Chapter 15. Cardiovascular emergencies
Ischaemic heart disease is the most common cardiovascular problem in the UK. Approximately one in four men and one in five women die from the disease. Acute manifestations of ischaemic heart disease are dealt with together under the term Acute Coronary Syndrome (ACS). Myocardial infarction (where prolonged ischaemia is causing irreversible damage to the myocardium) should be identified because reperfusion can be achieved by thrombolysis or by primary angioplasty. The factors that contribute to the development of ischaemic heart disease include:
• Cigarette smoking
• High blood cholesterol levels
• Hypertension
• Diabetes
• Family history
• Obesity.
The association of two or more risk factors greatly increases the chance of developing ischaemic heart disease. Cardiovascular events may still occur in individuals without identifiable risk factors. Ischaemic heart disease occurs when the supply of oxygenated blood to the heart is insufficient for the demands of the myocardium.
Ischaemic cardiac pain
Angina pectoris
• The discomfort of angina is caused by reversible myocardial ischaemia and usually occurs during conditions of increased oxygen demand in the presence of a fixed supply, most typically during physical exertion or mental and emotional stress
• When the patient ceases the activity and rests, the discomfort passes off rapidly (within 2–3 minutes)
• Patients with angina often describe a feeling of tightness in the chest (‘like a tight band’) or liken the discomfort to a weight on the chest
• The pain is felt retrosternally (behind the sternum) and may radiate across the chest, spreading into the arms
• In some patients, the pain may also radiate into the throat or jaw.
Acute coronary syndrome (unstable angina)
• The term unstable angina is used to describe a rapidly progressive, deteriorating pattern of angina often occurring in patients whose angina has been previously stable
• The patient’s exercise tolerance is reduced and ischaemic pain occurs more frequently
• The consumption of glyceryl trinitrate is often increased
• Ischaemic pain occurring at rest or on only minor exertion is a particularly worrying feature
• Unstable angina is a medical emergency and most patients are admitted to hospital for investigation and treatment, as there is a high instance of subsequent myocardial infarction.
Myocardial infarction
• The pain of myocardial infarction is similar in nature, site and distribution to that of angina, although it usually persists longer and is associated with more profound extra effects, such as profuse perspiration, dizziness and nausea and vomiting
• The intensity of the pain is not a reliable indicator of the immediate risk to the patient
• Only about half those with acute myocardial infarction will have a history of previous heart disease
• In elderly people and diabetics, pain may be absent (the ‘silent’ MI).
Myocardial infarction
The effects of an MI depend on the extent and location of the muscle loss, as well as on the pre-existing state of the myocardium.
The complications of myocardial infarction (see box 15.1) may be difficult to diagnose prehospital. Electrical effects are easier to diagnose using prehospital cardiac monitoring and indeed, are more commonly seen early in the course of the acute coronary event. Ischaemic and infarcted myocardial segments are electrically unstable and prone to ventricular fibrillation or tachycardia, both causes of cardiac arrest and sudden cardiac death. Atrial fibrillation also may occur which leads to a further reduction in cardiac output and an increase in risk of intracardiac thrombosis and peripheral embolisation. Interruption in the blood supply of the sinus node or atrioventricular node is a cause of bradycardia and degrees of heart block.
Box 15.1
• Cardiogenic shock – systolic output is reduced so that major organs are underperfused
• Mitral regurgitation – papillary muscles rupture causing an incompetent valve
• Cardiac tamponade – the myocardium ruptures and blood enters the pericardium
• Ventricular septal defect – the myocardium ruptures between the ventricles.
Diagnosis
• The diagnosis is made by combining the history and examination with the findings on ECG
• The patient will be anxious, pale, sweaty and may be complaining of severe chest pain, nausea and may be short of breath
• A tachycardia is likely, hypotension is an ominous sign
• Pulmonary oedema may have developed
• The 12-lead ECG may show ST segment elevation (an ‘ST elevation MI’), which will give information about which area of the myocardium is affected.
