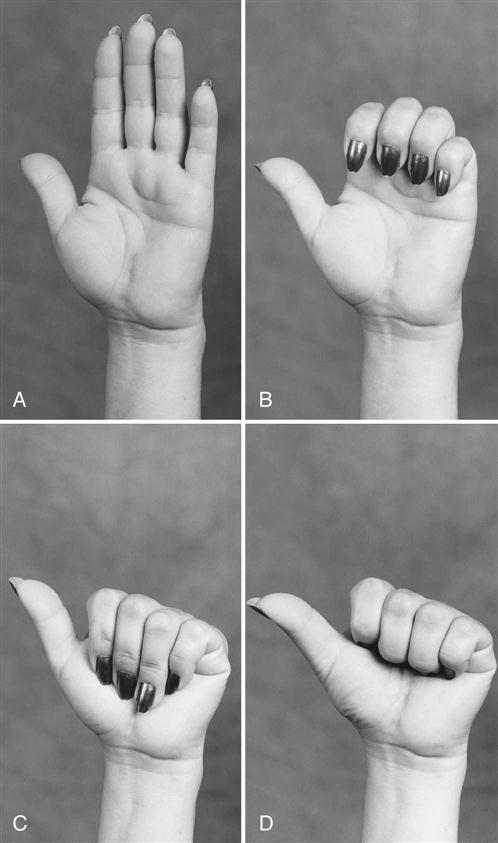
AROM measurements are obtained using a goniometer for the wrist and forearm. Individual finger AROM measurements may not be necessary when motion limitations are minimal. A global measurement of finger flexibility is obtained by measuring composite finger flexion to the DPC. The distance from the middle of the pulp of a finger to the DPC is measured in centimeters for each finger. Functional thumb opposition is recorded as the ability to oppose the thumb to each fingertip, and full composite flexion/opposition as the ability to touch the thumb to the DPC of the small finger. Full motion is recorded as “zero,” and lack of full motion as a negative number.
![]() To prevent bowstringing (i.e., subluxing, or anterior displacement, of the flexor tendons through the healing TCL), simultaneous wrist/finger flexion measurements should be deferred until 3 weeks after an open incision surgery. As mentioned, bowstringing may be more of a concern with open procedures than with endoscopic procedures.51
To prevent bowstringing (i.e., subluxing, or anterior displacement, of the flexor tendons through the healing TCL), simultaneous wrist/finger flexion measurements should be deferred until 3 weeks after an open incision surgery. As mentioned, bowstringing may be more of a concern with open procedures than with endoscopic procedures.51
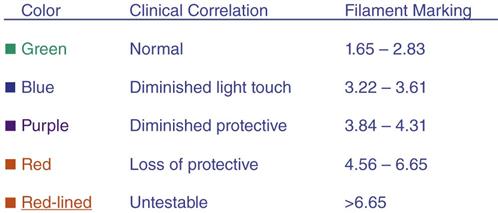
“Sensibility testing is the evaluation of the ability to feel or perceive a stimulus applied to an area.”52 Sensibility assessment is completed using the Semmes-Weinstein pressure aesthesiometer kit (a five filament kit is adequate). This type of sensory test is a pressure threshold test. The patient is seated comfortably for testing with the forearm supinated and the hand supported on a towel roll. The therapist should occlude the patient’s vision during the test and instruct the patient to report when a finger is stimulated and which finger feels the stimulus. The volar fingertips and thumb pulp are tested starting with the 2.83 monofilament. “Each monofilament is applied perpendicular to the skin for 1.5 seconds and lifted for 1.5 seconds.”52 The therapist should apply monofilaments 2.83 and 3.61 three times to the same spot, and apply monofilaments 4.31 through 6.65 once. The lowest-numbered monofilament felt for each digit should be recorded on the evaluation form.52 Full hand mapping is rarely required after a carpal tunnel release.
“Two point discrimination values are most often normal in CTS, and if they are abnormal it indicates advanced disease.”53,54 The therapist should complete two-point discrimination testing only if the patient demonstrates significant deficits on the Semmes-Weinstein Monofilament Test. Two point discrimination is an innervation density test.53 The difference between the pressure threshold test and an innervation density test is the sensitivity of the pressure threshold test to gradual loss or improvement in nerve function versus an all-or-none response on an innervation density test.
The surgical incision or scar is evaluated for its stage of healing. The therapist should document whether the scar is raised or flat, tough or soft, mobile or adherent. The color of the scar also is noted. Some authors have written that one of the principle predictors of good outcomes and successful back to work status is minimal scar tenderness.44,55 Therapeutic interventions by physical therapists that include scar assessment and management techniques are necessary, therefore, to ensure a flat, nonadherent, nonpainful scar.
