CHAPTER 3 Cardiac Intensive Care Unit Admission Criteria
Cardiovascular disease (CVD) accounted for 36.3% of all deaths in the United States in 2004.1 Nearly 2400 Americans die of CVD each day, an average of 1 death every 36 seconds. The United States leads the world in spending on health care, whether measured as a percentage of gross domestic product or as dollars per capita.2 Despite this cost, cardiac intensive care unit (CICU) beds remain a limited resource. There is evidence that physicians can safely adapt to substantial reductions in the availability of CICU beds.3 Determining the appropriateness for admission to the CICU can be challenging, however, and has been the subject of study since the early 1980s.4,5
Many disease processes typically lead to admission to the CICU (Table 3-1). This chapter discusses these conditions and the rationale for intensive care in their treatment.
Table 3–1 Cardiovascular Conditions Requiring Admission to the Cardiac Intensive Care Unit
| Chest pain, acute coronary syndromes, and acute myocardial infarction |
| Acute decompensated heart failure |
| Pulmonary hypertension |
| Arrhythmias |
| Sudden cardiac death |
| Cardiogenic shock |
| Conditions requiring IABP or other forms of mechanical circulatory support |
| Adult congenital heart disease (decompensated) |
| Valvular heart disease (with hemodynamic instability) |
| Aortic dissection |
| Hypertensive emergency |
| Cardiac tamponade |
| Pulmonary embolism (massive or submassive) |
| Postprocedure monitoring (percutaneous coronary intervention and electrophysiologic study) |
IABP, intra-aortic balloon pump.
History
The first description of the coronary care unit (CCU) was presented to the British Thoracic Society in July 1961.6 CCUs were initially established in the early 1960s in an attempt to reduce mortality from acute myocardial infarction (MI). The ability to abort sudden death from malignant ventricular arrhythmias in the post-MI setting led to the continuous monitoring of cardiac rhythm and an organized system of cardiopulmonary resuscitation, including external defibrillation.7 An early experience of patients with acute MI treated in the CCU published in 1967 showed that patients treated in the CCU had better survival rates compared with other patients with acute MI in the absence of cardiogenic shock.8 With creation of Myocardial Infarction Research Units in the United States by the National Heart, Lung and Blood Institute and evolving technologies, the foundation was in place for the CCU to expand into the modern-day CICU where comprehensive advanced care is provided for many cardiovascular conditions. The CICU has been called one of cardiology’s 10 greatest discoveries of the 20th century.9
Diagnoses
Chest Pain and Acute Coronary Syndromes, and Acute Myocardial Infarction
Chest pain accounts for approximately 6 million annual visits to emergency departments in the United States, making chest pain the second most common complaint in the emergency department.10 ACS are life-threatening causes of chest pain seen in the emergency department and include unstable angina, non–ST segment elevation MI (NSTEMI), and acute MI or ST segment elevation MI. Less than 15% to 30% of patients who present to the emergency department with nontraumatic chest pain have ACS, however.11,12 An important challenge is to identify patients with ACS appropriately and admit them to the appropriate setting for further care. For the evaluation and management of patients with acute chest pain, prediction models have markedly improved our ability to estimate risk, and cost-effectiveness analyses have helped guide the development of new paradigms and the incorporation of new technologies.13
In addition to treating patients with ACS, the CICU has traditionally been considered appropriate for monitoring patients with acute chest pain until ACS is diagnosed or excluded. Increasing health care costs have created pressures, however, to increase the efficiency of CICUs. Possible strategies seek to decrease resource use by identifying low-risk patients for initial triage or early transfer to lower levels of care. The application of management algorithms and the development of intermediate care units are allowing for a distinction between intensive coronary care and careful coronary observation.14 The development of chest pain units located in the emergency department is an another alternative to CICU admission. These units are safe, effective, and a cost-saving means of ensuring that patients with unstable angina who are considered to be at intermediate risk of cardiovascular events receive appropriate care.15 Patients at low clinical risk can receive immediate exercise testing in the chest pain unit if the appropriate diagnostic modalities are available. This approach is accurate for discriminating low-risk patients who require admission from patients who can be discharged to further outpatient evaluation.16
Several reports have detailed strategies to identify high-risk patients early. To achieve more appropriate triage to the CICU of patients presenting with acute chest pain, Goldman and coworkers17 used clinical data on 1379 patients at two hospitals to construct a computer protocol to predict the presence of MI. This protocol was tested prospectively, and it had a significantly higher specificity (74% versus 71%) in predicting the absence of infarction than physicians deciding whether to admit patients to the CICU, and it had a similar sensitivity in detecting the presence of infarction (88% versus 87.8%). Decisions based solely on the computer protocol would have reduced the admission of patients without infarction to the CICU by 11.5% without adversely affecting the admission of patients in whom emergent complications developed that required intensive care.
In another study,18 the acute cardiac ischemia time-insensitive predictive instrument (ACI-TIPI) was used to triage patients with symptoms suggestive of acute cardiac ischemia to the CICU, telemetry unit, ward, or home. Use of ACI-TIPI was associated with reduced hospitalization among emergency department patients without acute cardiac ischemia. Appropriate admission for unstable angina or acute infarction was not affected. If ACI-TIPI is used widely in the United States, its potential incremental impact is estimated to be more than 200,000 fewer unnecessary hospitalizations and more than 100,000 fewer unnecessary CICU admissions.18
In a cost-effectiveness analysis, Fineberg and colleagues19 found that for patients with a 5% probability of infarction, admission to a CICU would cost $2.04 million per life saved and $139,000 per year of life saved compared with intermediate care. For the expected number of such patients annually in the United States, the cost would be $297 million to save 145 lives.
In another study by Goldman and associates,20 a set of clinical features was defined; if these features were present in the emergency department, they were associated with an increased risk of complications. These clinical features included ST segment elevation or Q waves on the electrocardiogram (ECG) thought to indicate acute MI, other ECG changes indicating myocardial ischemia, low systolic blood pressure, pulmonary rales above the bases, or an exacerbation of known ischemic heart disease. The risk of major complications in patients with acute chest pain can be estimated on the basis of the clinical presentation and new clinical observations made during the hospital course. These estimates of risk help in making rational decisions about the appropriate level of medical care for patients with acute chest pain.
Despite these findings, the implementation of these algorithms in clinical practice by physicians without specific training in their use has been minimal.21,22 This situation may relate to physicians’ reporting that they are too busy, are unsure of the value of the algorithms, and are concerned about the consequences of inappropriately discharging patients who are later found to have had MI.23
A more recent analysis by Tosteson and colleagues24 indicates that the CICU usually should be reserved for patients with a moderate (≥21%, depending on the patient’s age) probability of acute MI, unless patients need intensive care for other reasons. Clinical data suggest that only patients with ECG changes of ischemia or infarction not known to be old have a probability of acute MI this high. A summary has been developed that outlines the location to which chest pain patients should be admitted (Table 3-2).25
Table 3–2 Indications to Guide Where to Admit Patients with Acute Chest Pain
ECG, electrocardiogram.
Adapted from Lee TH, Goldman L: Evaluation of the patient with acute chest pain. N Engl J Med 2000;342:1187-1195.
