CHAPTER 28 Carpal, Metacarpal, and Phalangeal Fractures
Carpal, metacarpal, and phalangeal fractures are among the most common injuries treated by hand surgeons. Historical data suggest that 10% of all fractures occur in the metacarpals and phalanges and that 80% of all hand fractures involve the tubular bones.1–3 Until the early 20th century, most carpal and hand fractures were treated nonoperatively. Even today, fractures that are nondisplaced or minimally displaced may be viewed as stable and treated conservatively or with closed reduced and cast immobilization. Unstable fractures require surgical fixation to maintain length, alignment, and rotation. Other options for fixation include percutaneous pinning, external fixation, traditional open reduction and internal fixation, and arthroscopically assisted reduction and internal fixation (AARIF).
HISTORICAL BACKGROUND
Arthroscopic surgery of the wrist and hand is a rapidly evolving discipline. Since Chen first reported on diagnostic arthroscopy of the wrist and finger joints in 1979 with the Watanabe no. 24 arthroscope, techniques for small joint arthroscopy have developed at a rapid pace.4 Current indications include the diagnosis and treatment of numerous wrist disorders, including fractures, soft tissue pathology, and arthritis. Arthroscopy of small joints, including the metacarpophalangeal (MCP) and interphalangeal (IP) joints, has lagged compared with the phenomenal interest generated by wrist arthroscopy. Badia theorized that minimal reporting in the literature and lack of direct teaching of this technique have contributed to the limited use of this potentially useful technology.5
In 1995, more than 15 years after Chen’s classic article, Ryu and Fagan described their experience treating the ulnar collateral ligament Stener lesion in eight thumbs with success.6 Arthroscopic reduction was achieved by reducing the lesion until the avulsed ligament sat juxtaposed to its insertion site on the proximal phalanx. After the reduction was performed, the ligament ends were débrided, and the joint was pinned. The results were excellent, with range of motion and strength comparable to those of the unaffected contralateral thumb.
In 1999, Rozmaryn and Wei presented a paper detailing the technical aspects of MCP arthroscopy, with general references to the potential use of this technique in treating juxta-articular and intra-articular fractures.7 In the same year, Slade and Gutow published a review article on arthroscopy of the MCP joint.8 They offered detailed technical explanations and emphasized that small joint arthroscopy requires specialized instruments and a thorough knowledge of the anatomy within these specialized joints. In 2006, Badia reported encouraging results treating bony gamekeeper’s thumb with AARIF.9
ANATOMY
The MCP joint is composed of several structures, including the osseous metacarpal head, the proximal phalangeal base, and soft tissue restraints, which include the stout volar plate, collateral ligaments, and a relatively thin and flimsy dorsal capsule. Strong extensor tendons run dorsal to the dorsal capsule and are held in check by capsular fibers and the sagittal bands. On either side of the joint are the insertions of the intrinsic muscles on the extensor mechanism. The digital neurovascular bundles rest volar to the joint, along with the flexor tendons; the terminal branches of the dorsal sensory nerves are less predictably centered over the dorsum of the joint.
PATIENT EVALUATION
History and Physical Examination
Particular attention should be paid to patients with frail or “rice paper” skin, such as those with chronic disease and those receiving steroids.10 If small joint arthroscopy is performed on these patients, special care should be taken to limit traction forces across the joint to prevent significant disruption of the skin surface.
Diagnostic Imaging
Plain radiographs provide most of the information necessary to diagnose lesions of the MCP joints. Special views, including oblique and Brewerton views to evaluate the metacarpal head, may be useful adjuncts to traditional posteroanterior and lateral radiographs. Computed tomographic (CT) scans aligned in the sagittal plane can help to define the step-off of intra-articular fractures, and bone scans can help to identify increased activity in the metacarpal head, which suggests possible osteochondral defects.8
TREATMENT
Indications and Contraindications
AARIF is an excellent choice for juxta-articular fractures of the carpometacarpal (CMC) and MCP joints of the thumb and digits, because these small joint injuries require anatomic reduction to prevent post-traumatic arthritis. As Slade and Gutow pointed out in their 1999 article describing arthroscopic techniques for MCP joint fixation, minimal surgical manipulation of the soft tissue envelope and preservation of the blood supply during operative exposure are indispensable for obtaining an optimal result.8 AARIF preserves vascular blood supply to bony fragments by minimizing dissection of the soft tissue envelope surrounding the joints of the hand. Open surgery of tissues surrounding these small joints may contribute to collateral ligament and flexor tendon scarring and shortening, which ultimately limit tendon excursion and lead to stiffness and suboptimal results.11
A example of a fracture pattern amenable to AARIF is the simple two-part fracture with displacement greater than 1 mm involving the metacarpal head or base of the proximal phalanx.10 Other excellent indications for AARIF are for reduction of an avulsion fracture with a rotated fragment from the collateral ligament insertion and for treatment of die-punch articular fractures of the proximal phalangeal base. AARIF enables the surgeon to use the arthroscope to clearly visualize articular reduction with a probe or Kirschner wire and to visualize subsequent percutaneous fixation.5 In pediatric cases, Salter-Harris type III physeal fractures may be reduced and secured without additional injury to the growth plate with the use of AARIF.
