13 Cardiovascular disease
Questions
What is the role of amiodarone in the acute management of asystole or pulseless electrical activity (PEA)?
What are the possible causes of atrial extrasystoles, in a patient with a normal echo, which last for several days and then disappear spontaneously? Is treatment with anxiolytics recommended?
How safe is it to stop administration of carvedilol to a patient with heart failure? Can the drug be tapered off? What are the effects/dangers of stopping carvedilol suddenly? What, if any, are the reasons for discontinuing carvedilol in patients with heart failure?
There have been a number of recent publications concerning aspirin versus warfarin trials. Would you recommend prescribing warfarin for secondary prevention of coronary heart disease in patients suffering from their first myocardial infarction (MI)?
Is there any benefit in combining aspirin with clopidogrel in post-MI angina and ischaemic stroke? A MATCH trial showed this combination not to be of benefit – would you therefore recommend we stop using this combination in our hospital unit?
You have said that in IV drug users the microbes go directly to the right ventricle, thus causing endocarditis in the right heart. But in dental xCardiovascular disease procedures the microbes also go through the veins to the right heart first, so why are the left heart valves more commonly affected?
In the treatment of hypertension, is it recommended to commence treatment with two drugs containing a thiazide (if elderly) or a beta-blocker (if young)?
Patients at medium risk of DVT and pulmonary embolism are usually given specific prophylaxis with low-dose heparin at a dose of 5000 units subcutaneously every 8-12 hours until the patient is ambulatory. Is the first dose given immediately after, say, extensive varicose vein surgery of small and great saphenous veins?
In a patient with heart failure and atrial fibrillation on warfarin who experiences frequent transient ischaemic attacks, will the patient benefit from having aspirin prescribed?
Pulsus bisferiens has two systolic peaks: the percussion and tidal waves. In dicrotic pulse, the second peak is in diastole immediately after the second heart sound (Fig. 13.1).
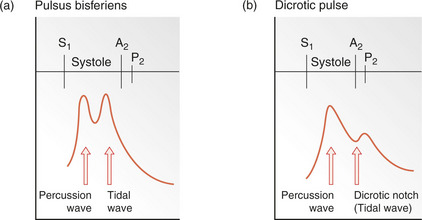
Fig. 13.1 Configurational changes in the carotid pulse and their differential diagnosis. (a) Pulsus bisferiens, with percussion and tidal waves occurring during systole. This type of carotid pulse contour is observed most frequently in patients with dominant regurgitation; occasionally it is seen in patients with mitral valve prolpase or in normal individuals. (b) Dicrotic pulse. This results from an accentuated dicrotic wave and tends to occur in sepsis, severe heart failure, hypovolaemic shock, cardiac tamponade and after aortic valve replacement. A2, aortic component of the second heart sound; P2, pulmonary component of the second heart sound; S1, first heart sound.
The percussion wave is the first wave produced by the transmission of the left ventricular pressure in early systole. With recoil of the vascular bed a second weaker wave (tidal) occurs which can be felt in the radial artery in the presence of slow ventricular emptying, e.g. in mixed aortic valve disease. A double pulse is bisferiens (Fig. 13.1).
Fluoroscopy is dynamic radiography. X-rays are being taken continually so that the image is moving, not static as in a chest X-ray. Radiation hazards limit the time used but it is invaluable in placing catheters etc. in the correct position.
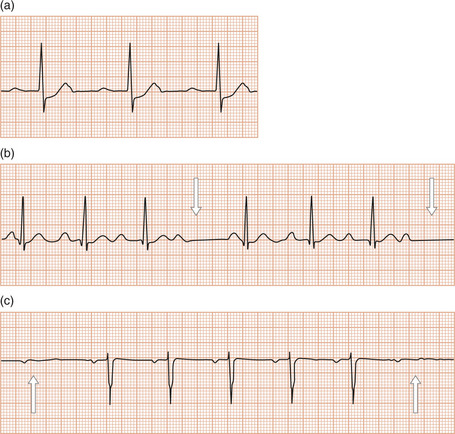
Fig. 13.2 (a) An electrocardiogram showing first-degree atrioventricular (AV) block with a prolonged PR interval. Coincidental ST depression is also present in this trace. (b) Wenckebach (Mobitz type I) AV block. The PR interval gradually prolongs until the P wave does not conduct to the ventricles (arrow). (c) Mobitz type II AV block. The P waves that do not conduct to the ventricles (arrow) are not preceded by gradual PR interval prolongation.
Atrial ectopic beats are usually of no significance. Treatment is not usually required but a beta-blocker can be used, particularly with anxiety.
Changes in the myocardial gene expression occur when the ventricle is overloaded, i.e. heart failure and there is a return to the fetal pattern, as shown in animal models. There is a shift from αα (usually predominates in the atrium) to ββ (usually mainly in the ventricles) myosin heavy chains in the atria.
Toxic levels of digoxin cause an increase in intracellular calcium, which leads to depolarization of the cells, initiating arrhythmia.
The CURE trial, which involved over 12000 patients, compared treatment with aspirin and aspirin plus clopidogrel. There was some suggestion of a better outcome with the two drugs but there was an increase in haemorrhagic complications. It was therefore recommended that clopidogrel be used for those people in whom aspirin is contraindicated. However, current guidelines recommend that aspirin and clopidogrel should be given to all patients with acute coronary syndromes unless cardiac bypass surgery is planned. There have been no published studies on unfractionated heparin or low-molecular-weight heparin with clopidogrel. Finally, the clopidogrel should be continued for at least 9-12 months.