Another important issue to consider is the length of stay in the CICU after patients are admitted. If patients are initially triaged to the CICU, the lack of cardiac enzyme abnormalities or recurrent chest pain during the first 12 hours of hospitalization are parameters that can be used to identify patients for whom a 12-hour period of CICU observation is sufficient to exclude acute MI.26 In a study by Weingarten and colleagues,27 physicians caring for patients with chest pain who were at low risk for complications received personalized written and verbal reminders regarding a guideline that recommended a 2-day hospital stay. Use of the practice guideline recommendation with concurrent reminders was associated with a decrease in length of stay from 3.54 ± 4.1 days to 2.63 ± 3 days and a total cost reduction of $1397 per patient. No significant difference was noted in complications, patient health status, or patient satisfaction when measured 1 month after hospital discharge.
The European Society of Cardiology and American College of Cardiology restructured the definition of acute MI in 2000 (Table 3-3).28 The principal revision compared with the previous World Health Organization definition29 is the inclusion of biomarkers, specifically troponin, as a necessary component. There have been some attempts to assess the new definition and the widespread introduction of troponin measurement on CICU admitting practices. One study by Amit and colleagues30 was a retrospective cohort study in which all admissions to the CICU the year before and after the introduction of troponin measurement and the updated MI definition were examined. There was a 20% increase in the number of CICU admissions, driven by a 141% increase in the number of NSTEMIs. Length of stay in the CICU decreased by 1 day for all ACS patients, and the 30-day mortality for acute MI did not change significantly. In another study by Zahger and associates,31 the number of NSTEMI patients increased by 33% after the definition change, whereas the number of patients with ST segment elevation MI remained the same. There was no change in the number of CICU beds at the participating institutions. The proportion of patients given the diagnosis of NSTEMI increased significantly more in centers with high use of troponin. These changes have a significant impact on resource use.
Table 3–3 European Society of Cardiology/American College of Cardiology Definition of Acute, Evolving, or Recent Myocardial Infarction
Adapted from Antman E, Bassand J-P, Klein W, et al: Myocardial infarction redefined—a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 2000;36:959-969.
Given this increased demand for a relatively fixed resource, the question of whether all NSTEMI patients need to be admitted to the CICU arises. The CRUSADE registry32 showed that patients with NSTEMI often receive excess doses of antithrombotic therapy, and that dosing errors occur more often in vulnerable populations and predict an increased risk of major bleeding. Some institutions have interpreted these data to indicate that all NSTEMI patients should be admitted to the CICU because a maximally observed setting may limit excess dosing and bleeding complications.
At our institution, it is practice for only NSTEMI patients who are high risk by the TIMI risk score33 to be admitted to the CICU. The lower risk NSTEMI patients are admitted to a telemetry unit with cardiac nurses. There is preliminary evidence that admission of patients with initially uncomplicated chest pain with a relatively low probability of acute MI to a stepdown unit does not place at increased risk those who eventually “rule in” for MI.34 Regardless of specific setting, the adherence to clinical pathways offers the potential to improve the care of patients with ACS while reducing the cost of care.35
Heart Failure
It is estimated that 5.2 million people in the United States are being treated for heart failure.1 Hospital discharges for heart failure increased from 402,000 in 1979 to 1,101,000 in 2004.36 Interventions to improve adherence, the control of hypertension, and the appropriate use of angiotensin-converting enzyme inhibitors may prevent many hospitalizations of heart failure patients.37 Device therapy, including biventricular pacemakers and implantable cardioverter-defibrillators, has also led to significant improvements in outcomes for certain heart failure patient populations.38,39 Nonetheless, some patients admitted to the hospital with heart failure require advanced cardiac care in the CICU. Standard criteria for management of acute decompensated heart failure (ADHF) in the CICU are not clearly established. Management usually involves invasive hemodynamic monitoring and inotropic or vasopressor support that cannot be done outside the CICU in most institutions.
Admission for heart failure is a high-risk event for patients, particularly patients admitted to an intensive care unit (ICU) setting.40 Table 3-4 shows the events and procedures that occurred during hospitalization of patients with congestive heart failure (CHF) in the ADHERE registry.
Table 3–4 Events and Procedures for Congestive Heart Failure Patients during Hospital Stay
| Event or Procedure | All Patients (N = 105,388) (%) | ICU/CICU Patients (n = 19,754) (%) |
|---|---|---|
| Death | 4 | 11 |
| Defibrillation or CPR | 1 | 6 |
| Mechanical ventilation | 5 | 23 |
| Intra-aortic balloon pump | <1 | 2 |
| Pulmonary artery catheter | 5 | 17 |
| Dialysis | 5 | 19 |
| New-onset dialysis | 1 | 3 |
| Electrophysiologic study | 4 | 5 |
| Cardiac catheterization | 10 | 20 |
| With PCI | 81 | 78 |
CPR, cardiopulmonary resuscitation; PCI, percutaneous coronary intervention.
Adapted from Adams KF Jr, Fonarow GC, Emerman CL, et al; ADHERE Scientific Advisory Committee and Investigators: Characteristics and outcomes of patients hospitalized for heart failure in the United States: Rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J 2005;149:209-216.
Weingarten and associates41 found that nearly one third of patients with CHF hospitalized in either the CICU or intermediate care unit are lower risk and potentially suitable for transfer 24 hours after admission. In this study, low risk is defined as patients without acute MI or ischemia, active or planned cardiac interventions, unstable comorbidity, worsening clinical status, or lack of response to diuretic therapy. A more common planned cardiac intervention for heart failure patients is the use of the pulmonary artery catheter. Although addition of the pulmonary artery catheter to careful clinical assessment increases anticipated adverse events, it does not affect overall mortality and hospitalization in patients with severe symptomatic and recurrent heart failure.42
In most hospitals, certain medical therapies used in the treatment for decompensated heart failure are delivered in the CICU setting. The need for pronounced afterload reduction is an indication for intravenous nitroprusside.43 This therapy is commonly delivered in the CICU because it requires continuous blood pressure monitoring. The major limitation to the use of nitroprusside is its metabolism to cyanide, possibly leading to development of cyanide toxicity or rarely thiocyanate toxicity that may be fatal.44
Patients with systolic dysfunction who remain volume-overloaded despite vasodilator and diuretic therapy may require intravenous inotropic support to improve systemic perfusion. The β agonist dobutamine is a useful inotropic agent for ADHF.45 In patients with severe CHF, short-term administration of dobutamine selectively improves vascular endothelial function.46 Another class of inotropic agents commonly used is the phosphodiesterase inhibitors. In addition to being given in the acute setting, prolonged outpatient therapy with milrinone, a phosphodiesterase inhibitor, has been employed.47 The use of intravenous continuous infusion of inotropes, including dobutamine and milrinone, has not been shown to have a benefit in mortality.48
Another treatment modality that has been used in the CICU or cardiac stepdown unit is the exogenous administration of nesiritide, recombinant human brain natriuretic peptide. In patients hospitalized with ADHF, nesiritide improves hemodynamic function.49 More recent independent analyses have questioned the safety of nesiritide, however. Compared with non–inotrope-based control therapy, nesiritide may be associated with an increased risk of worsening renal function50 and death51 after treatment for ADHF. If used, these treatments are best used in the CICU or cardiac stepdown unit to achieve hemodynamic targets.
