Chapter 9
Cardiac CT Angiography
1. What are the contraindications for cardiac computed tomography (CT)?
2. What is the difference between prospective triggering and retrospective gating?
Prospective triggering is an axial (step-and-shoot) image technique that acquires images of the heart in a predetermined phase of the cardiac cycle, for example 60% to 80% of the R-R interval. During the remainder of the cardiac cycle, the CT tube current is turned off. This is in contrast to retrospective gating, which is a spiral acquisition where the CT tube current remains on during the entire R-R interval. To reduce radiation, the tube current may be decreased during systole (electrocardiography [ECG] tube current modulation). However, there is a significant reduction in radiation dose when using prospective triggering (Fig. 9-1).
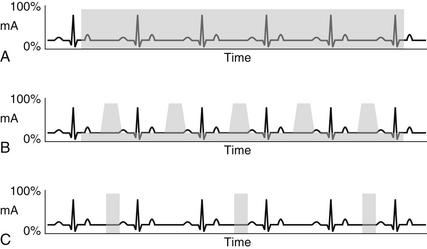
Figure 9-1 Schematic drawings of retrospective gating (A, B) and prospective triggering (C) techniques. Retrospective gating without tube current modulation (A) uses full tube current throughout the duration of the cardiac cycle. With tube current modulation applied (B), the full current is only delivered during a specified portion of the R-R interval (usually late diastole). In this case, the remainder of the cardiac cycle receives only 20% of the full tube current. Prospective triggering (C) only uses full tube current through a specified portion of the R-R interval. Every other heartbeat is imaged in prospective triggering to allow time for table movement.
3. When might retrospective gating be used rather than prospective triggering?
Retrospective gating is needed when cardiac function measurements are needed. Because images are acquired throughout the cardiac cycle, volume measurements of the right and left ventricles can be obtained in end-systole and end-diastole, allowing the calculation of stroke volume, ejection fraction, and cardiac output. Retrospective gating is also helpful in patients with irregular heart rhythm to help ensure diagnostic images of the coronary arteries are acquired. In contrast to prospective triggering, retrospective gating allows the user to employ ECG editing to remove artifacts related to premature ventricular contractions or dropped beats.
4. What is the radiation dose of a standard cardiac CT examination?
The radiation dose of a standard cardiac CTA depends on a multitude of factors and can range from less than 1 mSv to as high as 30 mSv with older high dose techniques and scanners. The median dose in an older registry study showed the cardiac CT dose to be just less than 10 mSv; however, since that time, there has been development of several new scanners and associated hardware, as well as new dose reduction strategies. At several hospitals (such as Massachusetts General Hospital), the median reported dose ranges from 3 to 5 mSv. To put things in perspective, the average dose from a nuclear perfusion stress test is 6 to 25 mSv (or as high as 40 mSv or more in thallium stress/rest tests), and the average dose from a simple diagnostic coronary angiogram is 5 to 7 mSv. Factors affecting the radiation dose of a cardiac CT include the type of scanner (single-source versus dual-source), the number of detectors (z-axis coverage), the body habitus of the patient, the selection of kilovolt peak (kVp) and milliampere seconds (mAs), and the scan mode (prospective triggering versus retrospective gating with or with or without tube current modulation, high pitch [FLASH] acquisitions). General measures to reduce the radiation dose to the patient should be used whenever possible, according to the “as low as reasonably achievable” (ALARA) principle. Tube modulation routinely should be applied if retrospective gating is selected, unless a specific reason prohibits its use (Fig. 9-2).
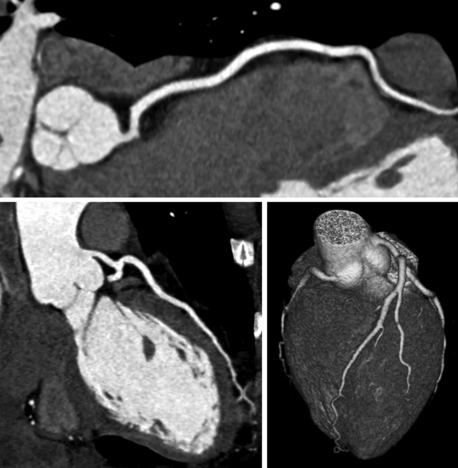
Figure 9-2 Curved multiplanar reconstructions of the right coronary artery (top) and left anterior descending coronary artery (bottom left) and volume-rendered three-dimensional reconstruction (bottom right) show absence of coronary plaque or stenosis. A negative computed tomography scan with good image quality has a very high negative predictive value and may spare the patient a diagnostic invasive angiogram. This study was done with a total radiation dose of 2.4 mSv.