The patient’s present functional status can be documented in the areas of grooming, dressing, bathing, cooking, home care, work, avocational activities, and driving. Standardized self-administered outcome measurement tools that can be employed include the DASH, the Michigan Hand Outcomes Questionnaire, and the Boston Carpal Tunnel Scales, which includes the symptoms severity scale and functional status scale. Each of these scales takes only about 5 minutes to complete. These scales have been validated for use in CTS and even reported as more responsive to clinical improvements than grip, MMT, or sensory testing by monofilaments or two-point discrimination (Fig. 12-6).56–58
If the patient is 3 weeks postoperation, grip strength is recorded using a dynamometer with the handle positioned at the second setting59,60 per American Society of Surgery of the Hand (ASSH) and ASHT guidelines.
To perform a grip test, the patient should be “seated with the shoulder adducted and neutrally rotated, elbow flexed to 90°, forearm in neutral position” and unsupported.61,62 The therapist may support the dynamometer to prevent dropping; however, the dynamometer should not be allowed to rest on the table. The therapist should document three grip measurements, alternating the right and left hands,63 unless repetitive grasping of the dynamometer would increase the discomfort in the patient’s hand. Several authors have published normal values for grip strength but because of the high standard deviation11 and inconsistencies in the studies, “comparison of grip scores to the contralateral extremity or longitudinal comparison to earlier values for each patient is recommended by ASSH and ASHT.”60,62,64
Three types of pinch can be recorded using a pinch meter. Finger positioning for a three-point pinch is performed with the index and middle finger on the top of the pinch meter and the thumb on the bottom. Lateral pinch positioning is performed with the pinch meter held between the radial side of the index finger and the thumb on the top of the meter. Tip pinch is thumb pulp against index finger pulp. Tip pinch has been reported as a better outcome measure of strength for postoperative carpal tunnel release than grip or lateral pinch.65 ![]() Early forceful pinch, however, is not recommended until 3 weeks after surgery.
Early forceful pinch, however, is not recommended until 3 weeks after surgery.
Finger dexterity can be evaluated with various instruments such as the nine hole peg test, Jebsen-Taylor hand function test, O’Connor finger dexterity test, modified Moberg pick-up test, or the Minnesota rate of manipulation test. These tests have been standardized and normative data have been established for comparison purposes.
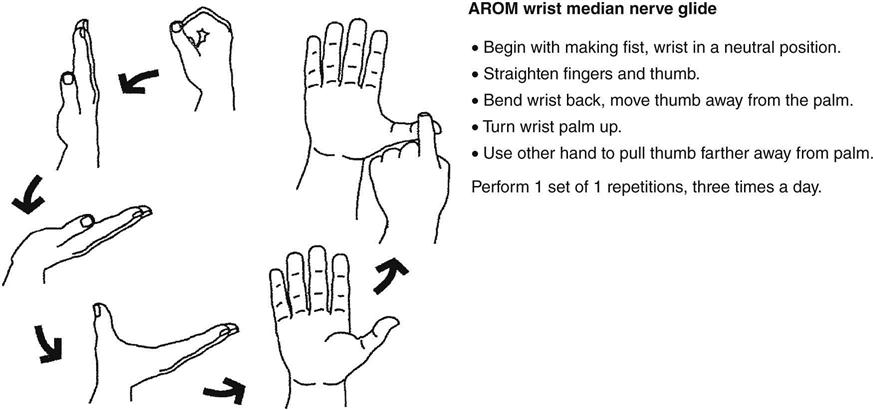
Upper-limb tension testing of the median nerve is appropriate to determine whether the patient has restrictions in nerve gliding. Limited studies have shown a decrease in the symptoms during conservative treatment of CTS,66,67 and neural gliding is recommended not only to minimize the potential of adhesions on the nerve, but to increase range of motion (ROM) and decrease pain.68 Local median nerve gliding at the wrist can be addressed as well (Fig. 12-7). Readers are referred to other authors such as Butler, Coppieter, and Elvey for more detailed information on neural tensioning principles and techniques.
The hand can be assessed for any atrophy of the thenar eminence, after which MMT of the upper quarter can be performed. As mentioned previously, care is taken to avoid undue stress on the flexor tendons until at least 3 weeks after surgery. ![]() In assessing the function of the median nerve, the “abductor pollicis brevis is the muscle of choice for clinical assessment because it is superficial, and is solely innervated by the median nerve.”69,70
In assessing the function of the median nerve, the “abductor pollicis brevis is the muscle of choice for clinical assessment because it is superficial, and is solely innervated by the median nerve.”69,70
Postoperative Splinting
The value of postoperative splinting has been debated, and physical therapists should engage the patient in a decision on the need for splint use.43,71 Neutral wrist splinting31,72 can be helpful for controlling tension at the wound site/scar, helping the patient to avoid simultaneous wrist/finger flexion, as well as functioning as a simple reminder for the patient to minimize use of the operative hand. However, according to one study,43 there was less pain and scar tenderness but a greater delay in return to full activity level and less strength in patients who wore a splint postoperatively for 2 weeks compared with those who did not wear a splint.
Phase I (Inflammatory Phase)
TIME: Day 1 to 3 weeks after surgery
Treatment of the patient after carpal tunnel release is based on the phases of wound healing and tissue response to stress. Treatment is directed toward patient education, edema control, scar modification, restoration of ROM, and strength and full return of hand function.
