Chapter 1 Cardiopulmonary resuscitation
Cardiopulmonary resuscitation (CPR) is one of the most difficult areas in clinical medicine and outcomes are often said to be extremely poor, especially in patients with unwitnessed out-of-hospital cardiac arrest. While many accepted practices do not yet have a strong evidence base, a number of principles can now reasonably be supported. Any attempt at resuscitation is worthwhile and, although some recommendations have changed, it is acceptable and appropriate that staff or bystanders trained in using previous practices use their known skills.
Despite the difficulties in performing research in this area, the body of evidence is growing and new concepts such as circulatory support alone (chest compression without active ventilation), devices and techniques to provide more effective external chest compression, devices for minimally invasive internal cardiac massage and improved technology for electrical therapy (biphasic cardioversion) are under investigation. Recent work suggests controlled hypothermia may improve neurological outcome post-arrest in some patients. Broader public education, improved telecommunications and increased availability of defibrillators have also had considerable impact.
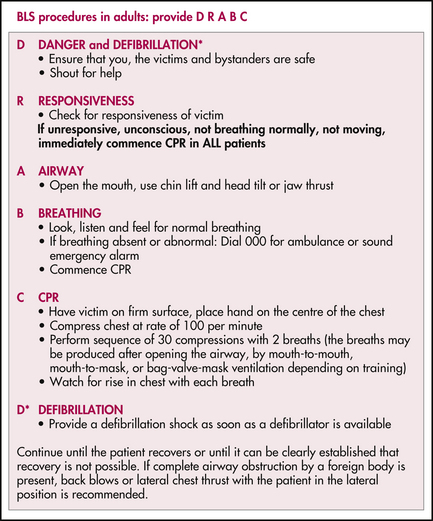
BASIC LIFE SUPPORT (BLS)
RESUSCITATION OF THE NEWBORN
If the baby has not started breathing or the heart rate is < 100 bpm, provide positive pressure ventilation with a self-inflating 240-mL neonatal resuscitation bag. Oxygen can be added if there is no improvement after the first few minutes. Use a soft-rimmed mask that covers the mouth and nose, but not the eyes. Keep the head in a neutral position as extension or flexion can kink and obstruct the airway.
Intubation can then be performed if there is an experienced operator available.
| Drug | Strength | IV/IO dose |
|---|---|---|
| Adrenaline | 1:10,000 | 0.1 mL/kg (10 μg/kg) |
| Sodium bicarbonate | 8.4% | 1 mL/kg (1 mmol/kg) |
| Dextrose | 10% | 2 mL/kg |
| Fluid/volume | Normal saline (or blood if indicated) | 10 mL/kg |
| Naloxone (Only if indicated and note the short half-life) | 400 μg/mL | 0.25 mL/kg (100 μg/kg) |
RESUSCITATION OF CHILDREN
Although bradycardia and asystole are common initial rhythms in paediatric cardiac arrest, primary cardiac disease is not often the cause. Hypoxaemia and hypotension are more common and may have been present for some time leading up to the arrest.
| BLS in children |
FOREIGN BODY AIRWAY OBSTRUCTION
Place the baby or infant prone and head down across the lap. Deliver firm blows with the heel of your hand to the baby’s back between the shoulder blades. Deliver up to five blows, checking in between to see if the airway has been cleared. If not successful, turn the infant over and perform up to five chest thrusts. These are sharp blows delivered to the lower sternum (the same location as for chest compressions in BLS). Again, assess in between blows for success.
ADVANCED LIFE SUPPORT (ALS) IN CHILDREN
A heart rate of less than 60 bpm in an infant (< 1 year) or less than 40 bpm in a child (< 8 years) should be regarded as cardiac arrest. Treat asystole, low output/severe bradycardia or pulseless electrical activity with adrenaline 10 μg/kg IV/IO every 2–5 minutes. Seek and treat any reversible causes (refer to Box 1.2). Administer 20 mL/kg fluid bolus. Consider sodium bicarbonate 1 mmol/kg IV/IO and atropine 20 μg/kg IV/IO. Pacing may be of value in rare cases.
Defibrillate ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) immediately. If the arrest was witnessed, up to three (‘stacked’) shocks can be delivered in quick succession. The initial energy level is 2 J/kg but deliver all subsequent shocks at 4 J/kg, rounding up to the nearest energy level. Then initiate 2 minutes of CPR before analysing the rhythm again and delivering a single shock of 4 J/kg, if indicated. Adrenaline 10 μg/kg IV/IO can be administered every 2–5 minutes. Persistent or refractory VF or VT may also be treated with amiodarone 5 mg/kg IV/IO, which may be repeated. Also consider sodium bicarbonate 1 mmol/kg IV/IO, magnesium sulfate 0.05–0.1 mmol/kg IV/IO, potassium chloride 0.05 mmol/kg IV/IO. Seek and treat any reversible causes (refer to Box 1.2).
RESUSCITATION OF ADULTS
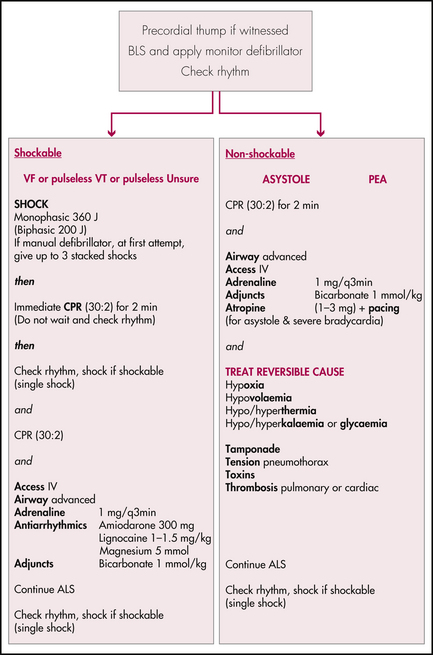
ADULT ADVANCED LIFE SUPPORT (ALS)
Administer adrenaline 1 mg every 2–5 minutes. The intravenous route is ideal. The intraosseous route is now preferable to the endotracheal route
EDITOR’S COMMENT
This vital skill is undergoing rapid change as the search for better outcomes continues. The key to good results is a prompt and orderly approach. An airway and early, effective and uninterrupted chest compressions are proving to be very important in improving outcome in adult cardiac arrest. In the future, to simplify BLS for lay or uncertain responders, the guidelines for adults may include compression only, i.e. no expired air resuscitation.