5. What is blooming and what techniques can be done to reduce it?
Blooming is an artifact created when material with very high attenuation is being imaged. The borders of a high-attenuation material will “bleed” into adjacent structures. In the case of coronary CTA, blooming from calcified plaque can lead to overestimation of the degree of coronary stenosis. For this reason, a very high calcium score (generally greater than 1000) may yield nonevaluable coronary artery segments. Using a higher current (mA) and/or tube potential (kVp) can reduce blooming artifact. Using a sharp reconstruction kernel and thin slices can help in postprocessing and interpretation (Fig. 9-3).
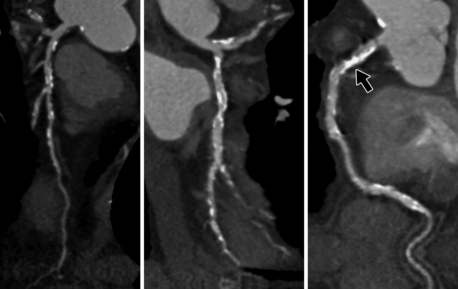
Figure 9-3 Curved multiplanar reconstructions of the left anterior descending coronary artery (left), left circumflex coronary artery (middle), and right coronary artery (right) demonstrate substantial calcification with blooming artifact. Evaluation of the degree of stenosis is limited in areas of extensive calcification, for example in the proximal right coronary artery (arrow). This patient had a calcium score of 867.
6. Are β-blockers necessary for coronary CTA?
7. A 66-year-old man with diabetes and smoking history comes to your clinic because he wants to check his calcium score. He states he read in a magazine that it is a good screening test for coronary artery disease (CAD). What is your response?
A calcium score is a specialized cardiac CT without contrast that is processed with software to quantify the amount of coronary calcium. This number, the Agatston score, is used as a surrogate for the total amount of coronary plaque and is correlated with patients of the same age and gender. It is most useful in patients with unclear or intermediate CAD risk, to guide decision-making. Whether this patient in question has a high or low calcium score, he is already considered high risk (ATP III/Framingham) and should be treated accordingly.
8. What is the value of a negative calcium score in a patient with low risk to intermediate risk?
A negative calcium score in a low-risk patient is associated with very low likelihood of coronary events. The “warranty period” for patients with 0 calcium score and low CAD risk is approximately 4 years. For patients with a 0 calcium score and low to intermediate risk, the negative predictive value for detecting obstructive CAD is between 95% and 99%. However, calcium scoring is not recommended in the acute chest pain setting, whereas coronary CTA may be a consideration (Fig. 9-4).
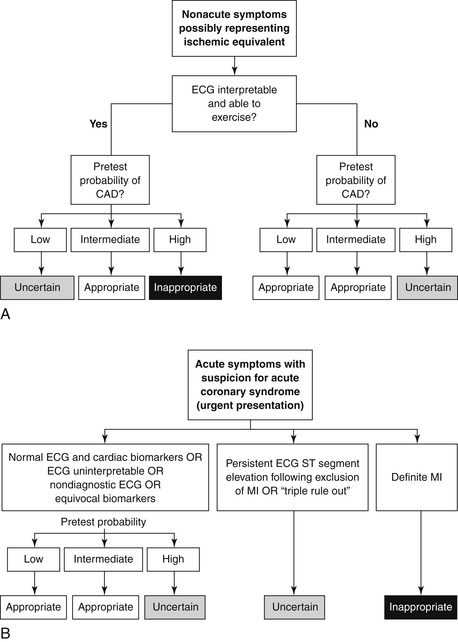
Figure 9-4 Flowcharts of suggested diagnostic imaging workup for patients with no known coronary artery disease (CAD) presenting with nonacute (A) and acute (B) symptoms suggestive of coronary ischemia. ECG, electrocardiogram; MI, myocardial infarction. (From Taylor AJ, Cerqueira M, Hodgson JM, et al: ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Appropriate use criteria for cardiac computed tomography, J Cardiovasc Comput Tomogr 4:407.e1-33, 2010.)
