14 Cardiothoracic surgery
Ischaemic heart disease
Epidemiology and aetiology
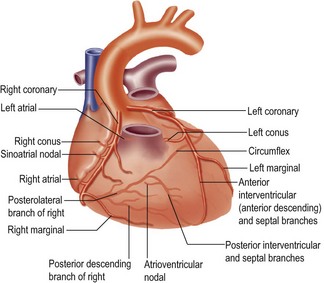
Ischaemic heart disease (IHD) includes all the consequences of narrowing or occlusion of the coronary arteries by atherosclerosis. These include angina, myocardial infarction and heart failure, arrhythmias and mitral valve incompetence. Myocardial infarction is the commonest cause of death in the UK. The risk factors and pathogenesis of atherosclerosis are the same as for peripheral vascular disease, discussed on page 203. The heart is supplied by the right and left coronary arteries. The left coronary artery is the bigger vessel and has a main stem 1 cm in length which divides into the left anterior descending artery and the circumflex artery (Fig. 14.1).
Clinical features
The manifestations of coronary artery disease vary depending on which vessels are affected and are summarised in Box 14.1.
Treatment
Risk factor modification and medical therapy
The modification of vascular risk factors is discussed in Chapter 13 on page 204. Medical therapy is aimed at reducing myocardial oxygen demand, but more severe disease requires coronary artery intervention by either angioplasty/stenting or coronary artery bypass grafting (CABG).
Coronary artery bypass grafting (CABG)
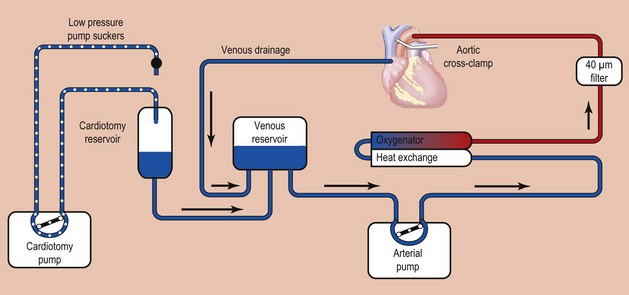
Coronary artery bypass graft is one of the most commonly performed major operations. Most are performed using cardiopulmonary bypass with hypothermia (Fig. 14.2).
Other procedures that may be carried out at the time of CABG include:
• left ventricular aneurysm excision (mortality 5%)
• mitral valve repair/replacement (mortality 15%)
• stroke (risk raised if carotid arteries stenosed)
• limb ischaemia/compartment syndrome (especially if intra-aortic balloon pump used perioperatively)
• wound problems from saphenous vein harvest
Stenting versus CABG for ischaemic heart disease
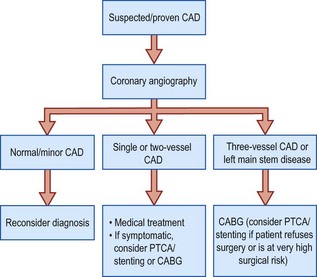
Indications for coronary bypass surgery are summarised in Box 14.2.
Box 14.2 Indications for coronary artery bypass surgery
Large clinical trials have shown that PTCA and stenting are effective in treating angina, with lower morbidity than surgery. However, the re-intervention rate is higher. CABG achieves better long-term survival, and is more effective in patients with triple vessel disease (Fig. 14.3).
Valvular heart disease
Infective/subacute infective endocarditis
This is a common condition which mainly affects aortic and mitral valves, and tricuspid in intravenous drug users. There is often an underlying valve abnormality (Table 14.1). The common organisms responsible are indicated in Table 14.2.
Table 14.1 Abnormalities associated with infective endocarditis
| Site | Abnormality |
|---|---|
| Aortic valve | Congenital bicuspid valveDegenerative valve diseaseRheumatic disease |
| Mitral valve | Rheumatic disease |
| Prolapsing valve | |
| Any prosthetic valve | Adherent thrombus |
| Congenital cardiac abnormalities | Patent ductus arteriosusSeptal defect |
Table 14.2 Organisms involved in infective endocarditis
| Bacterium | Antecedents | Pathological features |
|---|---|---|
| Streptococcus viridans | Dental extraction Other instrumentation: GI endoscopy, cystoscopy, bronchoscopy |
Often congenital abnormality of valve |
| Enterococcus | Prostatic disease Pelvic surgery |
Older patients |
| Staphylococcus aureus | Intravenous prostheses Drug addicts |
Acute ulcerative disease Abscess formation |
| Streptococcus epidermidis | Intravenous prostheses Drug addicts Artificial heart valves |
Low-grade disease |
| Fungal infection | Immunosuppression | Indolent disease |
Clinical features
Haemodynamic symptoms
• Low cardiac output – fatigue, lethargy, shortness of breath on exertion
• Aortic stenosis – syncope and angina
• Pulmonary congestion – any combination of stenosis or regurgitation of the left-sided heart valves causes breathlessness on exertion, cough, frothy sputum and haemoptysis
• Right heart failure – fatigue, headache, right upper quadrant pain from liver congestion, ascites, ankle swelling.