Slade and colleagues presented their results using AARIF in 1998 at the Annual Meeting of the Arthroscopy Association of North America (AANA). This study documented fewer complications and improved final range of motion when fractures were treated with AARIF compared with the results of standard open reduction.12
Contraindications to the use of AARIF for MCP and proximal IP fractures are poor soft tissue coverage, open fractures, and active cellulitis.10 Fractures with three or more fragments, comminution, or associated diaphyseal extension that cannot be easily reduced through percutaneous means are also disqualified for AARIF, because these fractures are better treated with standard open approaches.
Conservative Management
Most acute traumatic injuries involving the MCP and proximal IP joints can be managed conservatively with a trial of splint or cast immobilization. Fractures that result in rotational malalignment, an inability to fully extend the digits, or intra-articular displacement are best treated by some form of operative intervention, because nonoperative care may lead to long-term disability, such as pain, stiffness, or post-traumatic arthritis. As the surgeon becomes more adept at small joint arthroscopy, acute indications may evolve due to more accurate assessment of the extent of injury and more precise treatment.5
Arthroscopic Technique
Instruments
Inflow may be provided through a gravity system using a pinch pump and small joint tubing or the camera itself and a standard arthroscopy pump set to maintain a pressure between 50 and 80 mm Hg. The small radius of the inflow cannulas requires higher pressures to ensure adequate irrigation.8
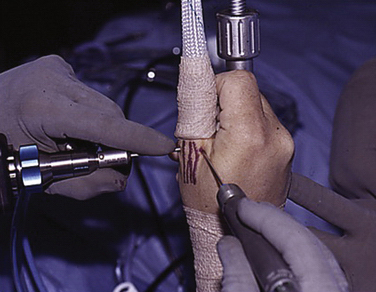
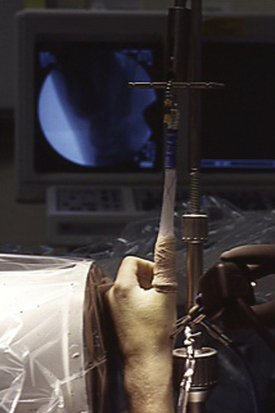
Adequate traction is vital for all joints, particularly those as small as the CMC, MCP, and proximal IP joints. Several commercial traction devices are available to adequately distract the joint and provide traction with the assistance of sterile, disposable plastic finger traps (Fig. 28-1). A mini-fluoroscope is essential to help localize the joint space, assess fracture reduction, and visualize fixation. Standard small hand instruments are also necessary, including a wire driver, mini-curettes, mini-fragment screws, and a power drill for final implant seeding.
Types of Injuries Treated Arthroscopically
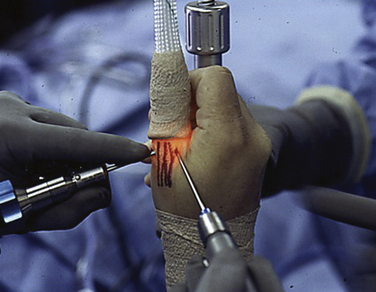
The patient is placed supine on the operating table, and a tourniquet is placed on the upper arm and preset to 250 mm Hg. General or regional anesthesia is appropriate for AARIF, as long as adequate sedation is achieved to allow painless elevation of the tourniquet for the necessary period. The affected arm is positioned on a radiolucent arm table, and the surgeon is positioned at the cephalic side of the arm. With the use of a Chinese finger trap, 5 pounds of longitudinal traction is typically applied to the thumb or affected digit, with the possibility of increasing traction to as much as 10 or 12 pounds. Care is taken to place the operative finger in the line of axis of traction, with the other two surrounding digits providing rotational control.10 Coban is used to wrap the wrist in place against the wrist tower, and it provides additional stabilization for the thumb or digits if the finger trap is loose fitting (Fig. 28-2). A mini–C-arm fluoroscopy machine is positioned parallel to the table, out of the way of the operating surgeon (Fig. 28-3).