The use of thrombolytic therapy continually changes. The diagnosis of MI was also changed to include a classic history and raised troponins. More recently, however, streptokinase therapy or other thrombolytics have been recommended only for patients with ECG changes of ST elevation (STEMI) (Fig. 13.4). Non-STEMI (no ST elevation) patients are not given thrombolytic therapy, even though troponins are raised, but are referred for coronary intervention.
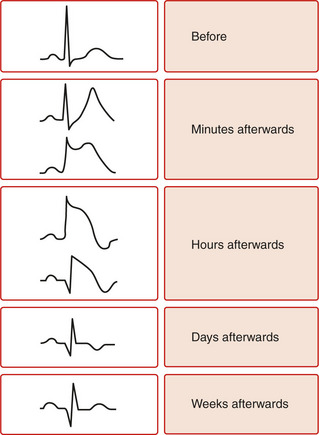
Fig. 13.4 Electrocardiographic evolution of ST-elevated myocardial infarction (STEMI). After the first few minutes, the T waves become tall, pointed and upright and there is ST segment elevation. After the first few hours, the T waves invert, the R wave voltage is decreased and Q waves develop. After a few days, the ST segment returns to normal. After weeks or months the T wave might return to upright but the Q wave remains.
This is difficult, but there is no evidence that using another agent, e.g. heparin, helps. Aspirin has been used but efficacy is not very good. Consideration should be given to treatment of the valvular lesion, which will include removal of clot from the left atrium and then DC cardioversion or drug therapy to control the rhythm.
Warfarin is teratogenic and should not be given in the first trimester, and women at risk of pregnancy should be warned to stop the drug very early. The use of anticoagulation in pregnancy is a very complicated problem and should only be done under careful supervision by people expert in the field. Anticoagulation is not necessary for a corrected VSD or coarctation of the aorta.
Duct-dependent circulation occurs in fetal life when there is no pulmonary circulation. The blood is diverted through the duct (that is, duct dependent) into the systemic circulation and is then re-oxygenated as it passes through the placenta. There is no comparable situation. Failure of ductal closure at birth results in persistent ductus arteriosus, which can lead to cardiac problems if not treated.
Ventilation-perfusion scan. A normal scan virtually excludes a pulmonary embolism. A ‘high probability’ scan indicates a 95% chance of a pulmonary embolism. A negative D-dimer assay excludes a pulmonary embolism. All of these investigations must be evaluated with the clinical features. If obtainable, a multi-slice CT has a high sensitivity of 83% and a specificity of 92% even with a small embolus
The diastolic pressure is of critical value and until fairly recently was the main target of treatment. This was because the diastolic pressure does not vary as much as the systolic and therefore clear guidance could be given that patients with a diastolic pressure 100mmHg should be treated; this value is now more usually 90mmHg. Recently, it has been realized that the systolic pressure is as important in the production of complications – both cerebrovascular and cardiac events.
Isolated systolic hypertension occurs frequently in the elderly 160mmHg and needs treatment (Table 13.1).
Table 13.1 British Hypertension Society classification of blood pressure levels
| Category | Systolic blood pressure (mmHg) | Diastolic blood pressure (mmHg) |
|---|---|---|
| Blood pressure | ||
| Optimal | <120 | <80 |
| Normal | <130 | <85 |
| High normal | 130–139 | 85–89 |
| Hypertension | ||
| Grade 1 (mild) | 140–159 | 90–99 |
| Grade 2 (moderate) | 160–179 | 100–109 |
| Grade 3 (severe) | >180 | >110 |
| Isolated systolic hypertension | ||
| Grade 1 | 140–149 | <90 |
| Grade 2 | >160 | <90 |
The classification equates with those of the European Society of Hypertension and the World Health Organization International Society of Hypertension and is based on clinical blood pressure and not values for ambulatory blood pressure measurement. Threshold blood pressure levels for the diagnosis of hypertension using self/home monitoring are greater than 135/85 mmHg. For ambulatory monitoring, 24-h values are greater than 125/80 mmHg. If systolic blood pressure and diastolic blood pressure fall into different categories, the higher value should be taken for classification.
The most recent advance in management reflects CT and MRI imaging, which show the effect of accelerated hypertension on the brain. In terms of treatment, the most important thing is not to reduce the pressure too quickly except in very urgent situations, e.g. a dissecting aneurysm. Here parenteral therapy is necessary. In other situations, oral hypotensive therapy only should be used. This can be with atenolol, labetalol or a calcium-channel blocker, e.g. amlodipine. Try to reduce pressure over 24 hours to between 100 and 110mmHg diastolic.
ACE inhibitors are thought to be the drug of choice for hypertension in the diabetic as they are renoprotective. Both reduce the risk of stroke. Often both drugs are needed for good control of hypertension. In non-diabetics, both are useful.
Many experts now advocate preoperative treatment (e.g. 2 hours before surgery) in medium- and high-risk patients. Many clinicians now use low-molecular-weight heparin, e.g. enoxaparin 40mg, rather than low-dose unfractionated heparin. Note: other prophylactic techniques, e.g. compression stockings, should also be used.
‘Aspirin resistance’ implies that aspirin does not inhibit tests of platelet function in vitro. This is unusual. The term is wrongly used to cover patients whose cardiovascular events are not helped by aspirin (treatment failure). Clopidogrel is used in these circumstances.