Certain causes of heart failure require specific therapies. Patients with giant cell myocarditis have improved outcomes if they receive immunosuppressive treatment.52 Patients with a fulminant presentation from giant cell myocarditis, or more rarely from other etiologies such as lymphocytic or viral myocarditis, require an intensive level of hemodynamic support with inotropes and vasopressors in the CICU.53
Patients receiving inotropic therapy can go on to have improved outcomes with the use of mechanical circulatory support, specifically left ventricular assist devices (LVADs), as destination therapy.54 Although cellular recovery and improvement in ventricular function are observed, the degree of clinical recovery is insufficient for device explantation in most patients with chronic heart failure.55 If not used as destination therapy, the LVAD may serve as a bridge to heart transplantation, and these patients are cared for in the cardiothoracic surgery ICU after surgery. Also, at cardiac transplantation centers, some advanced CHF patients require continuous infusion of a single high-dose intravenous inotrope (e.g., dobutamine, ≥7.5 μg/kg/min, or milrinone, ≥0.50 μg/kg/min), or multiple intravenous inotropes, in addition to continuous hemodynamic monitoring of left ventricle filling pressures, which satisfies criteria for listing as Status 1A by the United Network of Organ Sharing.56 Additionally, patients undergoing new advanced cardiac care procedures, such as percutaneous mechanical devices,57 require management in the CICU.
Multiorgan dysfunction in the setting of heart failure requires admission to the CICU. A reduced glomerular filtration rate is associated with an increased mortality in patients with heart failure.58 Because many patients with ADHF and renal failure have compromised hemodynamics, a form of renal replacement therapy, such as continuous venovenous hemofiltration or hemodialysis, in the intensive care setting is commonly required. Other volume management techniques for heart failure treatment, such as ultrafiltration,59 may necessitate care in the CICU or stepdown unit.
While the patient is hospitalized, careful attention to certain laboratory values such as serum sodium and blood urea nitrogen is reasonable because both values have been shown to be independent predictors of subsequent mortality.60,61 Treatment with tolvaptan, a vasopressin V2 receptor blocker, has been shown to increase serum sodium concentrations effectively in patients with euvolemic or hypervolemic hyponatremia,62 but has no effect on long-term mortality or heart failure–related morbidity.63
Pulmonary Hypertension
Several treatments for pulmonary arterial hypertension are approved in the United States, including epoprostenol, treprostinil, bosentan, and sildenafil. Because limited data are available from head-to-head comparisons of approved therapies, the choice of treatment is dictated by clinical experience and by patients’ preferences.64 There are no evidence-based guidelines on when to admit patients with pulmonary hypertension to the CICU. Generally, patients with New York Heart Association or World Health Organization functional class IV may require an intensive care setting for management. Intravenous epoprostenol is an advanced pulmonary hypertension therapy that has been shown to improve functional capacity and survival in patients with idiopathic pulmonary arterial hypertension.65 In addition to vasoreactivity testing in the cardiac catheterization laboratory, inhaled nitric oxide is sometimes used in acutely ill patients with severe pulmonary hypertension in the CICU.66
Arrhythmias
Narrow-complex tachycardias can lead to unstable hemodynamics. In this situation, immediate synchronized cardioversion is indicated.67 This is best done in the controlled setting of a CICU if possible. If a patient is out of the hospital or in a less monitored unit, admission or transfer to the CICU should be arranged for further management.
Wide-complex tachycardias may represent either supraventricular or ventricular arrhythmias. The mechanism of wide-complex tachycardias can be determined with clinical information and analysis of the 12-lead surface ECG.68 Regardless of the cause, a wide-complex tachycardia that is unstable and associated with hemodynamic compromise must be treated promptly with electrical cardioversion. Pulseless ventricular tachycardia or ventricular fibrillation requires immediate defibrillation. Admission to the CICU may be required even in patients with implantable cardioverter-defibrillators. Electrical storm, or three or more appropriate shocks delivered because of repeated episodes of ventricular tachycardia or ventricular fibrillation occurring within a 24-hour period, often requires antiarrhythmic medical therapy to suppress arrhythmias and further shocks. In the AVID cohort, electrical storm was a significant independent risk factor for nonsudden cardiac death.69
More recently, the American College of Cardiology/American Heart Association/European Society of Cardiology updated their guidelines for the management of ventricular arrhythmias and the prevention of sudden cardiac death.70 For successfully resuscitated cardiac arrest victims, whether the event occurred in or out of the hospital, post–cardiac arrest care includes admission to an ICU and continuous monitoring for 48 to 72 hours.71 The outcome of patients experiencing sudden cardiac death remains poor. In the Seattle series, survival to hospital discharge for patients treated between 1998-2001 was not significantly better than for patients treated between 1977-1981.72 Protocols involving induction of hypothermia after return of spontaneous circulation phase in the ICU have been associated with improved functional recovery and reduced cerebral histologic deficits in various animal models of cardiac arrest. Additional promising preliminary human studies have been completed.73
Bradyarrhythmias that require temporary transvenous pacing are an acceptable indication for admission to the CICU. Indications for temporary pacing are less clearly described than the indications for permanent pacing. Table 3-5 lists recommendations by class of evidence for transvenous pacing in the setting of acute MI, which includes several bradyarrhythmias.74 Regardless of level of evidence, in practice patients who receive temporary transvenous pacemakers should be admitted to the CICU. Monitoring in the CICU should continue until the acute and reversible cause of the bradyarrhythmia is corrected, or a permanent pacemaker is placed.
| Class I |
AV, atrioventricular; BBB, bundle branch block; LAFB, left anterior fascicular block; LPFB, left posterior fascicular block; MI, myocardial infarction; VT, ventricular tachycardia.
Adapted from Ryan TJ, Anderson JL, Antman EM, et al: ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). J Am Coll Cardiol 1996;28:1328-1428.
Withdrawal of pacemaker or implantable cardioverter-defibrillator support at the end of life is becoming a more frequently encountered clinical scenario. Granting terminally ill patients’ requests to remove unwanted medical support is legal and ethical.75 An analysis by Lewis and coworkers76 showed that only one third of terminally ill patients with ICDs actually had shock therapy withdrawn as part of a comfort care strategy.
Cardiogenic Shock
Cardiogenic shock is the most severe form of left ventricular failure. It can occur as a complication of acute MI or from other cardiovascular conditions (Table 3-6).77 For the acute MI subgroup, the CICU is used for temporizing measures, such as intra-aortic balloon pump (IABP) counterpulsation and use of vasopressor support. These patients benefit from early revascularization with a mortality benefit at 6 months78 that persists at 6 years of follow-up.79 The use of early intravenous β blocker therapy in patients admitted to the CICU with acute MI complicated by unstable hemodynamics reduces the risk of reinfarction and ventricular fibrillation, but increases the risk of cardiogenic shock during the first day after admission.80 Appropriately selected patients with acute cardiogenic shock in the setting of acute MI managed in the CICU have had encouraging initial experiences with use of ventricular assist devices.81
| Complications of Acute Myocardial Infarction |
| Extensive left ventricular infarction |
| Extensive right ventricular infarction |
| Ventricular septal rupture |
| Acute severe mitral regurgitation |
| Cardiac tamponade with or without free wall rupture |
| Other Conditions |
| Aortic dissection |
| Myocarditis |
| Massive pulmonary embolism |
| Critical valvular stenosis |
| Acute mitral or aortic regurgitation |
| Calcium channel blocker or β blocker overdose |
Adapted from Tschopp D, Mukherjee D: Complications of myocardial infarction. In Griffin BP, Topol EJ (eds): Manual of Cardiovascular Medicine, 2nd ed. Philadelphia, Lippincott Williams & Wilkins, 2004, pp 45-63.