Small joints of the hand offer minimal joint spaces, and considerable iatrogenic injury may be caused if care is not taken. In recently traumatized hands, excessive swelling may obscure superficial landmarks, and the surgeon should not hesitate to use C-arm fluoroscopy to assist in localization.10 We agree with Badia, who described an orderly evaluation of the joint beginning with one collateral ligament, followed by assessment of the volar plate and evaluation of the contralateral collateral ligament. This is followed with evaluation of the dorsal capsule and extensor mechanism and examination of the articular surface of the proximal phalanx and metacarpal head.5 After the particular pathology has been identified and addressed, the arthroscope is removed, and the portals are closed with nylon sutures.
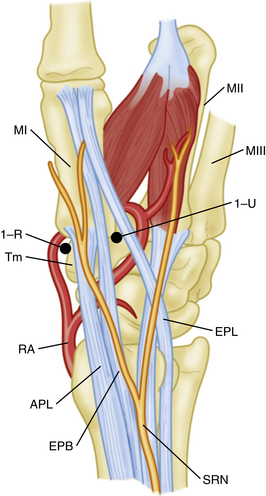
Thumb Carpometacarpal Injuries
Intra-articular fractures of the CMC joint of the thumb represent a subset of injuries amenable to AARIF. In the case of the thumb CMC joint, the base of the first metacarpal is identified and palpated. The incision for the 1-R (radial) portal is placed just volar to the abductor pollicis longus (APL) tendon, and the incision for the 1-U (ulnar) portal is made just ulnar to the extensor pollicis brevis (EPB) tendon (Figs. 28-4 and 28-5). Before the skin incision is made, the CMC joint is distended by injection of 2 mL of normal saline. A 1.9-mm arthroscope is atraumatically introduced into the joint at the 1-R portal, and under direct visualization, the working portal or 1-U portal is established in a similar fashion. Viewing and working portals are interchanged to ensure complete visualization of the critical ligamentous structures, including the dorsoradial, posterior oblique, ulnar collateral, and anterior oblique ligaments.
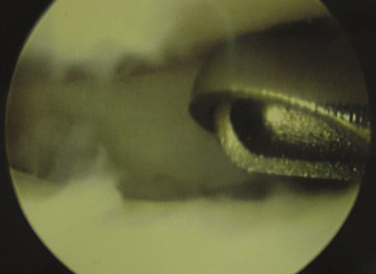
After the thumb CMC joint has been entered, it is often necessary to débride synovitis and fracture hematoma debris with an arthroscopic shaver (Fig. 28-6). A systematic approach is used to visualize critical structures such as the anterior oblique ligament and fracture fragments such as those seen in intra-articular fractures of the thumb metacarpal, including the more common Bennett’s fracture and the less common Rolando variant (Fig. 28-7).
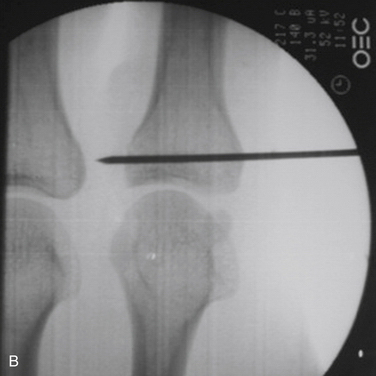
After the joint surfaces have been probed and examined, a blunt probe or trocar is used to manipulate fracture fragments into acceptable position (Fig. 28-8). If the fracture fragment is relatively small (<40% of the articular surface), Kirschner wires may be used to transfix the fragment and provide adequate fixation (Fig. 28-9). For larger fragments, a cannulated screw system may be used. However, we have found it essential to ensure rotational control with a second Kirschner wire fixation before the cannulated screw is inserted over the first Kirschner wire. We introduce the Kirschner wire just up to the fracture site, while holding the fracture fragment with a probe before transfixing the fracture with the Kirschner wire. After fixation is obtained, the arthroscope may be used to verify anatomic reduction and to ensure proper position of the Kirschner wire or screw.
