Tube Carcinoma, Primary Fallopian
Synonyms/Description
Tubal carcinoma/malignancy
Etiology
Primary fallopian tube carcinoma (PFTC) is among the rarest gynecologic malignancies, accounting for 0.3% of all gynecologic cancers, and is usually seen in postmenopausal women. There is recent evidence that the majority of high-grade, papillary serous cancers involving the ovary may actually originate in the fallopian tube, then spread to the ovary. There is a precursor lesion of the fallopian tube called serous intraepithelial tubal carcinoma (STIC) that is similar to high-grade ovarian serous adenocarcinoma. Recent research suggests that many ovarian cancers originate from a STIC in the fimbriated end of the fallopian tube. Histologically, up to 90% of tubal cancers are adenocarcinomas, most of which are serous adenocarcinomas. A minority of cases are endometrioid and clear cell adenocarcinoma. The risk factors for tubal cancer are similar to ovarian, including the inheritance of the BRCA 1 and BRCA 2 gene mutations. Approximately 15% to 45% of women with fallopian tube cancer are positive for one of these two mutations. Although the symptoms are nonspecific and may include pain and bleeding, tubal cancer has historically been associated with a characteristic watery vaginal discharge. The Latzko triad includes serosanguineous discharge, colicky pelvic pain, and a mass. Although this triad of symptoms is considered characteristic of tubal cancers, it occurs in only 15% of affected patients.
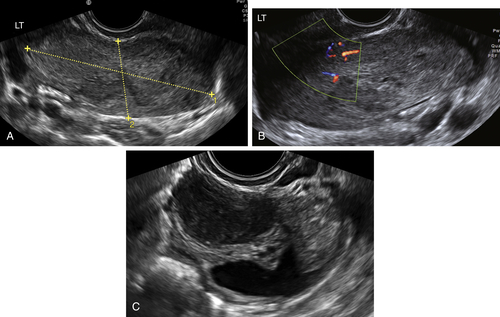
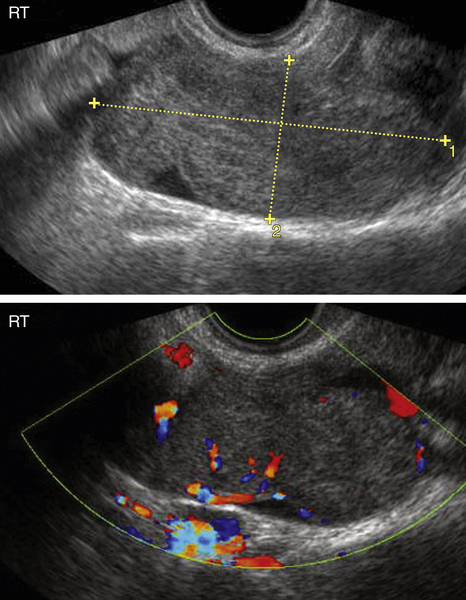
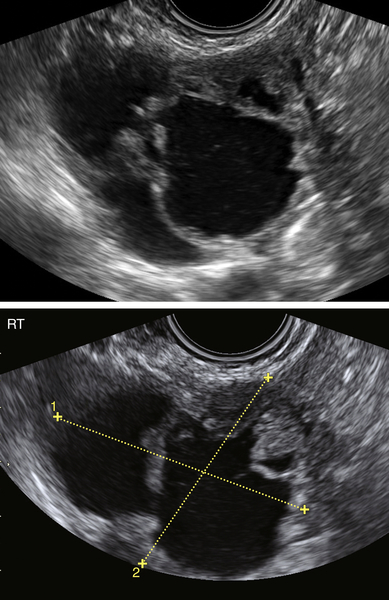
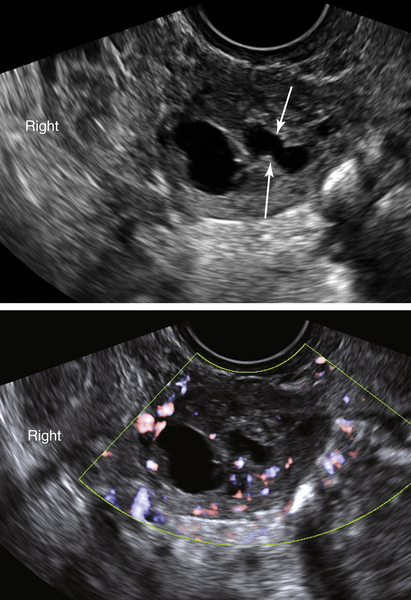
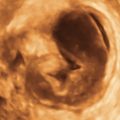
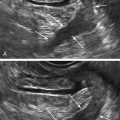
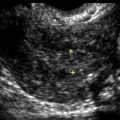
Ultrasound Findings
The sonographic appearance of tubal carcinoma is very similar to ovarian cancer. There is usually a complex but largely solid adnexal mass with cystic components and abundant blood flow. The mass may be sausage-shaped, suggesting that it may be tubal, but in most cases the ovary is not seen separately. Although hydrosalpinges have a characteristic appearance of incomplete septa and a spoke-wheel pattern, tubal cancers typically have a large solid component obscuring any distinctive features of the tube. Most patients with tubal cancer are presumed preoperatively to have an ovarian malignancy; thus it is rare to make the correct diagnosis prospectively. In a study by Slanetz and colleagues, only 3 of 20 patients were correctly diagnosed sonographically with primary tubal cancer, whereas the others were presumed to be of ovarian origin. These authors also report that the fallopian tube can be a site for metastatic disease from distant primaries.
Differential Diagnosis
The differential diagnosis for tubal cancer is similar to the one for ovarian cancer. The sonographic finding of a complex solid and cystic mass with abundant color flow Doppler and shaggy borders suggests a malignancy. Whether the mass is a tubal, ovarian, or metastatic tumor is indeterminate sonographically. Rarely, there are benign masses that can mimic a tubal or ovarian cancer, such as cystadenofibromas or cystadenomas, with small solid excrescences that may suggest a malignancy. There can also be unusual-appearing degenerating fibroids or complex endometriomas with irregular borders that occasionally simulate a cancer. Generally, tubal cancers tend to be large, multilocular, partly solid, and vascular when discovered, making the diagnosis of a malignancy likely.