Treatment
• Sit the patient up, give them high flow oxygen, put them on cardiac monitoring and establish intravenous access as a precaution in the first instance
• Record a 12-lead ECG at the earliest opportunity, if available
• Morphine should be given; as well as providing analgesia it will have the effect of reducing myocardial demand and improving coronary blood flow
• An antiemetic should be given, both to reduce the effects of the MI and the effects of the morphine (avoid cyclizine, which may produce vasoconstriction)
• Sublingual GTN may improve the patient’s pain (only give if the systolic blood pressure is >90 mmHg). GTN reduces the workload of the heart as well as causing the coronary arteries to dilate. Sublingual administration of 0.4–0.8 mg is either by tablet or spray
• Unless contraindicated, all patients with acute coronary syndrome (ACS) or suspected myocardial infarction (MI) will benefit from 300 mg aspirin orally (contraindications include active peptic ulcer disease, bleeding disorders or allergy to aspirin)
• Consider thrombolysis dependent on local protocols.
• Address complications such as arrhythmias or pulmonary oedema
• Diuretics such as frusemide 40–120 mg IV may be used to address clinically significant heart failure and pulmonary oedema.
Thrombolytic therapy
• Thrombolytic agents activate the natural mechanism for producing clot breakdown ( lysis)
• Dissolution of the obstructing thrombus occurs with reperfusion of ischaemic myocardium
• Treatment is most effective when given as soon as possible after the onset of symptoms. The most serious side-effect is intracerebral bleeding
• Generally thrombolysis is used when primary angioplasty is not available or transfer times are prolonged
• The diagnosis of MI and the administration of thrombolysis may be made autonomously by the paramedic or may be achieved via telemetry with the receiving hospital
• Tenecteplase and reteplase are the preferred thrombolytic agents for prehospital use, as each is administered in bolus doses rather than as an infusion. Tenecteplase is given in a single dose adjusted according to the patient’s weight. Reteplase is given as two bolus doses that must be administered 30 minutes apart
• Concurrent treatment with heparin is usually required
• Adverse events following thrombolytic therapy include ventricular fibrillation, ventricular tachycardia and other arrhythmias. Hypotension and shock may also occur. These complications should be addressed as per normal protocols
• Rarely, anaphylaxis may occur, and is also treated according to standard protocols, ensuring that administration of the thrombolytic agent is discontinued immediately
• The incidence of haemorrhagic stroke (through disruption of an existing intracerebral clot) is 1 per 200 patients thrombolysed, and half of these cases will result in death
• In order to ensure that the benefit of prehospital thrombolysis outweighs the risk of adverse events, only patients meeting the criteria established by the Joint Royal Colleges Ambulance Liaison Committee (JRCALC) should be administered thrombolytic agents by paramedics.
Dissecting aortic aneurysm
A dissecting aortic aneurysm is one of the most serious cardiovascular emergencies. The condition is more common in men and hypertension is an important predisposing factor. The condition starts with a tear in the intima of the aorta, usually in the ascending part of the arch of the aorta and the dissection may involve one or more major branches of the aorta, including the coronary arteries. Rupture of the aorta into the pericardium or pleura may occur and is usually rapidly fatal.
The pain of dissecting aneurysm is similar to that of myocardial infarction, although perhaps a little more abrupt in onset. It is sometimes described as having a ‘tearing’ quality and often radiates into the back between the scapulae.
A dissection is sometimes manifest as a discrepancy in the pulses in the arms or a marked difference in blood pressure on the two sides. The same may occur with the carotid or femoral vessels: disturbance of consciousness occurs with interruption of cerebral blood supply. Myocardial infarction (from obstruction of the coronary arteries), stroke or paraplegia (from obstruction to spinal blood flow) may be seen. The administration of thrombolytic drugs for MI due to aortic dissection will seriously jeopardise the outcome.