9. Is calcium scoring an appropriate test in a patient of low CAD risk but with a family history of premature CAD?
Patients with a family history of premature CAD have been shown to have detectable coronary artery calcium despite a low Framingham risk estimation. Thus, calcium scoring is an appropriate test to evaluate for subclinical coronary atherosclerosis in this population.
10. Summarize the current consensus of indications for coronary CTA in the management of CAD in patients with nonacute and acute symptoms without known heart disease.
Coronary CTA is appropriate in patients with nonacute symptoms potentially representing an ischemic equivalent and low or intermediate pretest probability of CAD. It is also appropriate in patients presenting acutely with suspected acute coronary syndrome (ACS) who have low or intermediate pretest probability of CAD and normal, nondiagnostic, or uninterpretable ECG or cardiac biomarkers (see Fig. 9-4).
11. A 49-year-old man with severe osteoarthritis presents with nonacute chest pain. You determine he has an intermediate pretest probability of CAD. Would cardiac CT be an appropriate first test to evaluate for CAD?
12. A 59-year-old woman with low to intermediate pretest probability of CAD presents with acute chest pain. Despite negative ECG and cardiac biomarkers, you are still suspicious for ACS. Is coronary CTA an appropriate test to evaluate for CAD?
Yes, patients with low to intermediate pretest probability of CAD and normal and/or equivocal ECG and biomarkers are appropriate for evaluation by coronary CTA. The Rule Out Myocardial Infarction Using Computer Assisted Tomography (ROMICAT) trials demonstrated that patients with no evidence of CAD by coronary CTA have essentially 0% chance of a major adverse cardiovascular event for at least two years, and subsequent trials have confirmed a close to zero event rate in this setting. Additionally, coronary CTA was shown to reduce the length of hospital stay compared with a standard in-hospital workup (Fig. 9-5).
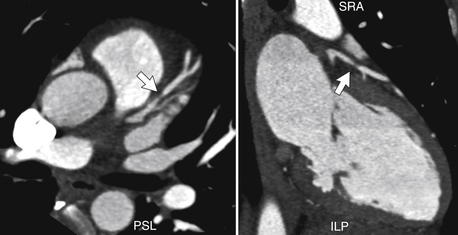
Figure 9-5 Multiplanar reformatted images demonstrate focal, severe stenosis of the mid left anterior descending (LAD) coronary artery (arrow). This patient was experiencing symptoms of acute chest pain. Conventional cardiac catheterization showed 85% stenosis in the mid LAD. Angioplasty and stenting were performed.
13. A 61-year-old woman presents to your office with nonacute chest pain. She has a history of prior stent placement in the right coronary artery (RCA). The stent is 2.5 mm in diameter. Is coronary CTA a useful test for detecting in-stent restenosis in this patient?
Accurate assessment of in-stent restenosis is based on a number of factors, including the diameter of the stent, material used, and size of the struts, as well as the capabilities of the CT scanner. Based on recent appropriateness criteria, stents less than 3 mm in diameter are not appropriate for evaluation by coronary CTA. A stent is considered occluded if the lumen is unopacified and there is absent distal runoff. The presence of distal contrast opacification alone is not an adequate sign of stent patency because of the potential for retrograde filling from collateral vessels. Figure 9-6 demonstrates a patent stent in a different patient with a larger stent.
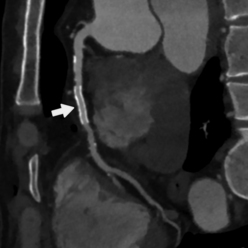
Figure 9-6 Curved multiplanar reconstruction of the right coronary artery (RCA) showing a patent stent in the mid RCA (arrow). Note contrast opacification within the stent and distal to the stent. A sharp reconstruction kernel and thin slices were used for reconstructions. This particular stent measured 3.5 mm in diameter.
14. A 69-year-old man with history of prior coronary artery bypass graft (CABG) presents with nonacute chest pain. Is coronary CTA useful for detecting graft stenosis in this patient?