Other Indications for Intra-Aortic Balloon Pump
Other indications for IABP placement are clinical situations where admission to the CICU is necessary. IABP may be useful in a high-risk or complicated percutaneous coronary intervention (PCI),82 rescue PCI after failed thrombolysis,83 and acute MI with mechanical complications such as acute ventricular septal defect and mitral regurgitation.84 The prophylactic placement of an IABP before coronary artery bypass graft surgery has been performed in patients with left main coronary artery stenosis, severely depressed left ventricular systolic function, diffuse coronary artery disease, and redo surgery.85,86
Adult Congenital Heart Disease
The total population of adult congenital heart disease patients in the United States in 2000 was 785,000.87 This number, which exceeds the number of pediatric cases, reflects tremendous advances in pediatric cardiac care. Adult congenital heart disease patients may require management in the CICU. The need for CICU care is commonly due to the main consequences of congenital cardiac lesions: cyanosis, congestive heart failure, pulmonary hypertension, Eisenmenger syndrome, and cardiac arrhythmias. These patients are best cared for by a multidisciplinary team at designated adult congenital heart disease centers.88
Valvular Heart Disease
Patients with acute mitral regurgitation are often critically ill with significant hemodynamic abnormalities. In most cases, definitive treatment is surgery, but medical therapy in the CICU is needed to support the patient initially. Intravenous nitroprusside can reduce mitral regurgitation leading to increased forward cardiac output and diminished pulmonary congestion.89 Nitroprusside should not be given as monotherapy in patients who are hypotensive at presentation. Some benefit may be achieved initially by concurrent administration of an inotropic agent such as dobutamine, but an IABP is often inserted.90
Acute aortic insufficiency is a valvular condition that can require management in the CICU. The two most common causes of acute aortic insufficiency are endocarditis and aortic dissection.91 Treatment of acute severe aortic insufficiency is emergency aortic valve replacement. If there is any delay in surgery, stabilization may be attempted in the ICU using intravenous vasodilators, such as nitroprusside, and possibly inotropic agents, such as dopamine or dobutamine, in an attempt to enhance forward flow and lower left ventricular end-diastolic pressure.90 An IABP is contraindicated because inflation of the balloon in diastole would worsen the severity of aortic insufficiency.
A special consideration is acute valvular disease in the setting of infective endocarditis. Surgery in native valve endocarditis is sometimes delayed to allow a longer duration of antibiotic therapy; however, several studies support the use of early surgery in patients with acceptable indications.92,93 The decision as to when to operate is often difficult and requires close consultation with surgical colleagues for each case.
Patients with severe aortic stenosis and hemodynamic instability are managed in the CICU. If the patients are high risk for aortic valve replacement, percutaneous balloon valvuloplasty has been performed. This procedure has been shown to reduce aortic valve gradient, but morbidity and mortality remain high in this population.94 The 2006 American College of Cardiology/American Heart Association guidelines for management of patients with valvular disease90 concluded that balloon valvuloplasty is not a substitute for valve replacement in adults. The guidelines do recognize the above-mentioned situation as a setting in which balloon valvuloplasty may be reasonable. Its use for palliation in patients with serious comorbid conditions that prevent performance of aortic valve replacement is also a reasonable exception. These patients require intensive management in the CICU during the periprocedure time period. Two catheter-based techniques for replacing the aortic valve have also been investigated: percutaneous implantation via a retrograde femoral approach and direct apical puncture. These techniques are currently experimental, and more experience is required before either approach can be recommended for routine clinical practice.95–97
Aortic Disease
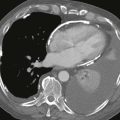
Patients with uncomplicated aortic dissections confined to the descending thoracic aorta (Stanford type B or DeBakey type III) are best treated with medical therapy in the ICU.98 The acute management usually involves an intravenous β blocker, plus an intravenous vasodilator such as nitroprusside if further blood pressure lowering is needed to minimize aortic wall stress.99 Pain control is also an important component of treatment. Patency or thrombosis of the false lumen has been found to have prognostic implications. Partial thrombosis of the false lumen, compared with complete patency, is a significant independent predictor of postdischarge mortality in patients with type B acute aortic dissection.100
Patients with aortic intramural hematoma of the ascending aorta are at high risk for early progression to overt dissection and rupture and require undelayed surgical repair.101 Acute aortic dissection of the ascending aorta, or type A dissection, is highly lethal, with a mortality rate of 1% to 2% per hour after the onset of symptoms.102 Although the definitive treatment for type A dissections is emergent surgery, medical therapy including intravenous β blockade to reduce blood pressure and the force of left ventricular ejection is needed initially as the diagnosis is confirmed.99
Hypertensive Emergency
Although there have been many advances in antihypertensive therapy, only 31% of patients with diagnosed hypertension have adequate blood pressure control.103 Adherence to therapy remains a problem104 and contributes to poor blood pressure control that can lead to hypertensive emergency. Nonadherence to medical therapy is the most common reason patients present to the emergency department with hypertensive crises.105 Multiple classes of intravenous antihypertensive medications, including vasodilators, adrenergic inhibitors, and diuretics, are available for use in the CICU for the treatment of hypertensive emergency.106 Intravenous infusion of nitroprusside is effective, reliable, and safe in this situation.107 Labetalol is used parenterally for rapid control of blood pressure in hypertensive emergencies.108 Although useful as adjunctive therapy in hypertensive crises, diuretics should be used with caution if volume depletion is suspected.109 The continuous infusion of parenteral antihypertensive agents is usually performed with concomitant invasive blood pressure monitoring by an arterial catheter. Patients can be transferred from the CICU after they are transitioned to oral therapy for blood pressure control and with improvement or stabilization of end-organ damage.
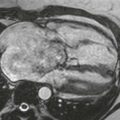
Cardiac Tamponade
A stable pericardial effusion without clinical signs of cardiac tamponade may not require admission to the CICU. In a patient with a known pericardial effusion, the clinical examination may help guide decisions about the appropriateness of expectant management or more urgent, invasive intervention.110 Cardiac tamponade with only mild hemodynamic compromise may be treated conservatively; this may require admission to the CICU for careful monitoring, serial echocardiographic studies, and therapy aimed at the underlying cause. Volume expansion is valuable in hypovolemic patients.111 Tamponade with overt hemodynamic compromise requires urgent removal of pericardial fluid, which produces a rapid improvement in cardiac hemodynamics.112 Removal of pericardial fluid can be performed by catheter pericardiocentesis or surgical pericardiectomy. Positive-pressure mechanical ventilation should be avoided if possible in patients with acute tamponade because it reduces cardiac filling further.113
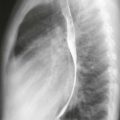
Pulmonary Embolism
Thrombolysis can be lifesaving in patients with cardiogenic shock from massive pulmonary embolus.114 If performed in the emergency department, the patient should be admitted to the ICU for monitoring. Thrombolysis can minimize escalation of therapy—defined as the need for pressors, mechanical ventilation, cardiopulmonary resuscitation, or open-label thrombolysis—without an increase in major bleeding in patients with normal systemic blood pressure, but with right ventricular dysfunction or pulmonary hypertension.115
Periprocedure and Postprocedure Setting
The risk of producing a major complication (death, MI, or major embolization) during diagnostic cardiac catheterization is generally less than 1%.116 Rates of major complications after PCI are also low.117 If a coronary artery complication, myocardial ischemia, or vascular complication is suspected or detected, however, admission to the CICU after the procedure may be warranted. In particular, vascular access complications, including retroperitoneal bleeding, pseudoaneurysm formation, and arteriovenous fistula formation, may require postprocedure admission to the CICU. Patients with major bleeding after PCI have higher in-hospital and 1-year mortality compared with patients with minor or no bleeding.118 The need for transfusion of red blood cells for a bleeding complication after PCI is independently associated with in-hospital mortality.119
Complications of invasive cardiac electrophysiology studies are low. In one series, the complication rate was reported at approximately 2%, and there was no mortality.120 If a serious complication such as tricuspid valve damage, pulmonary embolism, cardiac chamber perforation, cardiac tamponade, or other vascular injury occurs, however, management in the CICU is appropriate in conjunction with cardiothoracic surgeons if needed.