Management
In many cases, the patient will be suspected to be suffering from myocardial infarction. ECG monitoring, oxygen therapy and analgesia are equally appropriate in both conditions, while sublingual nitrates will do no harm in dissection. Venous access will be established at an early stage and used to provide effective analgesia. Do not administer thrombolysis if an aortic dissection is suspected. Rapid transfer to hospital is mandatory.
Pulmonary embolism
Pulmonary embolism is commonly under-diagnosed. It occurs when a thrombus that has formed in a large vein in the leg or pelvis becomes dislodged and is carried through the venous system and right ventricle into the pulmonary circulation.
Conditions associated with a high risk of thromboembolism include pregnancy, recent operations (particularly orthopaedic and gynaecological procedures), chronic heart failure or pulmonary disease, fractures and other injuries of the legs, chronic venous insufficiency affecting the lower leg, prolonged immobility, including prolonged travel and the presence of carcinoma.
The immediate result of pulmonary thromboembolism is obstruction of all or part of the pulmonary arterial bed which, when severe, will lead to pulmonary hypertension with acute right ventricular dilation and failure, tachycardia and a decline in cardiac output. Pulmonary embolism can therefore present with collapse due to electromechanical dissociation.
Diagnosis
Treatment
• Outside hospital, treatment will centre on emergency resuscitation where appropriate, the administration of oxygen, instituting cardiac monitoring and securing intravenous access
Cardiac tamponade
Cardiac tamponade occurs when fluid collects in the pericardial cavity in quantities sufficient to interfere with cardiac filling and obstruct venous return. The most common cause is a penetrating injury to the anterior chest wall which penetrates the myocardium allowing blood to fill the pericardium. Other causes produce fluid which builds up more gradually.
• Trauma – blood
• Following myocardial infarction – blood or serous fluid
• Following surgery – blood or serous fluid
• Malignancy – serous fluid
• Infection – purulent fluid (pus).
Diagnosis
• The cardinal diagnostic feature of cardiac tamponade is a reduction in cardiac output associated with systemic venous congestion
• With rapidly developing effusions, as may occur with cardiac trauma, quiet heart sounds occur but the recognition of this sign is difficult
• Electromechanical dissociation may occur
• When tamponade develops slowly, the clinical features may resemble heart failure: dyspnoea, tachycardia, congestion of the neck veins, hepatic engorgement and peripheral oedema.
Treatment
Immediate treatment may be life-saving and in most cases, will be undertaken in hospital after confirmation of the diagnosis by echocardiography. Only very rarely is pericardial aspiration or open thoracotomy by medical staff performed before hospital admission. Treatment by the paramedic will be the provision of oxygen, establishment of intravenous access and cardiac monitoring.
Cardiac arrhythmias
The treatment of asystole, pulseless ventricular tachycardia, ventricular fibrillation and pulseless electrical activity follows Advanced Life Support guidelines.
All arrhythmia patients require oxygen.
In prehospital care, treatment of arrhythmias is relatively simple. The golden rule is to treat the patient and not the arrhythmia.
TREAT THE PATIENT, NOT THE ARRHYTHMIA.
Treatment of tachycardia
Prehospital treatment should only be undertaken if the arrhythmia presents a significant threat to the patient’s cardiovascular status or life and wherever possible during ECG monitoring, with a paper record made of the initial tachycardia and any response to treatment.
Tachycardias may be classified as regular or irregular with narrow or broad (>120 ms) QRS complexes.
Regular narrow complex
• Sinus tachycardia
• AV nodal tachycardia
• Macroreentrant AV tachycardia (in Wolff–Parkinson–White syndrome)
• Atrial tachycardia with fixed AV conduction
• Atrial flutter with fixed AV conduction.
Irregular narrow complex
• Atrial fibrillation
• Atrial flutter with variable AV conduction
• Atrial tachycardia with variable AV conduction.
Regular broad complex
• Ventricular tachycardia
• Any cause of regular narrow complex with coexistent bundle branch block.