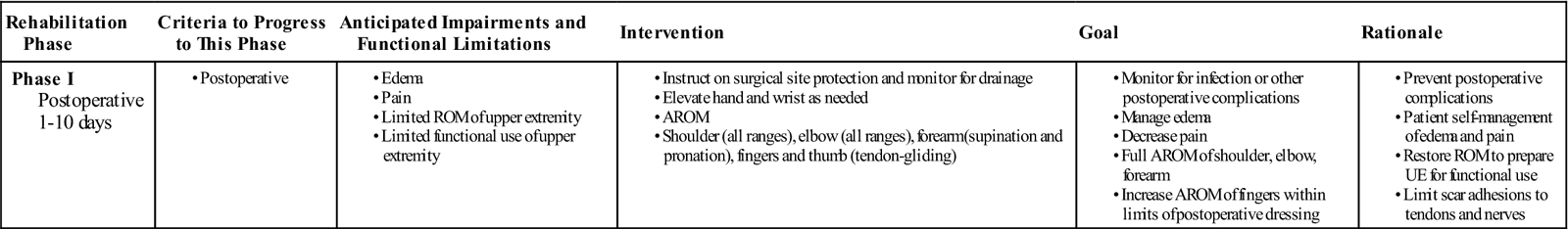
GOALS: Promote wound healing, maintain tendon excursion, and prevent median nerve from adhering to tendon, increase digit ROM to within normal limits (WNL) and maintain proximal ROM, decrease pain, decrease edema, independence with ADL, independence with home program (Table 12-1)
TABLE 12-1
< ?comst?>
| Rehabilitation Phase | Criteria to Progress to This Phase | Anticipated Impairments and Functional Limitations | Intervention | Goal | Rationale |
| Phase I Postoperative 1-10 days |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
A light postoperative dressing is usually worn for 7 to 10 days after surgery. The patient should be instructed to elevate the hand and move fingers frequently to help decrease edema. Exercises during phase I consist of AROM to the shoulder, elbow, and digits. The patient is instructed in tendon-gliding exercises (Fig. 12-8) to prevent adhesion of the tendons through the carpal tunnel and to help decrease edema.73 The patient is also instructed in nerve glides, which include gentle wrist flexion and extension with the UE held in a relaxed position at side of body. Many patients are not referred to formal therapy and, after instruction, can perform exercises as a home program and are instructed to use the hand as tolerated.
Phase Ia
TIME: 10 days to 3 weeks postoperative
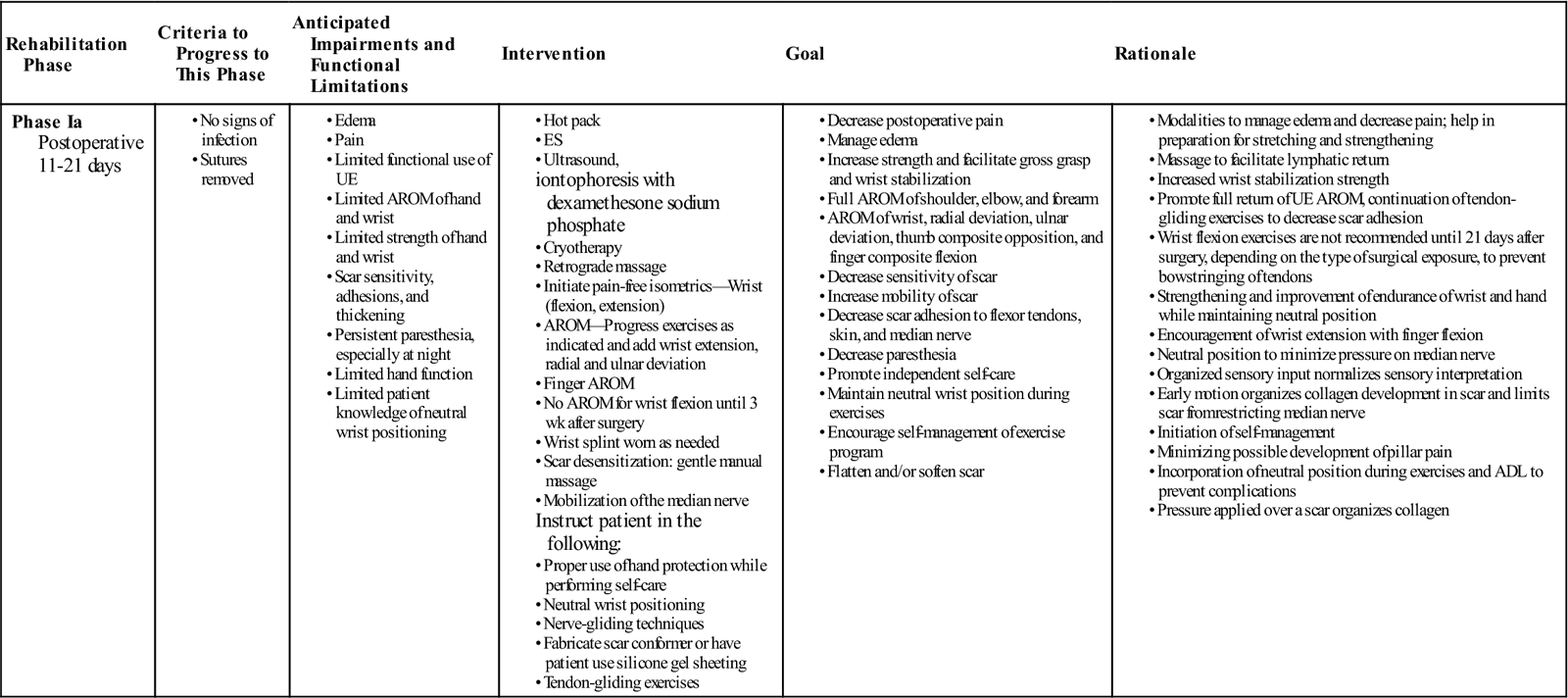
GOALS: Promote scar remodeling, decrease hypersensitivity and pain, increase wrist ROM to WNL, begin to increase hand strength, independence in home exercise program (Table 12-2)
TABLE 12-2
< ?comst?>
| Rehabilitation Phase | Criteria to Progress to This Phase | Anticipated Impairments and Functional Limitations | Intervention | Goal | Rationale |
| Phase Ia Postoperative 11-21 days |
|
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Within 48 hours of suture removal, scar mobilization techniques may be initiated. Begin with a light scar massage with lotion and progress to a more vigorous soft tissue mobilization as tolerated.
AROM should include composite flexion and extension of the digits, isolated blocking to the FDS and FDP, full median nerve glides, and continued tendon-gliding exercises. Seven to 10 repetitions are performed three to four times per day. At this time, ![]() composite flexion of the wrist and fingers is generally avoided until 21 days postoperation to prevent bowstringing of the tendons through the healing carpal ligament. Some patients may be