Coronary CTA is indicated for symptomatic patients with prior CABG to evaluate for graft patency. It is also an excellent method for evaluating graft thrombosis, malposition, aneurysms, and pseudoaneurysms. Inclusion of the entire chest is helpful in the postoperative period for evaluating pericardial or pleural effusions, mediastinal or wound infection, and the integrity of the sternotomy (Fig. 9-7).
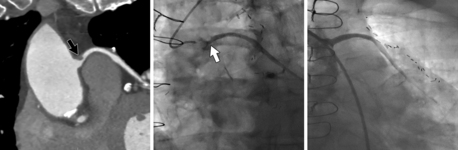
Figure 9-7 Curved multiplanar reconstruction (left image) of a saphenous vein graft demonstrates focal, proximal stenosis of the graft (black arrow). Conventional angiogram (middle image) confirms the high-grade stenosis (white arrow). After intervention with balloon angioplasty, the vessel is widely patent (right image).
15. What is the role of cardiac CT in patients presenting for noncoronary cardiac surgery?
16. What is the diagnostic accuracy and clinical utility of plaque characterization by cardiac CT?
17. Is cardiac CT safe and useful in patients presenting with newly diagnosed heart failure? What is the objective in this patient population?
18. Can cardiac CT be used to differentiate between a subacute and an old myocardial infarction (MI)?
Characteristic morphologic changes in the myocardium can be detected in patients who have a remote history of MI. Patients usually develop wall thinning in relation to normal, adjacent myocardium. In some instances, fatty metaplasia or calcification may develop. If retrospective gating is used, a regional wall motion abnormality is usually seen. Delayed enhancement imaging reveals an area of hyperenhancement in the appropriate coronary territory. In contrast, an acute myocardial infarct will appear as a hypoperfused, akinetic area of myocardium with normal wall thickness (Fig. 9-8).
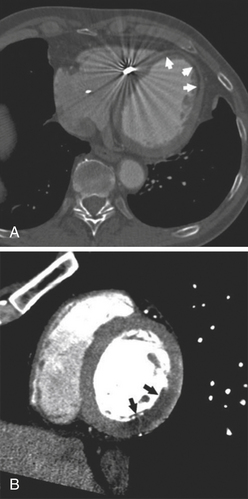
Figure 9-8 A, Cardiac-gated axial computed tomography (CT) shows apical myocardial thinning and deposition of subendocardial low-attenuation material (arrows) measuring −15 Hounsfield units (HU), indicating fatty metaplasia in a patient with remote left anterior descending myocardial infarction. B, Cardiac-gated CT in left ventricular short axis shows inferolateral subendocardial hypoenhancement that measures 35 HU (arrows) and normal myocardial wall thickness, representing a perfusion defect in a patient with acute left circumflex myocardial infarction.
19. Should noncoronary structures be reviewed and reported on during cardiac CT examination?
20. Summarize the appropriate uses of cardiac CT in regard to evaluation of cardiac structure and function.
Cardiac CT is an excellent test for evaluation of coronary anomalies and assessment of adult congenital heart disease. It is appropriate for evaluating left ventricular function after MI or in patients with congestive heart failure (CHF) when other imaging modalities are inadequate, and it is useful for evaluating the right ventricular morphology and function, including in cases of suspected arrhythmogenic right ventricular dysplasia (ARVD). When other imaging modalities are inadequate or incomplete, it is useful for evaluating native or prosthetic cardiac valves in the setting of valvular dysfunction and for evaluating cardiac masses. Prior to invasive procedures, cardiac CT is useful for pulmonary vein mapping, coronary vein mapping, and for localizing bypass grafts and other retrosternal anatomy. Finally, cardiac CT is an appropriate test for evaluation of the pericardium.
21. Would cardiac CT be an appropriate first modality in the assessment of a 29-year-old woman with suspected Turner’s syndrome presenting with symptoms of dyspnea, murmur, and hypertension?
Patients with suspected Turner’s syndrome may have multiple congenital anomalies, including a bicuspid aortic valve, coarctation of the aorta, elongation of the transverse aortic arch, atrial or ventricular septal defect, and partial anomalous pulmonary venous return. Cardiac CT is a reasonable choice as the first modality in assessing all of these congenital anomalies in a single study (Figs. 9-9 and 9-10).