Irregular broad complex
• Atrial fibrillation with coexistent bundle branch block.
Sinus tachycardia
Treatment should be directed towards the cause of the tachycardia (e.g. hypovolaemia due to haemorrhage).
Atrial tachycardia and atrial flutter
Drug treatment may be considered during rapid transfer to hospital.
Carotid sinus massage or the Valsalva manoeuvre (‘ Take a huge breath in and strain as if you were on the toilet’) is unlikely to terminate the arrhythmia but may abolish ventricular activity long enough for the underlying atrial abnormality to be recognised and the correct diagnosis made. Both of these are ‘vagal manoeuvres’ and are more effective in the younger patient and when lying flat. Vagal stimulation with a Valsalva occurs on release of the manoeuvre.
Carotid sinus massage (massage over the carotid artery level with the upper border of the larynx) should not be performed for more than 5–10 seconds.
The patient with acute paroxysmal cardiovascular compromise is best treated by synchronised cardioversion after arrival in hospital.
Amiodarone (150 mg IV given over 10 minutes, repeated once) may be administered by paramedics.
Atrial fibrillation
Atrial fibrillation with a moderate ventricular response (pulse rate <120/min) usually responds to a course of oral digoxin.
In the patient with pronounced tachycardia, intravenous digoxin, verapamil or β-blocker may slow the ventricular rate.
Administration of more advanced drugs or synchronised defibrillation is best undertaken in hospital.
Junctional tachycardia
Junctional tachycardia (or AV nodal reentrant tachycardia – AVNRT) may be terminated by vagal manoeuvres (carotid sinus massage or the Valsalva manoeuvre).
If vagal manoeuvres fail, the first-line treatment is adenosine 6 mg by rapid IV injection, followed if unsuccessful after 1–2 minutes by 12 mg and followed again if unsuccessful by 12 mg.
Paramedics are not currently licensed to administer adenosine. Immediate evacuation for treatment in hospital is appropriate. Cardiac monitoring must be maintained during the treatment.
Amiodarone (150 mg IV given over 10 minutes repeated once) may be administered by paramedics.
Remember to print a rhythm strip.
Ventricular tachycardia
If ventricular tachycardia is pulseless the resuscitation algorithm for ventricular fibrillation should be followed.
 |
| Figure 15.1. |
| Junctional tachycardia (AVNRT). |
If a pulse is present, oxygen should be given, followed by immediate rapid transfer to hospital.
Administration of intravenous amiodarone is indicated, subject to local protocol, followed if necessary after arrival in hospital by DC cardioversion.
Isolated ventricular complexes (ventricular premature beats) do not require treatment unless they occur in salvos in which case 150 mg of amiodarone should be given IV.
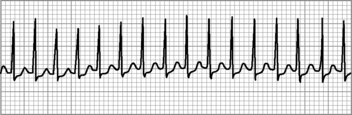
 |
| Figure 15.2. |
| Ventricular tachycardia. |
Treatment of bradycardia
First- and second-degree heart block rarely require treatment. Very occasionally, enough complexes fail to be transmitted in second-degree heart block to cause bradycardia with cardiovascular compromise (hypotension or chest pain). Atropine 0.5 mg (repeated if necessary to a maximum dose of 3 mg) should then be given.
If third-degree heart block (‘complete heart block’) is accompanied by an adequate cardiovascular status, it may be appropriate to delay treatment until arrival in hospital. Otherwise treatment is with intravenous atropine (0.5 mg, repeated if needed to a maximum dose of 3 mg). If this is unsuccessful, external pacing (if available) should be attempted.
In summary, bradycardia or heart block requires the following treatment.
1. First-degree block – none
2. Second-degree block – none or atropine
3. Third-degree block – none, external pacing or atropine
4. Sinus bradycardia – none or atropine.
For further information, see Ch.15 in Emergency Care: A Textbook for Paramedics.