referred for formal hand therapy for pain relief, scar desensitization, hand strengthening, and to help facilitate return to maximum activity (see Table 12-2). Modalities may be used to decrease pain and edema, to increase elasticity of tissues, and to promote tissue healing.74 Moist heat may be used for pain control before exercise and to prepare tissues for soft tissue mobilization. The modalities of pulsed US, iontophoresis,74 and high-voltage galvanic stimulation74 are helpful in reducing the local swelling and pain experienced by patients after carpal tunnel release. Phonophoresis has not been shown to be any more effective than US alone for pain relief.56
composite flexion of the wrist and fingers is generally avoided until 21 days postoperation to prevent bowstringing of the tendons through the healing carpal ligament. Some patients may be referred for formal hand therapy for pain relief, scar desensitization, hand strengthening, and to help facilitate return to maximum activity (see Table 12-2). Modalities may be used to decrease pain and edema, to increase elasticity of tissues, and to promote tissue healing.74 Moist heat may be used for pain control before exercise and to prepare tissues for soft tissue mobilization. The modalities of pulsed US, iontophoresis,74 and high-voltage galvanic stimulation74 are helpful in reducing the local swelling and pain experienced by patients after carpal tunnel release. Phonophoresis has not been shown to be any more effective than US alone for pain relief.56
Iontophoresis with dexamethasone sodium phosphate may be used for decreasing local edema about the incision site. However, the incision must be completely healed and able to tolerate the stimulation.
Cryotherapy, if tolerated, may be administered after exercises for 10 minutes to help in managing edema and pain. Light retrograde massage also may facilitate lymphatic return. Patients with persistent edema may benefit from wearing a compression glove in conjunction with other edema-controlling modalities. The compression glove should be worn almost continuously at first, and then worn only at night as edema decreases. As discussed, splinting is declining in favor during postoperative treatment because of the deleterious effects of immobilization on joint mobility and muscle length. Splinting may be appropriate for patients who experience nighttime pain associated with flexed postures of the wrist and may also be used to provide rest to inflamed tissues.