Marenzi and coworkers121 have shown that periprocedural hemofiltration effectively prevents the deterioration of renal function resulting from contrast agent–induced nephropathy, and is associated with improved in-hospital and long-term outcomes. More frequent use of this treatment paradigm in patients with chronic kidney disease undergoing an invasive cardiac procedure requiring a contrast agent would result in a larger number of periprocedural admissions to the CICU.
Specific Populations
Elderly
The elderly population, defined as individuals 65 years old or older, numbered 37.3 million in 2006, which represents 12.4% of the U.S. population, about one in every eight Americans.122 Patients 75 years old or older with acute MI were 2.5 times more likely not to be admitted to the CICU than younger patients with acute MI.123 There is evidence that after cardiac surgery and intensive care admission, surviving elderly patients have experienced a favorable outcome in terms of quality of life, and mortality rates are acceptably low.124 Efforts need to be directed toward narrowing this discrepancy in CICU admission rates. In a study of nonagenarians and centenarians with NSTEMI, increasing adherence to guideline-recommended therapies was associated with decreased mortality.125 These findings reinforce the importance of optimizing care patterns for even the oldest patients with NSTEMI, while examining novel approaches to reduce the risk of bleeding in this rapidly expanding patient population.125
Women
Attempts at making cardiovascular randomized controlled trials more inclusive of women seem to have had limited success. Women remain underrepresented in published trial literature relative to their disease prevalence126; this has important implications because safety and efficacy can vary as a function of gender. In one cohort of patients with known coronary artery disease, less aggressive treatment of coronary artery disease and less use of aspirin among women than among men was found during 1 year of observation.127 After controlling for baseline differences, women with coronary artery disease in this study experienced a more rapid decline in physical health status than did men. There is evidence that gender differences in the treatment of cardiac disease seem to be evident. There are no data reviewing gender differences in the CICU specifically, but some differences in the use of cardiac procedures have been observed. These gender differences may involve other factors, however. Mark and colleagues128 reported that academic cardiologists made appropriately lower pretest predictions of categories of disease in women with possible coronary artery disease than in men, and these assessments, along with women’s lower rate of positive exercise tests, rather than bias based on sex, accounted for the lower rate of catheterization among women. Gender differences may also be augmented by varying practice patterns. Women with ACS experience more bleeding than men whether or not they are treated with glycoprotein IIb/IIIa inhibitors. Because of frequent excessive dosing in women, however, one fourth of this sex-related risk difference in bleeding is avoidable.129 Gender differences in cardiac care is an issue that needs further exploration.
Minority Populations
After adjustment for sociodemographics, comorbidity, and illness severity, African Americans admitted to hospitals without revascularization services remain less likely to be transferred, and African Americans admitted to hospitals with revascularization are less likely to undergo revascularization compared with whites.130 In a study by Johnson and associates,131 after adjustments were made for multiple clinical factors, a lower proportion of African Americans presenting with acute chest pain were admitted to the hospital, and, after being admitted, African Americans were less likely to be triaged to the CICU. It is imperative that all CICUs distribute resources to the patients in greatest medical need regardless of other factors.
1. Heart Disease and Stroke Statistics—2007 Update. A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69-e171.
2. Hlatky M.A., Mark D.B. Economics and cardiovascular disease. In: Zipes D.P., Libby P., Bonow R.O., Braunwald E., editors. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 7th ed. Philadelphia: Saunders; 2005:20-26.
3. Selker H.P., Griffith J.L., Dorey F.J., D’Agostino R.B. How do physicians adapt when the coronary care unit is full? A prospective multicenter study. JAMA. 1987;257:1181-1185.
4. Fuchs R., Scheidt S. Improved criteria for admission to cardiac care units. JAMA. 1981;246:2037-2041.
5. Pozen M.W., D’Agostino R.B., Selker H.P., et al. A predictive instrument to improve coronary-care-unit admission practices in acute ischemic heart disease: A prospective multicenter clinical trial. N Engl J Med. 1984;310:1273-1278.
6. Julian D.G. The history of coronary care units. Br Heart J. 1987;57:497-502.
7. Khush K.K., Rapaport E., Waters D. The history of the coronary care unit. Can J Cardiol. 2005;21:1041-1045.
8. Killip T.3rd, Kimball J.T. Treatment of myocardial infarction in a coronary care unit: A two year experience with 250 patients. Am J Cardiol. 1967;20:457-464.
9. Mehta N.J., Khan I.A. Cardiology’s 10 greatest discoveries of the 20th century. Tex Heart Inst J. 2002;29:164-171.
10. McCaig L., Burt C. National Hospital Ambulatory Medical Care Survey: 2003 Emergency Department Summary. In: Advance Data from Vital and Health Statistics. Atlanta, GA: Centers for Disease Control and Prevention; 2005.
11. Launbjerg J., Fruergaard P., Hesse B., et al. Long-term risk of death, cardiac events and recurrent chest pain in patients with acute chest pain of different origin. Cardiology. 1996;87:60-66. 1996
12. Lindsell C.J., Anantharaman V., Diercks D., et al. The Internet Tracking Registry of Acute Coronary Syndromes: A multicenter registry of patients with suspicion of acute coronary syndromes reported using the standardized reporting guidelines for emergency department chest pain studies. Ann Emerg Med. 2006;48:666-677.
13. Goldman L. Using prediction models and cost-effectiveness analysis to improve clinical decisions: Emergency department patients with acute chest pain. Proc Assoc Am Physicians. 1995;107:329-333.
14. Lee T.H., Goldman L. The coronary care unit turns 25: Historical trends and future directions. Ann Intern Med. 1988;108:887-894.
15. Farkouh M.E., Smars P.A., Reeder G.S., et al. A clinical trial of a chest-pain observation unit for patients with unstable angina. Chest Pain Evaluation in the Emergency Room (CHEER) Investigators. N Engl J Med. 1998;339:1882-1888.
16. Amsterdam E.A., Kirk J.D., Diercks D.B., et al. Immediate exercise testing to evaluate low-risk patients presenting to the emergency department with chest pain. J Am Coll Cardiol. 2002;40:251-256.
17. Goldman L., Cook E.F., Brand D.A., et al. A computer protocol to predict myocardial infarction in emergency department patients with chest pain. N Engl J Med. 1988;318:797-803.
18. Selker H.P., Beshansky J.R., Griffith J.L., et al. Use of the acute cardiac ischemia time-insensitive predictive instrument (ACI-TIPI) to assist with triage of patients with chest pain or other symptoms suggestive of acute cardiac ischemia: A multicenter, controlled clinical trial. Ann Intern Med. 1998;129:845-855.
19. Fineberg H.V., Scadden D., Goldman L. Care of patients with a low probability of acute myocardial infarction: Cost effectiveness of alternatives to coronary-care-unit admission. N Engl J Med. 1984;310:1301-1307.
20. Goldman L., Cook E.F., Johnson P.A., et al. Prediction of the need for intensive care in patients who come to the emergency departments with acute chest pain. N Engl J Med. 1996;334:1498-1504.