Trapezial Fractures
Fractures of the trapezium are rare, comprising less than 5% of all small bone fractures. These injuries occur when the trapezial body of an adducted thumb is forced onto the articular surface of the carpal bone. Forced radial deviation of the thumb may result in small avulsion fractures caused by capsular strain (Fig. 28-10). Portals are created as previously described for CMC arthroscopy, albeit slightly more proximal, so that the scaphotrapeziotrapezoid (STT) joint may be evaluated. After débridement and evacuation of hematoma to ensure adequate visualization, the fracture fragments are manipulated into position with a probe or Kirschner wire. A 0.035- or 0.045-inch Kirschner wire is useful for this purpose, and it can be used as a joystick to reduce and pin the fragments. Alternatively, one or two fixation screws may be used. Most cannulated screw systems come in a variety of sizes and may be inserted over a 0.035- or 0.045-inch Kirschner wire.
After the fracture has been adequately reduced, the guidewire is inserted as nearly perpendicular to the fracture plane as possible. A second guidewire is inserted to maintain rotational control and fixation during application of the cannulated screw. After proper screw length is measured and chosen, the appropriate screw is inserted over the guidewire, and the fracture is visualized as the screw is inserted. C-arm fluoroscopy is useful during fixation and final reduction. Final fluoroscopic pictures are taken after stability has been confirmed, and the joint is taken through a final range of motion (Fig. 28-11). The topic of carpal bone fixation is addressed more thoroughly elsewhere in this text, but the principles are similar to those discussed here.
Thumb and Digital Metacarpophalangeal Injuries
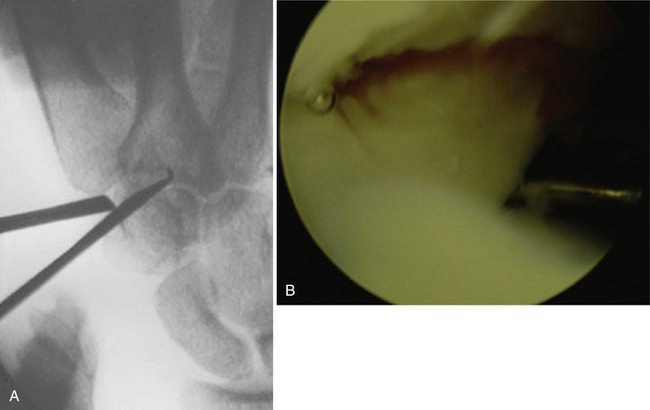
After the patient is positioned and the thumb is suspended as previously described, the principles for thumb MCP AARIF are quite similar to those for CMC arthroscopy and are exemplified by a thumb radial collateral ligament avulsion fracture (Fig. 28-12). The portals for MCP arthroscopy are simple, because they lie on either side of the visible extensor tendon (Fig. 28-13). The interval between the metacarpal head and the proximal phalanx is narrow, and the joint space is localized with an 18-gauge needle before a nick incision of the skin. The arthroscope is introduced at the same angle, and thorough joint inspection is performed along with synovectomy and débridement of fracture hematoma. Fracture reduction is achieved with the use of a probe, and a Kirschner wire is inserted in a perfect position to maintain anatomic reduction (Figs. 28-14 and 28-15). For thumb MCP injuries, we use a short arm thumb spica splint in extension to protect the joint during the initial postoperative period.
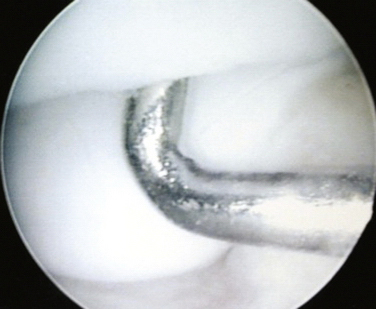
FIGURE 28-14 The arthroscopic view shows anatomic fixation of a radial collateral ligament avulsion fracture.
