Chapter 26 Cardiovascular disorders
Cardiovascular disease is an enormous health problem in the Western world and is high in the list of causes of death. Evidence from clinical trials suggests that prevention of hypertension and lipidaemia (see Chapter 27 ‘Problems with lipid metabolism’, p. 203) can significantly reduce cardiovascular disease and deaths.
Physiology of the Heart
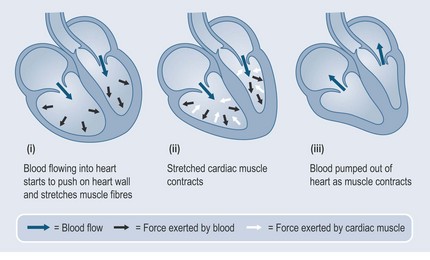
Hydrostatic Pressure
A constant hydrostatic pressure is maintained in two main ways:
Cardiac glycosides in digitalis, digoxin and Crategus (hawthorn) increase the force of contraction of the heart (see Chapter 24 ‘Glycosides’, p. 183), which is important in patients with heart failure.
• How the Kidneys can Affect Blood Pressure
The kidneys perform two functions for the cardiovascular system:
Stages in the Removal of Water from the Body
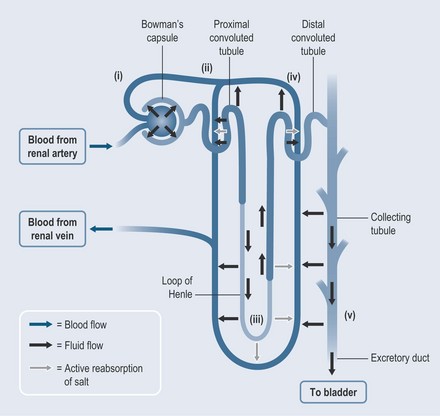
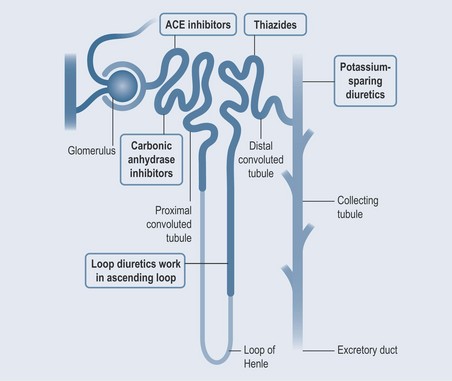
Figure 26.2 shows the structure of a nephron, the functional unit of the kidney. The numbers in the figure are explained below.
(i) Filtration
Blood enters the glomerulus of the kidney under pressure. This pressure forces the water and small molecules (e.g. sodium, potassium, glucose) that are present in the blood through the basement membrane of the glomerulus and into the Bowman’s capsule (Figure 26.2). At this stage, the filtered fluid is mainly blood plasma minus largely all the plasma proteins (there is some seepage of these, but not much). Factors such as heavy exercise can increase the amount of protein found in the urine, but a large amount of protein in the urine indicates kidney pathology. The fluid flows from the Bowman’s capsule into the proximal tubule.
(ii) Active Transport
All the amino acids and glucose, and a large amount of the sodium, potassium and other salts are reabsorbed in the proximal tubule. The active transport of sodium out of the proximal tubule is controlled by angiotensin II. If this is reduced, by medication such as an ACE inhibitor (see Figure 26.6), the sodium remains in the tubule, and the water stays with it. As a result, the patient urinates more.
(iii) Loop of Henle
The filtered fluid passes from the proximal tubule into the descending part of the loop of Henle, where the osmotic gradient still encourages water to leave the nephron. The fluid is encouraged to leave the descending part of the loop because, in the ascending part – which is aligned directly opposite – an active transport mechanism pulls sodium salts from the loop; water from the descending loop accompanies the salts as the result of osmosis. However, fluid cannot follow the salts from the ascending loop because the wall of the loop is impermeable to water. This is where loop diuretics work, by preventing sodium reabsorption.
(iv) Distal Convoluted Tubule
More sodium is removed from the tubules by active transport, with yet more water being pulled out by osmosis. Thiazides (Figure 26.5) such as bendroflumethiazide act here.
(v) Collecting Tubule
This is where the final balancing of water and electrolytes takes place, before the fluid is removed from the body. Potassium-sparing diuretics (Figure 26.5) work here, as well as in the distal convoluted tubules. The collecting tubule is normally impermeable to water, but it can become permeable in the presence of antidiuretic hormone (ADH), which is secreted by the pituitary gland (see Chapter 37 ‘Metabolic disorders’, p. 288). As much as 75% of water in the urine can be reabsorbed as it leaves the collecting duct by osmosis. A failure to produce ADH (due to a fault in the posterior pituitary gland) is seen in the condition known as diabetes insipidus, which involves excretion of copious amounts of urine, despite reduced consumption of fluids.
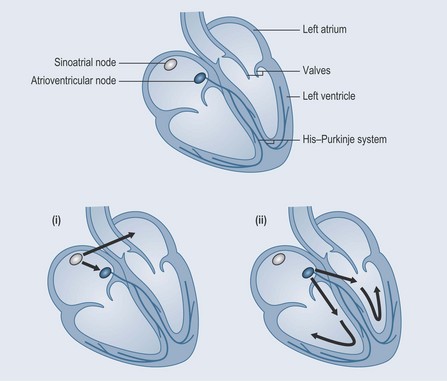
Electrical Stimulation of the Heart
The autonomic nervous system (see Figure 31.5, p. 239) stimulates, and therefore increases, the heart rate through the stimulation of the sympathetic nervous system. This is where the beta-adrenoceptor antagonists (beta-blockers; see below) act (Figure 26.3):
The Special Nature of Heart Muscle
An action potential stimulates the rapid release of sodium ions, followed by the slower release of calcium ions, into the heart muscle. This occurs through voltage-gated ion channels (see Figure 31.2, p. 237). These channels are the site of action of calcium-channel blockers and potassium-channel activators (see below).