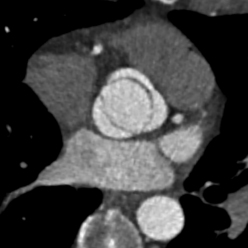
Figure 9-9 Systolic frame of retrospectively gated cardiac computed tomography in short-axis plane of the aortic valve shows an open, bicuspid aortic valve. There is congenital fusion of the right and left coronary cusps.
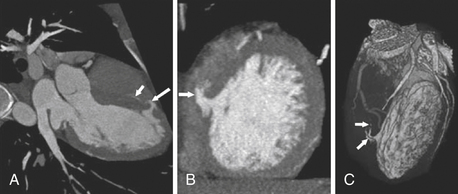
Figure 9-10 Cardiac gated computed tomographic angiogram in (A) left ventricle (LV) long-axis and (B) short-axis views shows a defect in the ventricular septum with contrast spilling from the opacified LV cavity across the septum into the otherwise unopacified right ventricle (arrows). C, The volume-rendered image shows the contrast within the LV cavity and the small shunt volume (arrows) crossing into the unopacified right ventricle.
22. A 22-year-old female is being evaluated for syncope. Echocardiography was not able to demonstrate a normal origin of the RCA. Is coronary CTA an appropriate next test?
23. A 45-year-old female is having a CT of the pulmonary veins prior to radiofrequency ablation for atrial fibrillation. What is the purpose of pulmonary vein mapping? What is the most common anatomic variant of the pulmonary veins?
Intraoperative pulmonary vein mapping with conventional angiography can be time consuming, and significant time-savings can be realized by mapping the pulmonary veins with CT. Digital Imaging and Communications in Medicine (DICOM) image datasets can be uploaded into cardiac imaging software for direct correlation and fusion with electroanatomic maps during the pulmonary vein isolation procedure. Preoperative mapping is also useful for detecting variant anatomy, which can be fairly common; the most common anatomic variant is a separate ostium for the right middle pulmonary vein. Measurement of the pulmonary vein ostia may be important for the proper catheter selection and for future comparison if there is a question of pulmonary vein stenosis (Fig. 9-11).
Bibliography, Suggested Readings, and Websites
1. Abbara, S., Walker, T.G. Diagnostic imaging: cardiovascular, ed 1, Salt Lake City: Amirsys, 2008.
2. Achenbach, S., Cardiac, C.T. State of the art for the detection of coronary arterial stenosis. J Cardiovasc Comput Tomogr. 2007;1:3–20.
3. Budoff, M., Achenbach, S., Narula, J. Atlas of cardiovascular computed tomography. Philadelphia: Current Medicine; 2007.
4. Cronin, P., Sneider, M.B., Kazerooni, E.A., et al. MDCT of the Left Atrium and Pulmonary Veins in Planning Radiofrequency Ablation for Atrial Fibrillation: A How-To Guide. Am J Roentgenol. 2004;183:767–778.
5. Hoffmann, U., Bamberg, F., Chae, C.U., et al. Coronary Computed Tomography Angiography for Early Triage of Patients With Acute Chest Pain – The ROMICAT (Rule Out Myocardial Infarction Using Computer Assisted Tomography) Trial. J Am Coll Cardiol. 2009;53:1642–1650.
6. Lu, M., Chen, J.J., Awan, O., et al. Evaluation of Bypass Grafts and Stents. Radiol Clin N Am. 2010;48:757–770.
7. Schoepf, U.J. CT of the heart: principles and applications, ed 2. Totowa, NJ: Humana Press; 2008.
8. Taylor, A.J., Cerqueira, M., Hodgson, J., et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Appropriate Use Criteria for Cardiac Computed Tomography: A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2010;56:1864–1894.
9. Zadeh, A.A., Miller, J.M., Rochitte, C.E., et al. Diagnostic Accuracy of Computed Tomography Coronary Angiography According to Pre-Test Probability of Coronary Artery Disease and Severity of Coronary Arterial Calcification – The CORE-64 International Multicenter Study. J Am Coll Cardiol. 2012;59:379–387.