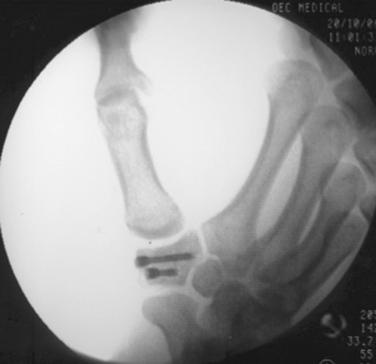
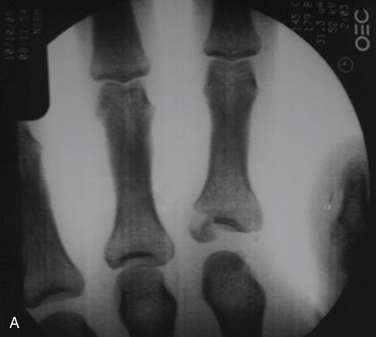
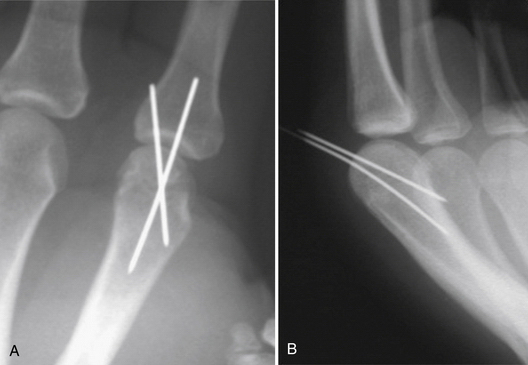
Digital MCP injuries may include fractures of the metacarpal head or the base of the proximal phalanx with or without intra-articular extension. Other fracture patterns include die-punch fractures with impaction of the joint surface, which may complicate fracture reduction. Intra-articular fractures at the base of the index proximal phalanx exhibit disruption of the normal contour and loss of the normal sourcil, a French term meaning “eyebrow” (Fig. 28-16A). After arthroscopic reduction and pinning, the final fluoroscopic images and postoperative radiographs demonstrate excellent alignment, fixation, and healing (see Fig. 28-16B). Postoperative photographs show barely perceptible but well-healed surgical scars and a full range of motion (Fig. 28-17).


FIGURE 28-17 A and B, Postoperative photographs show well-healed surgical scars with full range of motion.
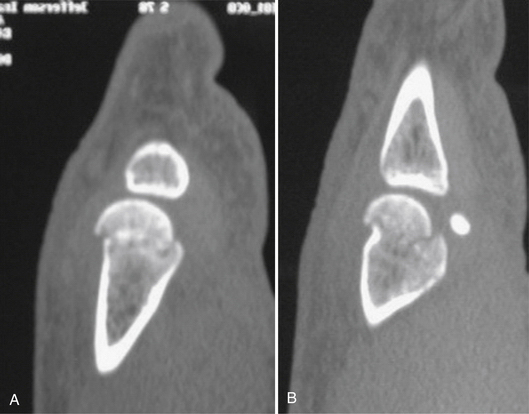
A displaced fracture of the metacarpal head is shown in Figure 28-18. Preoperative CT in the coronal and sagittal planes provides additional insight into the degree of displacement of the fracture and visualization of the intra-articular component, which is not fully appreciated on plain radiographs (Fig. 28-19). AARIF allows superior visualization of the metacarpal fracture component and the adequacy of reduction after pinning. Postoperative radiographs demonstrate excellent alignment and anatomic reduction with no intra-articular step-off or deformity (Fig. 28-20). Final clinical pictures show full motion with no evidence of lag or rotational malalignment (Fig. 28-21). Restoration of joint congruity minimizes the likelihood of future post-traumatic arthrosis in patients treated with AARIF.
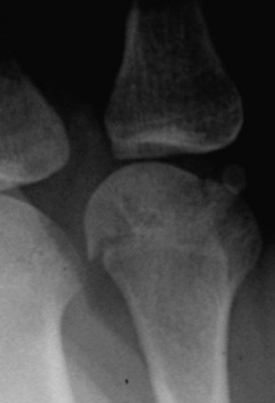
FIGURE 28-18 The radiograph demonstrates a metacarpal head fracture with intra-articular involvement.