21. Corey G.A., Merenstein J.H. Applying the acute ischemic heart disease predictive instrument. J Fam Pract. 1987;25:127-133.
22. Lee T.H., Pearson S.D., Johnson P.A., et al. Failure of information as an intervention to modify clinical management: A time-series trial in patients with acute chest pain. Ann Intern Med. 1995;122:434-437.
23. Pearson S.D., Goldman L., Garci T.B., et al. Physician response to a prediction rule for the triage of emergency department patients with chest pain. J Gen Intern Med. 1994;9:241-247.
24. Tosteson A.N.A., Goldman L., Udvarhelyi S., Lee T.H. Cost-effectiveness of a coronary care unit versus an intermediate care unit for emergency department patients with chest pain. Circulation. 1996;94:143-150.
25. Lee T.H., Goldman L. Evaluation of the patient with acute chest pain. N Engl J Med. 2000;342:1187-1195.
26. Lee T.H., Juarez G., Cook E.F., et al. Ruling out acute myocardial infarction: A prospective multicenter validation of a 12-hour strategy for patients at low risk. N Engl J Med. 1991;324:1239-1246.
27. Weingarten S.R., Riedinger M.S., Conner L., et al. Practice guidelines and reminders to reduce duration of hospital stay for patients with chest pain: An interventional trial. Ann Intern Med. 1994;120:257-263.
28. Antman E., Bassand J.-P., Klein W., et al. Myocardial infarction redefined—a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36:959-969.
29. Nomenclature and criteria for diagnosis of ischemic heart disease. Report of the Joint International Society and Federation of Cardiology/World Health Organization task force on standardization of clinical nomenclature. Circulation. 1979;59:607-609.
30. Amit G., Gilutz H., Cafri C., et al. What have the new definition of acute myocardial infarction and the introduction of troponin measurement done to the coronary care unit? Impacts on admission rate, length of stay, case mix and mortality. Cardiology. 2004;102:171-176.
31. Zahger D., Hod H., Gottlieb S., et al. for the ACSIS 2002 Study Group: Influence of the new definition of acute myocardial infarction on coronary care unit admission, discharge diagnosis, management and outcome in patients with non-ST elevation acute coronary syndromes: A national survey. Int J Cardiol. 2006;106:164-169.
32. Alexander K.P., Chen A.Y., Roe M.T., et al. CRUSADE Investigators: Excess dosing of antiplatelet and antithrombin agents in the treatment of non-ST-segment elevation acute coronary syndromes. JAMA. 2005;294:3108-3116.
33. Antman E.M., Cohen M., Bernink P.J., et al. The TIMI risk score for unstable angina/non-ST elevation MI: A method for prognostication and therapeutic decision making. JAMA. 2000;284:835-842.
34. Fiebach N.H., Cook E.F., Lee T.H., et al. Outcomes in patients with myocardial infarction who are initially admitted to stepdown units: Data from the Multicenter Chest Pain Study. Am J Med. 1990;89:15-20.
35. Cannon C.P., Hand M.H., Bahr R., et al. National Heart Attack Alert Program (NHAAP) Coordinating Committee Critical Pathways Writing Group: Critical pathways for management of patients with acute coronary syndromes: An assessment by the National Heart Attack Alert Program. Am Heart J. 2002;143:777-789.
36. National Hospital Discharge Survey, CDC/NCHS. Available at: http://www.cdc.gov/DHDSP/library/fs_heart_failure.htm Accessed: August 15, 2007.
37. Chin M.H., Goldman L. Factors contributing to the hospitalization of patients with congestive heart failure. Am J Public Health. 1997;87:643-648.
38. Cleland J.G., Daubert J.C., Erdmann E., et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352:1539-1549.
39. Bardy G.H., Lee K.L., Mark D.B., et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225-237.
40. Adams K.F.Jr., Fonarow G.C., Emerman C.L., et al. ADHERE Scientific Advisory Committee and Investigators: Characteristics and outcomes of patients hospitalized for heart failure in the United States: Rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005;149:209-216.
41. Weingarten S.R., Riedinger M.S., Shinbane J., et al. Triage practice guideline for patients hospitalized with congestive heart failure: Improving the effectiveness of the coronary care unit. Am J Med. 1993;94:483-490.
42. Binanay C., Califf R.M., Hasselblad V., et al. ESCAPE Investigators and ESCAPE Study Coordinators: Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness: The ESCAPE trial. JAMA. 2005;294:1625-1633.
43. Palmer R.F., Lasseter K.C. Drug therapy: Sodium nitroprusside. N Engl J Med. 1975;292:294-297.
44. Schulz V. Clinical pharmacokinetics of nitroprusside, cyanide, thiosulphate and thiocyanate. Clin Pharmacokinet. 1984;9:239-251.
45. Leier C.V. Current status of non-digitalis positive inotropic drugs. Am J Cardiol. 1992;69:120G-128G.
46. Patel M.B., Kaplan I.V., Patni R.N., et al. Sustained improvement in flow-mediated vasodilation after short-term administration of dobutamine in patients with severe congestive heart failure. Circulation. 1999;99:60-64.
47. Cesario D., Clark J., Maisel A. Beneficial effects of intermittent home administration of the inotrope/vasodilator milrinone in patients with end-stage congestive heart failure: A preliminary study. Am Heart J. 1998;135:121-129.
48. Thackray S., Easthaugh J., Freemantle N., Cleland J.G. The effectiveness and relative effectiveness of intravenous inotropic drugs acting through the adrenergic pathway in patients with heart failure—a meta-regression analysis. Eur J Heart Fail. 2002;4:515-529.
49. Colucci W.S., Elkayam U., Horton D.P., et al. Intravenous nesiritide, a natriuretic peptide, in the treatment of decompensated congestive heart failure. Nesiritide Study Group. N Engl J Med. 2000;343:246-253.
50. Sackner-Bernstein J.D., Skopicki H.A., Aaronson K.D. Risk of worsening renal function with nesiritide in patients with acutely decompensated heart failure. Circulation. 2005;111:1487-1491.
51. Sackner-Bernstein J.D., Kowalski M., Fox M., Aaronson K. Short-term risk of death after treatment with nesiritide for decompensated heart failure: A pooled analysis of randomized controlled trials. JAMA. 2005;293:1900-1905.
52. Menghini V.V., Savcenko V., Olson L.J., et al. Combined immunosuppression for the treatment of idiopathic giant cell myocarditis. Mayo Clin Proc. 1999;74:1221-1226.
53. Magnani J.W., Dec G.W. Myocarditis: Current trends in diagnosis and treatment. Circulation. 2006;113:876-890.
54. Stevenson L.W., Miller L.W., Desvigne-Nickens P., et al. REMATCH Investigators: Left ventricular assist device as destination for patients undergoing intravenous inotropic therapy: A subset analysis from REMATCH (Randomized Evaluation of Mechanical Assistance in Treatment of Chronic Heart Failure). Circulation. 2004;110:975-981.
55. Maybaum S., Mancini D., Xydas S., et al. LVAD Working Group: Cardiac improvement during mechanical circulatory support: A prospective multicenter study of the LVAD Working Group. Circulation. 2007;115:2497-2505.
56. Hauff H. UNOS policy and transplant coordination in practice. In: Edwards N.M., Chen J.M., Mazzeo P.A., editors. Cardiac Transplantation. Totowa, NJ, Human Press: The Columbia University Medical Center/New York Presbyterian Hospital Manual; 2004:37-62.
57. Mather P.J., Konstam M.A. Percutaneous mechanical devices in the management of decompensated heart failure. Curr Heart Fail Rep. 2007;4:43-47.