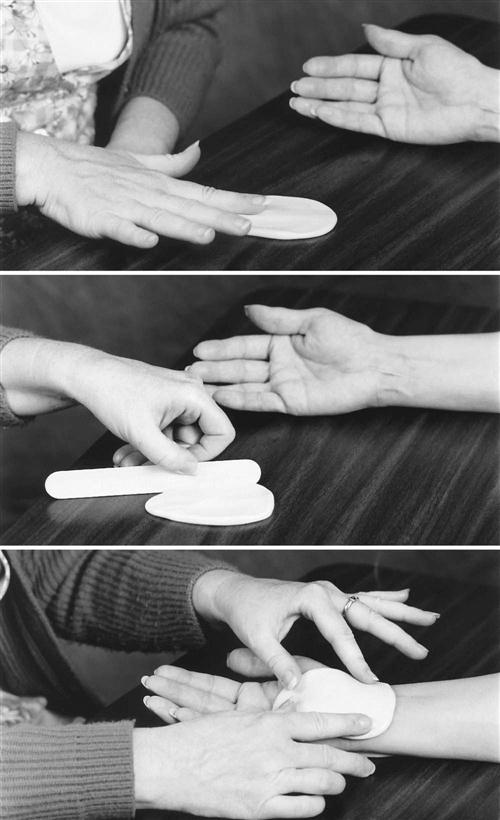
The therapist should initiate scar desensitization when the surgical incision is closed. The desensitization process is initiated gently and can be performed in many ways. These methods include manual self-massage of the scar, immersion in tubs of textured particles, and rubbing the scar with different textures. When performing scar desensitization, the scar is initially rubbed lightly with soft fabrics; treatment progresses by using deeper pressure and coarser textures. Scar massage is initiated with minimal force, and the force is increased as the incision increases in tensile strength (Fig. 12-9). Scar massage can be done for 1 to 3 minutes, five times per day.
Limiting the development of scar adhesion to tendons, skin, and nerves is another important aspect of scar management after carpal tunnel release surgery. Tendon-gliding exercises are continued to move the flexor tendons differentially in the carpal tunnel. Nerve-gliding techniques are helpful in maintaining mobility of the median nerve after a carpal tunnel release.75 The home program for median nerve gliding begins with the arm held at the side of the body, the elbow extended, and the forearm and wrist in a neutral position. The patient is instructed to extend the wrist from a neutral position in a gliding motion. The patient should be cautioned not to be overzealous with these exercises and to inform the therapist if symptoms increase.
When the incision is fully closed, a scar conformer can be fabricated from silicone elastomers or cut from silicone gel sheets (Fig. 12-10). Because the scar conformer works by applying pressure over the scar, it needs to be held firmly in place. Silicone sheeting does not need pressure wrapping, because the intervention is simply direct contact with scar tissue. Silicone gel sheeting is recommended for nightly application, for 8 to 10 hours per day. The therapist can use a self-adherent wrap such as Coban to secure the conformer or gel sheeting over the scar. The patient should be instructed not to wrap the scar conformer or sheeting too tightly with the Coban because tight wrapping will cause edema and pain in the hand. An explanation should be given to the patient regarding the purpose and importance of scar management techniques for at least 3 months. The patient should wash the scar conformer or silicone sheeting as needed to prevent skin irritation and replace the scar conformer/sheeting if it becomes worn or soiled. The patient should observe the skin closely for signs of skin maceration or heat rash. If these problems occur, then the patient should stop using the scar conformer or silicone and inform the therapist. Decreasing the amount of wear time or placing a light gauze or tissue between the scar elastomer pad and the skin may control skin maceration and heat rash.
After 3 weeks, the therapist can also initiate isometric strengthening exercises for wrist extension and flexion. Wrist isometrics are performed in a neutral wrist position.76 The patient applies enough resistance with the opposite hand to create a muscle contraction, which is held for 5 seconds without increasing pain. The exercises can be progressed by increasing resistance and repetitions. Instruction on ways to maintain a neutral wrist position during functional use of the hand is emphasized with paper crunch activity and isometric strengthening exercises. This education is further emphasized with ergonomic instruction in phase II.
The patient should be encouraged to use the affected hand for self-care while avoiding wrist flexion, forceful repetitive grip, and lifting more than 3 lb. Tasks that require forceful grip, such as vacuuming, handling wet laundry, putting fitted sheets on the bed, yard work, tool use, lifting, and pushing, should be avoided for 6 to 8 weeks to allow complete healing.