Contraction stops when this flow is shut off and the normal electrolyte balance restored.
The sodium–potassium pump removes sodium and pumps potassium back into the muscle cells against the respective concentration gradients (see Figure 31.1, p. 236). The increased permeability of the membrane to potassium inhibits the generation of the action potential.
Depolarization starts in the sinoatrial (SA) node, spreading over the atria to the atrioventricular (AV) node and on to the conducting fibres in the bundle of His (in the intraventricular septum) and the His–Purkinje system. The ventricular muscle then contracts.
Cardiac Conditions
Hypertension
• Pharmacological Treatment of High Blood Pressure
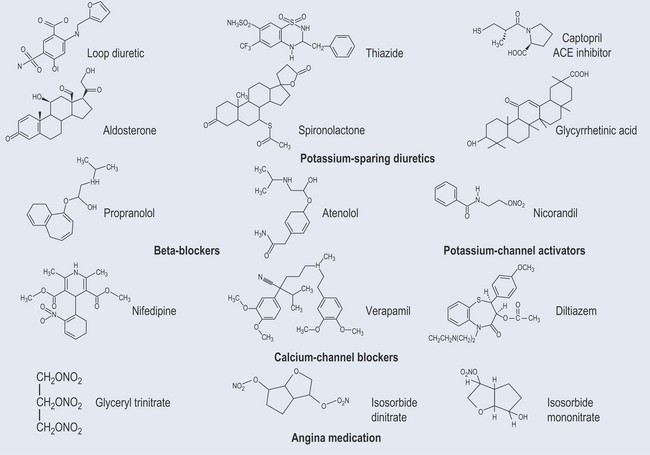
Figure 26.4 illustrates the structures of the different types of cardiovascular medication.
Diuretics
Most diuretics work by inhibiting sodium and water reabsorption at various points in the nephron (Figure 26.5). As the various diuretics increase sodium excretion, water removal occurs by the principle of osmosis (see Chapter 16 ‘How do drugs get into cells?’, p. 123).
Loop Diuretics
General Adverse Effects of Loop and Early Distal Tubule Diuretics
Hypokalaemia (Low Levels of Potassium)
Levels of potassium are reduced in plasma due to loss of potassium in urine, resulting in:
Potassium-Sparing Diuretics
Potassium-sparing diuretics (Figure 26.5) are the weakest diuretics, but they do reduce sodium loss.
Aldosterone
• Carbonic Anhydrase Inhibitors
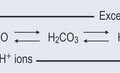
Under normal conditions, the action of carbonic anhydrase retains sodium and bicarbonate in the plasma (see Figure 18.3, p. 135). This mechanism is relevant not only for maintaining blood pressure but also the correct pH of the blood, which must be kept within very narrow limits (see Chapter 8 ‘Acids and bases’, p. 58).
• Beta-Blockers
The beta-adrenoreceptors are found in three main areas of the body:
Side Effects
• Calcium Antagonists (Calcium-Entry Blockers, Calcium-Channel Blockers)
Calcium antagonists affect the cellular entry of calcium, rather than its action on the cell.
Muscle contraction is calcium dependent (see Chapter 31 ‘The nervous system’, p. 237). There are muscles in the peripheral blood vessel walls and the heart is predominantly muscle. If the calcium channels are blocked then vasodilatation of the blood vessels takes place and the contractility of the heart muscle is reduced. There are three classes of calcium antagonist:
All the calcium antagonists are subject to the first-pass metabolism to a great degree.
• Angiotensin-Converting Enzyme Inhibitors
Angiotensin-converting enzyme (ACE) inhibitors inhibit the activity of angiotensin-converting enzyme (Figure 26.6). Angiotensin makes the kidneys retain salt and water. ACE inhibitors:
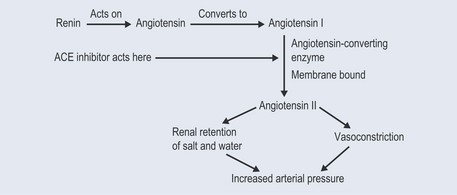
Figure 26.6 The action of the angiotensin-converting enzyme (ACE) inhibitors on the renin–angiotensin system.
Side Effects
Angina
Treatment is directed towards clearing the coronary arteries. An antithrombotic (see Chapter 28 ‘Blood disorders’, p. 212) is used as the primary treatment. Surgery might be necessary in severe cases (bypass surgery or coronary angioplasty).
• Pharmacological Treatment of Angina
Glyceryl Nitrate
Isosorbide Dinitrite and Isosorbide Mononitrate
Potassium-Channel Activators
These have a similar action to nitrates and relax the walls of the coronary arteries, improving blood flow. Smooth muscle relaxation occurs by selectively increasing the membrane permeability to potassium, which flows out of the cell quickly after the muscle cell has been activated. The resulting charge across the membrane makes it more difficult to generate another action potential, leaving the muscle in a state of rest for longer (see Figure 31.2, p. 237).