58. McAlister F.A., Ezekowitz J., Tonelli M., Armstrong P.W. Renal insufficiency and heart failure: Prognostic and therapeutic implications from a prospective cohort study. Circulation. 2004;109:1004-1009.
59. Costanzo M.R., Guglin M.E., Saltzberg M.T., et al. UNLOAD Trial Investigators: Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol. 2007;49:675-683.
60. Klein L., O’Connor C.M., Leimberger J.D., et al. OPTIME-CHF Investigators: Lower serum sodium is associated with increased short-term mortality in hospitalized patients with worsening heart failure: Results from the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF) study. Circulation. 2005;111:2454-2460.
61. Filippatos G., Rossi J., Lloyd-Jones D.M., et al. Prognostic value of blood urea nitrogen in patients hospitalized with worsening heart failure: Insights from the Acute and Chronic Therapeutic Impact of a Vasopressin Antagonist in Chronic Heart Failure (ACTIV in CHF) study. J Card Fail. 2007;13:360-364.
62. Schrier R.W., Gross P., Gheorghiade M., et al. SALT Investigators: Tolvaptan, a selective oral vasopressin V2-receptor antagonist, for hyponatremia. N Engl J Med. 2006;355:2099-2112.
63. Konstam M.A., Gheorghiade M., Burnett J.C., et al. Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) Investigators: Effects of oral tolvaptan in patients hospitalized for worsening heart failure: The EVEREST Outcome Trial. JAMA. 2007;297:1319-1331.
64. Humbert M., Sitbon O., Simmonneau G. Treatment of pulmonary arterial hypertension. N Engl J Med. 2004;351:1425-1436.
65. Barst R.J., Rubin D.J., Long W.A., et al. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. The Primary Pulmonary Hypertension Study Group. N Engl J Med. 1996;334:296-302.
66. Ichinose F., Roberts J.D.Jr., Zapol W.M. Inhaled nitric oxide: A selective pulmonary vasodilator: current uses and therapeutic potential. Circulation. 2004;109:3106-3111.
67. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112(Suppl 1):1-203.
68. Antunes E., Brugada J., Steurer G., et al. The differential diagnosis of a regular tachycardia with a wide QRS complex on the 12-lead ECG: Ventricular tachycardia, supraventricular tachycardia with aberrant intraventricular conduction, and supraventricular tachycardia with anterograde conduction over an accessory pathway. Pacing Clin Electrophysiol. 1994;17:1515-1524.
69. Exner D.V., Pinski S.L., Wyse D.G., et al. Electrical storm presages nonsudden death: The antiarrhythmics versus implantable defibrillators (AVID) trial. Circulation. 2001;103:2066-2071.
70. Zipes D.P., Camm A.J., Borggrefe M., et al. ACC/AHA/ESC 2006 Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death—Executive Summary. A report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). J Am Coll Cardiol. 2006;48:1064-1108.
71. Myerburg R.J., Castellanos A. Cardiac arrest and sudden cardiac death. In: Zipes D.P., Libby P., Bonow R.O., Braunwald E., editors. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 7th ed. Philadelphia: Saunders; 2005:865-908.
72. Rea T.D., Eisenberg M.S., Becker L.J., et al. Temporal trends in sudden cardiac arrest: A 25-year emergency medical services perspective. Circulation. 2003;107:2780-2785.
73. Nolan J.P., Morley P.T., Vanden Hoek T.L., et al. International Liaison Committee on Resuscitation: Therapeutic hypothermia after cardiac arrest: An advisory statement by the Advanced Life Support Task Force of the International Liaison Committee on Resuscitation. Circulation. 2003;108:118-121.
74. Ryan T.J., Anderson J.L., Antman E.M., et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). J Am Coll Cardiol. 1996;28:1328-1428.
75. Mueller P.S., Hook C.C., Hayes D.L. Ethical analysis of withdrawal of pacemaker or implantable cardioverter-defibrillator support at the end of life. Mayo Clin Proc. 2003;78:959-963.
76. Lewis W.R., Luebke D.L., Johnson N.J., et al. Withdrawing implantable defibrillator shock therapy in terminally ill patients. Am J Med. 2006;119:892-896.
77. Tschopp D., Mukherjee D. Complications of myocardial infarction. In: Griffin B.P., Topol E.J., editors. Manual of Cardiovascular Medicine. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2004:45-63.
78. Hochman J.S., Sleeper L.A., Webb J.G., et al. Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock (SHOCK) Investigators: Early revascularization in acute myocardial infarction complicated by cardiogenic shock. N Engl J Med. 1999;341:625-634.
79. Hochman J.S., Sleeper L.A., Webb J.G., et al. SHOCK Investigators: Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction. JAMA. 2006;295:2511-2515.
80. Chen Z.M., Pan H.C., Chen Y.P., et al. COMMIT (Clopidogrel and Metoprolol in Myocardial Infarction Trial) collaborative group: Early intravenous then oral metoprolol in 45,852 patients with acute myocardial infarction: Randomised placebo-controlled trial. Lancet. 2005;366:1622-1632.
81. Dang N.C., Topkara V.K., Leacche M., et al. Left ventricular assist device implantation after acute anterior wall myocardial infarction and cardiogenic shock: A two-center study. J Thorac Cardiovasc Surg. 2005;130:693-698.
82. Ishihara M., Sato H., Tateishi H., et al. Intraaortic balloon pumping as the postangioplasty strategy in acute myocardial infarction. Am Heart J. 1991;122:385-389.
83. Lincoff A.M., Popma J.J., Ellis S.G., et al. Percutaneous support devices for high risk or complicated coronary angioplasty. J Am Coll Cardiol. 1991;17:770-780.
84. Gold H.K., Leinbach R.C., Sanders C.A., et al. Intraaortic balloon pumping for ventricular septal defect or mitral regurgitation complicating acute myocardial infarction. Circulation. 1973;47:1191-1196.
85. Rajai H.R., Hartman C.W., Innes B.J., et al. Prophylactic use of intraaortic balloon pump in aortocoronary bypass for patients with left main coronary artery disease. Ann Surg. 1978;187:118-121.
86. Field M., Rengarajan A., Khan O., et al. Preoperative intra aortic balloon pumps in patients undergoing coronary artery bypass grafting. Cochrane Database Syst Rev. 2007;1:CD004472.
87. Webb G.D., Smallhorn J.F., Therrien J., Redington A.N. Congenital heart disease. In: Zipes D.P., Libby P., Bonow R.O., Braunwald E., editors. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 7th ed. Philadelphia: Saunders; 2005:1489-1552.
88. Therrien J., Dore A., Gersony W., et al. Canadian Cardiovascular Society (CCS): CCS Consensus Conference 2001 update: Recommendations for the management of adults with congenital heart disease. Part I. Can J Cardiol. 2001;17:940-959.
89. Chatterjee K., Parmley W.W., Swan H.J., et al. Beneficial effects of vasodilator agents in severe mitral regurgitation due to dysfunction of subvalvar apparatus. Circulation. 1973;48:684-690.
90. Bonow R.O., Carabello B.A., Kanu C., et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): Developed in collaboration with the Society of Cardiovascular Anesthesiologists: Endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation. 2006;114:e84-e231.
91. Roberts W.C., Ko J.M., Moore T.R., Jones W.H.3rd. Causes of pure aortic regurgitation in patients having isolated aortic valve replacement at a single US tertiary hospital. Circulation. 2006;114:422-429.