Phase II (Proliferation Phase)
TIME: 3 to 6 weeks after surgery
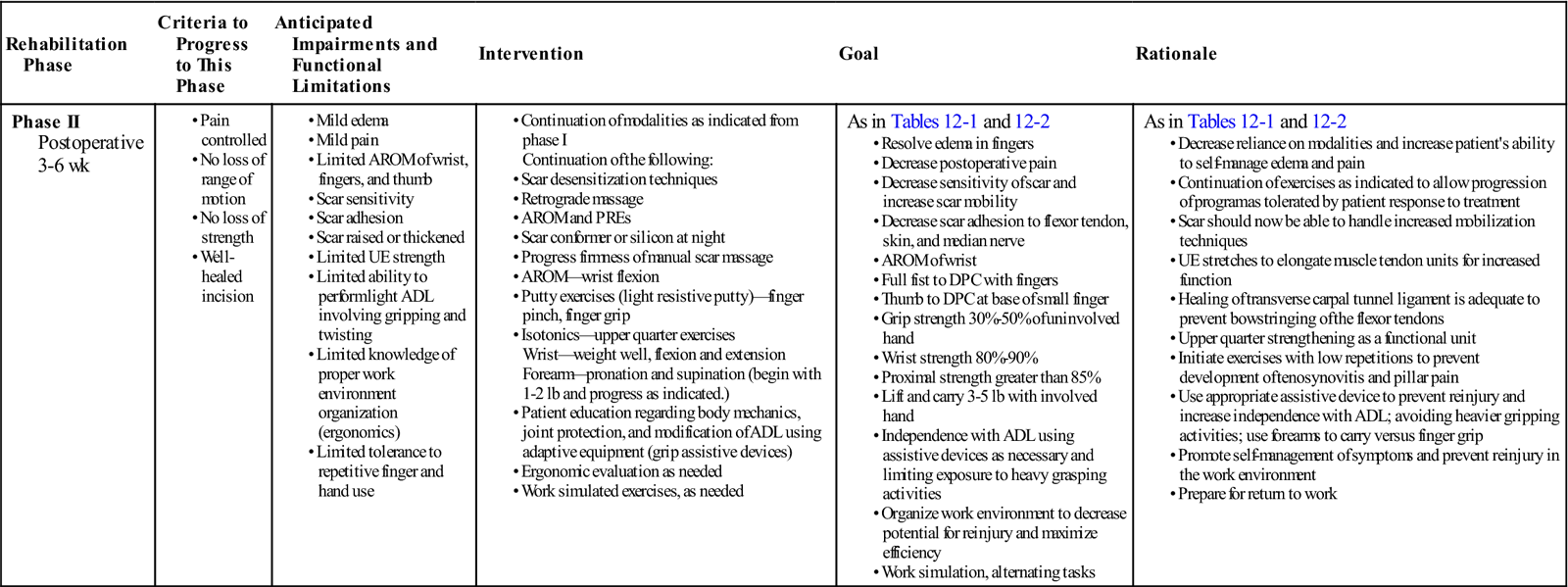
GOALS: Improve strength and endurance in hand and UE for independence in ADL, progress strength and endurance in hand to prepare for return to work, return to full-time work activities (Table 12-3)
TABLE 12-3
< ?comst?>
| Rehabilitation Phase | Criteria to Progress to This Phase | Anticipated Impairments and Functional Limitations | Intervention | Goal | Rationale |
| Phase II Postoperative 3-6 wk |
|
As in Tables 12-1 and 12-2 |
As in Tables 12-1 and 12-2 |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Phase II focuses primarily on strengthening and education (see Table 12-3). It begins on day 22 after surgery and continues until day 42 (6 weeks after surgery). Phase I modalities are continued for edema and pain control. Moist heat may be continued before exercises. Scar desensitization is continued with scar massage and soft tissue mobilization. Texture desensitization techniques are continued, especially as part of the home program. Use of a gel sheeting to pad the sensitive palm may increase comfort for performing self-care and light home care. Tendon-gliding and nerve-gliding exercises and scar massage are continued to prevent or decrease scar adhesions. The pressure used for scar massage is increased in intensity for manual massage. Use of the scar conformer or gel sheeting is continued at night to soften and flatten the scar.
![]() The patient can add active wrist flexion exercises after 21 days with the expectation of full wrist flexion by the end of the sixth week after surgery.
The patient can add active wrist flexion exercises after 21 days with the expectation of full wrist flexion by the end of the sixth week after surgery.
Full UE stretching exercises and neural-gliding exercises are added at this time. UE stretches include composite motions of (1) wrist flexion, forearm pronation, and elbow extension; (2) wrist extension, forearm pronation, and elbow extension; and (3) wrist extension, forearm supination, and elbow extension.77
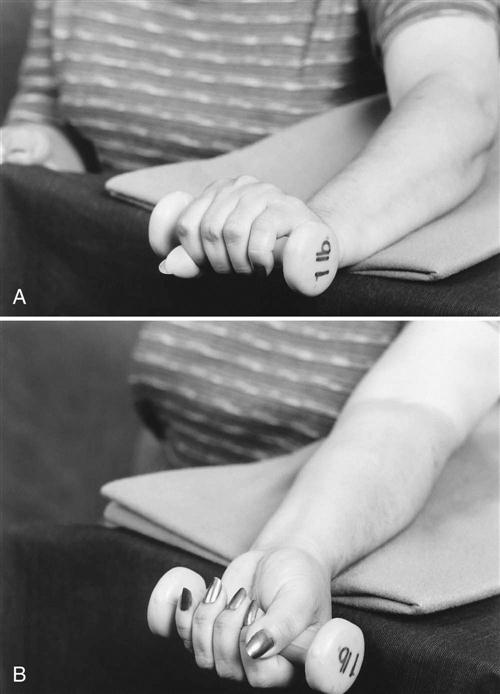
Resistive gripping and pinching exercises with light resistive putty may be started 28 days after surgery. Putty exercises must be comfortably tolerated before moving to more resistive putty; however, if patients begin to complain of pillar pain, this should be discontinued for another week or two. Pillar pain is described in the literature as pain in the thenar or hypothenar areas, and should be distinguished from incisional or local scar tenderness.44,78,79 Pillar pain occurs at the bony attachments of the TCL (the hook of the hamate, pisiform, scaphoid tubercle, and the ridge of the trapezium). Patients with pillar pain may have difficulty with gripping and palmar weight-bearing activities. Modalities may be used to decrease the inflammation and symptoms of pillar pain. Low-intensity continuous US80 (0.5 W/cm2, 3 MHz) has been noted to help decrease this type of pain. The therapist should instruct the patient that the maximum use of putty is two times a day for 5 minutes, and tell him or her to stop using the putty and notify the therapist if the pain increases significantly. Wrist isometric exercises can be continued along with the initiation of grip isometric exercises. The patient can perform grip isometric exercises by squeezing a towel roll in the hand. Light progressive resistance exercises (PREs) are added when pain is controlled. PREs are added for both wrist extension and flexion (Fig. 12-11).76 Resistance should begin at  to 1 lb and progressed to 3 lb as the patient tolerates it.