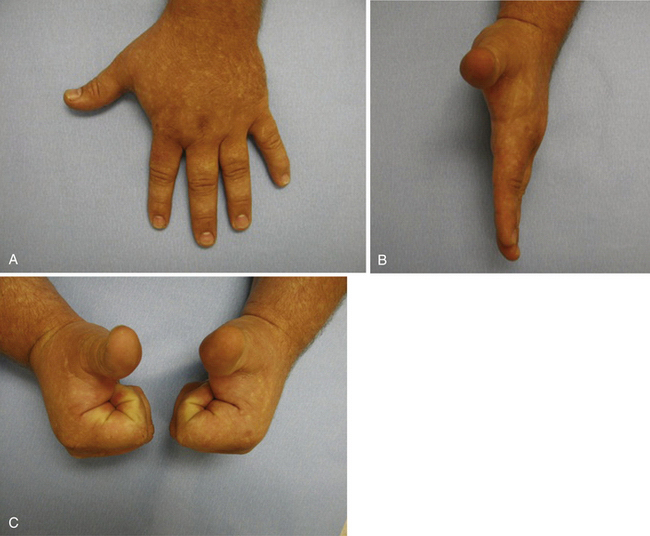
FIGURE 28-21 A–C, Clinical photographs reveal well-healed scars, full digital range of motion, and no evidence of extensor lag or rotational malalignment.
PEARLS& PITFALLS
PEARLS
PITFALLS
Postoperative Rehabilitation
Therapy after minimally invasive surgery in general and after AARIF in particular is one of the principal advantages of this technique. AARIF of small joints offers the benefit of minimal capsular, collateral ligament, and tendon scarring. Consequently, there is faster recovery of the full digital range of motion.9
OUTCOMES
In one of the only known studies comparing AARIF with the standard open approach, Slade and Gutow reviewed the outcomes of 14 consecutive patients with displaced fractures of the MCP joint treated with AARIF.8 All of the patients presented with closed injuries, and all digits of the hand were represented: six thumbs, two index fingers, two long fingers, three ring fingers, and one small finger. The operating time for AARIF averaged 1.8 hours. The final range of motion for the MCP joint averaged 81 degrees, and the total final range of motion for the proximal IP joint averaged 98.8 degrees. There was only one complication, a loss of reduction that required a second AARIF, which ultimately resulted in a successful outcome. The average time before return to work or unrestricted athletic activities was compared with that of a matched set of similar injuries treated with a standard open technique at the same institution. AARIF patients had greater final motion and earlier return of motion than their counterparts who were treated with an open approach.
1. Green DP, Rowland SA, Hotchkiss RN. Fractures and dislocations in the hand. In: Operative Hand Surgery. New York, NY: Churchill Livingstone; 1991.
2. Kelsey JL, Pastides H, Kreiger N, et al. Upper Extremity Disorders: A Survey of Their Frequency and Cost in the United States, 1-71, St. Louis, MO: CV Mosby; 1980.
3. Emmett JE, Breck LW. A review and analysis of 11,000 fractures seen in a private practice of orthopaedic surgery, 1937-1956. J Bone Joint Surg Am. 1958;40:1169-1175.
4. Chen YC. Arthroscopy of the wrist and finger joints. Orthop Clin North Am. 1979;10:723-733.
5. Badia A. Arthroscopy of the trapeziometacarpal and metacarpophalangeal joints. J Hand Surg Am. 2007;32:707-724.
6. Ryu J, Fagan R. Arthroscopic treatment of acute complete thumb metacarpophalangeal ulnar collateral ligament tears. J Hand Surg Am. 1995;20:1037-1042.
7. Rozmaryn LM, Wei N. Metacarpophalangeal arthroscopy. Arthroscopy. 1999;15:333-337.
8. Slade JFIII, Gutow AP. Arthroscopy of the metacarpophalangeal joint. Hand Clin. 1999;15:501-527.
9. Badia A. Arthroscopic reduction and internal fixation of bony gamekeepers thumb. Orthopaedics. 2006;29:675-678.
10. Barbieri RA. Arthroscopic treatment of metacarpophalangeal joint fractures in the hand. In: Capo J, Tan V, editors. Atlas of Minimally Invasive Hand and Wrist Surgery. New York, NY: Informa Healthcare; 2008:235-238.
11. Woods GL. Troublesome shaft fractures of the proximal phalanx. Hand Clin. 1988;4:75-85.
12. Slade JFIII, Cappelino A, Ansah P. Paper presented at the 17th Annual Meeting of the Arthroscopy Association of North America, 1998. Orlando, FL. The efficacy of arthroscopic treatment of intra-articular fractures of the small joints of the hand. 1998.