92. Bauernschmitt R., Jakob H.G., Vahl C.F., et al. Operation for infective endocarditis: Results after implantation of mechanical valves. Ann Thorac Surg. 1998;65:359-364.
93. Middlemost S., Wisenbaugh T., Meyerowitz C., et al. A case for early surgery in native left-sided endocarditis complicated by heart failure: Results in 203 patients. J Am Coll Cardiol. 1991;18:663-667.
94. Moreno P.R., Jang I.K., Newell J.B., et al. The role of percutaneous aortic balloon valvuloplasty in patients with cardiogenic shock and critical aortic stenosis. J Am Coll Cardiol. 1994;23:1071-1075.
95. Cribier A., Eltchaninoff H., Tron C., et al. Treatment of calcific aortic stenosis with the percutaneous heart valve: Mid-term follow-up from the initial feasibility studies: The French experience. J Am Coll Cardiol. 2006;47:1214-1223.
96. Grube E., Laborde J.C., Gerckens U., et al. Percutaneous implantation of the CoreValve self-expanding valve prosthesis in high-risk patients with aortic valve disease: The Siegburg first-in-man study. Circulation. 2006;114:1616-1624.
97. Lichtenstein S.V., Cheung A., Ye J., et al. Transapical transcatheter aortic valve implantation in humans: Initial clinical experience. Circulation. 2006;114:591-596.
98. Erbel R., Alfonso F., Boileau C., et al. Diagnosis and management of aortic dissection. Eur Heart J. 2001;22:1642-1681.
99. Tsai T.T., Nienaber C.A., Eagle K.A. Acute aortic syndromes. Circulation. 2005;112:3802-3813.
100. Tsai T.T., Evangelista A., Nienaber C.A., et al. International Registry of Acute Aortic Dissection: Partial thrombosis of the false lumen in patients with acute type B aortic dissection. N Engl J Med. 2007;357:349-359.
101. von Kodolitsch Y., Csosz S.K., Koschyk D.H., et al. Intramural hematoma of the aorta: Predictors of progression to dissection and rupture. Circulation. 2003;107:1158-1163.
102. Erbel R., Alfonso F., Boileau C., et al. Diagnosis and management of aortic dissection. Eur Heart J. 2001;22:1642-1681.
103. Hajjar I., Kotchen T.A. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003;290:199-206.
104. Osterberg L., Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487-497.
105. Bender S.R., Fong M.W., Heitz S., Bisognano J.D. Characteristics and management of patients presenting to the emergency department with hypertensive urgency. J Clin Hypertens. 2006;8:12-18.
106. Kaplan N.M. Systemic hypertension: Therapy. In: Zipes D.P., Libby P., Bonow R.O., Braunwald E., editors. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 7th ed. Philadelphia: Saunders; 2005:989-1012.
107. Gifford R.W. Management of hypertensive crises. JAMA. 1991;266:829-835.
108. Ram C.V. Management of hypertensive emergencies: Changing therapeutic options. Am J Heart. 1991;122(1 Pt 2):356-363.
109. Tuncel M., Ram V.C. Hypertensive emergencies: Etiology and management. Am J Cardiovasc Drugs. 2003;3:21-31.
110. Roy C.L., Minor M.A., Brookhart M.A., Choudhry N.K. Does this patient with a pericardial effusion have cardiac tamponade? JAMA. 2007;297:1810-1818.
111. Spodick D.H. Acute cardiac tamponade. N Engl J Med. 2003;349:684-690.
112. Reddy P.S., Curtiss E.I., O’Toole J.D., Shaver J.A. Cardiac tamponade: Hemodynamic observations in man. Circulation. 1978;58:265-272.
113. Little W.C., Freeman G.L. Pericardial disease. Circulation. 2006;113:1622-1632.
114. Arcasoy S.M., Kreit J.W. Thrombolytic therapy of pulmonary embolism: A comprehensive review of current evidence. Chest. 1999;115:1695-1707.
115. Konstantinides S., Geibel A., Heusel G., et al. Management Strategies and Prognosis of Pulmonary Embolism-3 Trial Investigators: Heparin plus alteplase compared with heparin alone in patients with submassive pulmonary embolism. N Engl J Med. 2002;347:1143-1150.
116. Baim D.S., Grossman W. Complications of cardiac catheterization. In Baim D.S., editor: Grossman’s Cardiac Catheterization, Angiography and Intervention, 7th ed, Baltimore: Lippincott Williams & Wilkins, 2005.
117. Weintraub W.S., Mahoney E.M., Ghazzal Z.M., et al. Trends in outcome and costs of coronary intervention in the 1990s. Am J Cardiol. 2001;88:497-503.
118. Kinnaird T.D., Stabile E., Mintz G.S., et al. Incidence, predictors, and prognostic implications of bleeding and blood transfusion following percutaneous coronary interventions. Am J Cardiol. 2003;92:930-935.
119. Yatskar L., Selzer F., Feit F., et al. Access site hematoma requiring blood transfusion predicts mortality in patients undergoing percutaneous coronary intervention: Data from the National Heart, Lung, and Blood Institute Dynamic Registry. Catheter Cardiovasc Interv. 2007;69:961-966.
120. Dimarco J.P., Garan H., Ruskin J.N. Complications in patients undergoing cardiac electrophysiologic procedures. Ann Intern Med. 1982;97:490-493.
121. Marenzi G., Marana I., Lauri G., et al. The prevention of radiocontrast-agent-induced nephropathy by hemofiltration. N Engl J Med. 2003;349:1333-1340.
122. Department of Health and Human Services, Administration on Aging. Available at: http://www.aoa.gov/prof/Statistics/statistics.asp, Aging Statistics. Accessed: August 1, 2007.
123. Fleming C., D’Agostino R.B., Selker H.P. Is coronary-care-unit admission restricted for elderly patients? A multicenter study. Am J Public Health. 1991;81:1121-1126.
124. McHugh G.J., Havill J.H., Armistead S.H., et al. Follow up of elderly patients after cardiac surgery and intensive care unit admission, 1991 to 1995. N Z Med J. 1997;110:432-435.
125. Skolnick A.H., Alexander K.P., Chen A.Y., et al. Characteristics, management, and outcomes of 5,557 patients age greater or equal to 90 years with acute coronary syndromes: Results from the CRUSADE Initiative. J Am Coll Cardiol. 2007;49:1790-1797.
126. Lee P.Y., Alexander K.P., Hammill B.G., et al. Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA. 2001;286:708-713.
127. Schwartz L.M., Fisher E.S., Tosteson N.A., et al. Treatment and health outcomes of women and men in a cohort with coronary artery disease. Arch Intern Med. 1997;157:1545-1551.
128. Mark D.B., Shaw L.K., DeLong E.R., et al. Absence of sex bias in the referral of patients for cardiac catheterization. N Engl J Med. 1994;330:1101-1106.
129. Alexander K.P., Chen A.Y., Newby L.K., et al. CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) Investigators: Sex differences in major bleeding with glycoprotein IIb/IIIa inhibitors: Results from the CRUSADE initiative. Circulation. 2006;114:1380-1387.
130 Popescu I., Vaughan-Sarrazin M.S., Rosenthal G.E. Differences in mortality and use of revascularization in black and white patients with acute MI admitted to hospitals with and without revascularization services. JAMA. 2007;297:2489-2495.
131. Johnson P.A., Lee T.H., Cook E.F., et al. Effect of race on the presentation and management of patients with acute chest pain. Ann Intern Med. 1993;118:593-601.