to 1 lb and progressed to 3 lb as the patient tolerates it.
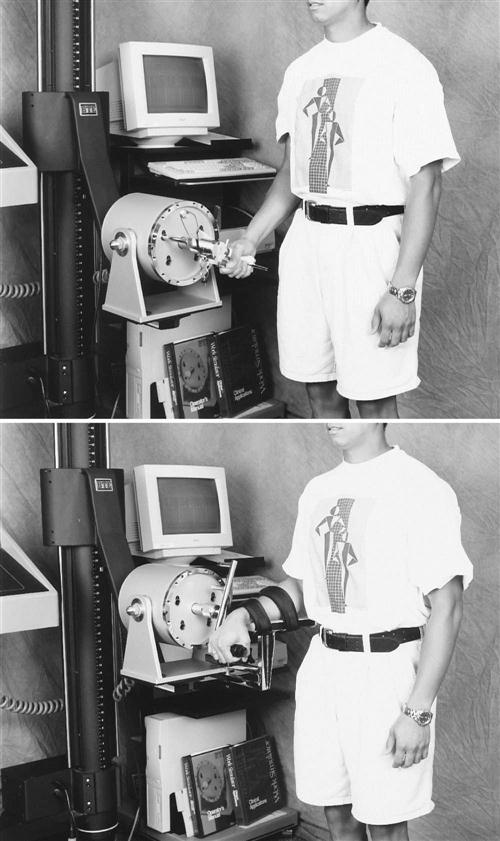
Wrist and grip strengthening are progressed to using a weight well or computerized work simulator (Fig. 12-12). The patient starts on the weight well with no weight or on the work simulator at minimal torque and progresses as tolerated.
Proximal muscle strengthening of the forearm, elbow, shoulder, and shoulder girdle can be started on day 28 after surgery. Forearm rotation strength can be achieved using a hammer held with the elbow flexed at 90° and stabilized against the side of the body. The therapist should ask the patient to rotate the forearm from the neutral position into supination and pronation. Simply moving the hammerhead away from the hand to increase the lever arm, or toward the hand to decrease the lever arm, can change the resistance of the exercise. Bicep curls and elbow extension exercises can be performed with dumbbells beginning at 1 or 2 lb and progressing as the patient tolerates. Shoulder and shoulder girdle exercises beginning with 1 to 2 lb are important and are performed for flexion, abduction, internal and external rotation, and scapular retraction. The patient should be monitored closely during the advancement of the proximal strengthening program to prevent the development of other cumulative trauma disorders, such as shoulder impingement syndrome, lateral epicondylitis, de Quervain’s syndrome, or trigger finger symptoms.
Treatment of the patient after carpal tunnel release surgery may also include instruction on ergonomic principles, proper posture, and body mechanics to prevent recurrence of CTS or the development of other repetitive stress injuries. Instruction should include general topics for all patients and job-specific teaching for those returning to highly repetitive or heavy-labor jobs.
Ergonomic Recommendations
Patients with jobs involving computers should be instructed in workstation setup. According to the literature, the most important factor in CTS and work is wrist position on the keyboard. Based on carpal tunnel pressure studies, in wrist extension angles greater than 15° can increase pressure in the carpal tunnel, which could result in more pressure on the median nerve. Neutral wrist extension could decrease the probability of developing other musculoskeletal disorders affecting the hand and wrist. To maintain this position, elbows should be flexed to 90° or a little less with wrists in a neutral position over the keyboard. A keyboard tray may need to be added to the desk to achieve proper positioning. Using ergonomic keyboards or negatively tilting the keyboard also may be useful for maintaining a neutral wrist position.81 If a wrist rest is used, the patient should be instructed not to press on it during typing but to use it to rest the UEs when scanning the monitor screen.
Patients with sedentary jobs are usually discharged to a home program by the end of phase II. Heavy laborers generally progress to phase III at 6 to 8 weeks after surgery, where more emphasis is placed on increasing strength, endurance, and return to work activities.
Phase III (Remodeling and Maturation Phase)
TIME: 6 weeks after surgery, ending when the scar is mature. This phase can last for 1 year or longer.