Physical signs of valvular disease
General examination reveals many signs of heart disease, especially right heart failure (cyanosis, pitting ankle oedema, liver enlargement). If the JVP is high, it may be necessary to sit the patient up more than the usual 45° (Table 14.3). Thrills, displacement of the apex and sternal lifting may be detected on examination of the precordium. Auscultation should proceed methodically over the aortic, pulmonary, tricuspid and mitral valve areas, listening for the heart sounds and any murmurs.
Table 14.3 Features of physical examination of peripheral circulation in heart disease
| Feature | Findings | Significance |
|---|---|---|
| Fingers and hands | Cool Capillary pulsation Splinter haemorrhages Clubbing |
Low cardiac outputAortic regurgitationBacterial endocarditisCyanotic heart disease |
| Arm pulse | Low amplitude High amplitude Jerking Double pulse |
Low cardiac output Aortic regurgitation Aortopulmonary shunt CO2 retention Cardiomyopathy Mixed aortic stenosis/aortic regurgitation |
| Carotid pulse | Slow rising; low amplitude Bouncing full Head nods Systolic murmur Systolic thrill |
Aortic stenosis Aortic regurgitation Aortic regurgitation Referred from aortic stenosis Carotid artery stenosis Carotid artery stenosis |
| Neck veins | High jugular pressure (JVP) | Congestive heart failure Right ventricular failure Tricuspid regurgitation Tamponade (JVP rises on inspiration) Constrictive pericarditis |
Investigations
• Blood tests – ESR, Hb, CRP, blood cultures
• ECG – left ventricular hypertrophy often seen in aortic valve disease, atrial fibrillation in mitral valve stenosis
• Echocardiography (transthoracic or transoesophageal) – the most widely used and useful method for investigating valve function
• Angiography – allows measurement of pressure gradients and assessment of coexisting coronary artery disease.
Treatment
Indications for surgery include:
• pressure gradients >50 mmHg across aortic valve, or >10 mmHg across mitral valve
• ventricular decompensation (dilating left or right ventricle shown by serial CXRs or echocardiography)
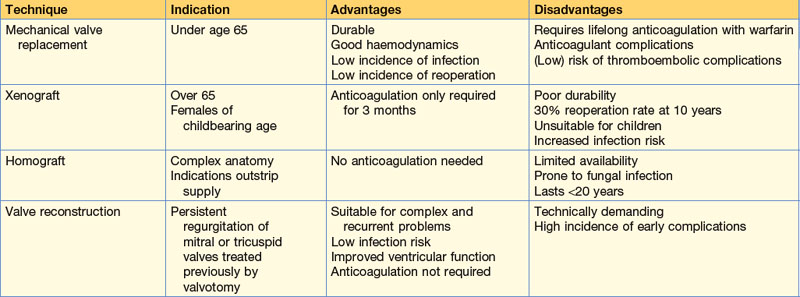
The operative options and their relative merits are indicated in Table 14.4.
Congenital heart disease
Congenital heart defects affect around 1 in 100 live births and result in 40 operations per million population per year in the UK. The commonest lesion is a ventricular septal defect (Box 14.3). The causes are multifactorial and include rubella (persistent ductus arteriosus and pulmonary valve stenosis), maternal alcohol abuse (septal defects), maternal drug and radiation treatment and genetic and chromosomal abnormalities (e.g. Down’s syndrome).
Cardiomyopathy
Cardiac transplantation
Retrieval, tissue typing, transplantation ethics and immune suppression
These topics are all discussed in Chapter 12, pages 196–199.
Operation
The recipient’s heart is removed, leaving atrial cuffs in situ, to which the donor atria are then sutured. The pulmonary artery and aortic anastomosis are then completed. See Table 14.5 for prognosis.
| 1 year | 72% |
| 3 years | 67% |
| 5 years | 62% |
Carcinoma of the bronchus
Epidemiology, aetiology and pathology
Benign lung tumours
‘Surgical’ lung infections
Pneumothorax
Aetiology
Traumatic pneumothorax is discussed on page 63. Spontaneous pneumothorax has three main causes:
Pathology
As air enters the pleural cavity the lung collapses. With both spontaneous and traumatic pneumothorax, if air continues to leak out of the lung with each breath, since there is no route for it to escape, the pressure in the pleural cavity increases, causing a tension pneumothorax (see p. 63).
Mediastinoscopy and thoracoscopy
Indications for diagnostic and therapeutic chest endoscopic procedures are summarised in Table 14.7.
Table 14.7 Indications for diagnostic and therapeutic thoracoscopy
| Diagnostic | |
| Problem | Possible diagnosis |
| Pleural effusions | Malignancy, tuberculosis, lymphoma |
| Pleural nodules/thickening | Mesothelioma, tuberculosis, malignancy, fibromas |
| Diffuse parenchymal lung disease | Sarcoid, lymphoma, HIV-related conditions, opportunistic infections, granulomas |
| Staging of lung cancer | Mediastinal and hilar node sampling |
| Lung nodules | Primary or secondary tumours, granulomas, including tuberculosis |
| Therapeutic | |
| Indication | Procedure |
| Empyema | Drainage and breakdown loculi |
| Recurrent pneumothorax | Pleurectomy or pleural abrasion (talc) Stapling of apical bullae |
| Pericardial effusion | Creation of pericardial to pleural window |
| Malignant effusion | Pleurectomy or talc or tetracycline pleurodesis |
| Lung masses | Resection as wedge or lobectomy |