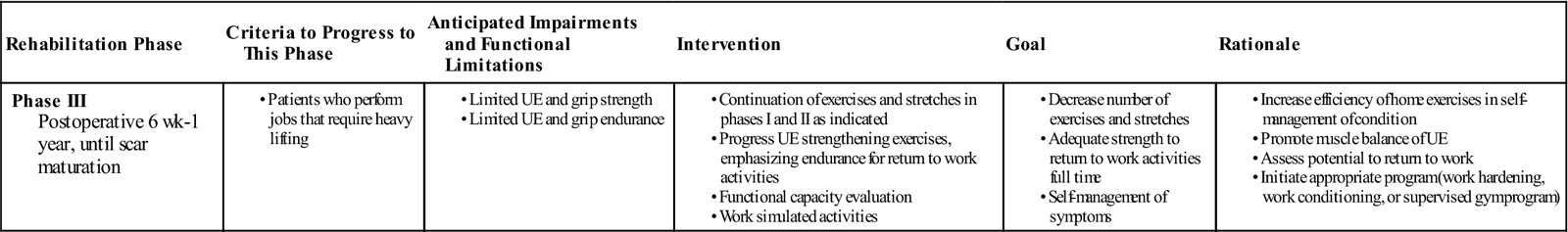
GOALS: Adequate strength to return to full-time work activities, independent home exercise program, self-management of symptoms (Table 12-4)
TABLE 12-4
< ?comst?>
| Rehabilitation Phase | Criteria to Progress to This Phase | Anticipated Impairments and Functional Limitations | Intervention | Goal | Rationale |
| Phase III Postoperative 6 wk-1 year, until scar maturation |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
The types of patients who progress to phase III are heavy laborers, construction workers, mechanics, and assembly workers. These patients should be able to progress to aerobic exercise using a bicycle, treadmill, or UE ergometer. The stretching program and scar management program from phase II is continued. Scar massage also continues, with the patient wearing the scar conformer or gel sheeting until the scar color is no longer reddened. Scar maturation can take as long as 1 year. Phase II strengthening exercises should be continued and progressed as tolerated. Large muscle group exercises using gym equipment or free weights are appropriate at this time for general body conditioning.
Work activity simulation is an important aspect of the phase III therapy protocol. These activities can include using a pipe tree or assembly boards and learning proper lifting and carrying techniques. The use of work simulation equipment can be helpful for strengthening and simulation of specific work activities (see Fig. 12-12). Full return of presurgical grip and pinch strengths often does not occur until 3 to 6 months following surgery.
Clearly, CTS affects patients physically, financially, and psychologically. Comprehensive management of the patient recovering from surgery for CTS optimizes the potential to return to ADL, work, and avocational activities.
Suggested Home Maintenance for THE Postsurgical Patient
The home maintenance section outlines the postoperative rehabilitation the patient is to follow. The physical therapist can use it in customizing a patient-specific program.
Clinical Case Review
1Sharon had carpal tunnel release 2 months ago. She has been making good progress in therapy but continues to complain of paresthesia that was present before surgery. What could explain her continued symptoms?
It is not uncommon for patients to continue with symptoms postoperatively. The healing response of the nerve may take as much as 3 to 6 months. Besides the use of antiinflammatory modalities, wearing a night splint may help keep the wrist in a neutral position and facilitate the healing response.
2Yvonne is a 48-year-old grocery checker who has been diagnosed with intermediate CTS; she has constant numbness and paresthesia but no thenar atrophy. She had surgery 3 weeks ago for a carpal tunnel release, and the edema is persistent. What are some treatment techniques that may be helpful for decreasing her edema at this point?
Light retrograde massage may facilitate lymphatic return. Patients with persistent edema may benefit from wearing a compression glove in conjunction with other edema-controlling modalities. Initially the glove should be worn almost continuously. As the edema decreases, the patient only needs to wear the glove at night.
3Yvonne tends to heal quickly after having surgery. In fact, she had difficulty regaining full knee ROM after knee surgery because adhesions quickly formed around the joint. Limiting the development of scar adhesions also is important in the patient who has had carpal tunnel release. What are some problematic areas Yvonne may have after her carpal tunnel release? What types of treatment can be used to limit scar adhesions in this area?
Limiting the development of scar adhesion to tendons, skin, and nerves is another important aspect of scar management in the patient after carpal tunnel release surgery. Tendon-gliding exercises are continued to move the flexor tendons differentially in the carpal tunnel. Nerve-gliding techniques are helpful in maintaining mobility of the median nerve after a carpal tunnel release.
4Lupe is returning to work (as a receptionist) 8 weeks after carpal tunnel release. Her symptoms have resolved but she is still tender over the incision. What ergonomic recommendations should be made?
In general, a worksite evaluation should be made. Close attention should be paid to the degree of wrist extension (neutral) and postural setup (i.e., head on neck, shoulder, elbow, and overall spine and pelvis position while seated) as it relates to her monitor and job duties. A padded wrist rest or padded gloves may also be useful.




 to 1 lb
to 1 lb
