67
Candidiasis (moniliasis)

Macerated scale and fissuring favor interdigital involvement.

Satellite papules within the moist environment of body folds.
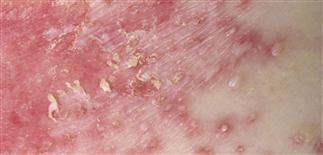
Papules coalescing into plaques studded with pustules and fragile scale.

Mucosal involvement with exudates and overgrowth of Candida. Diabetes is a predisposing factor.
DESCRIPTION
Skin and mucosal infection caused primarily by Candida albicans.
HISTORY
• Candida species live among the normal flora of the mouth, vaginal tract, lower gastrointestinal tract. Candida reproduces through the budding of oval yeast forms, forming elongated pseudohyphae. The yeast infects only the outer layers of the epithelium of mucous membrane and skin (stratum corneum). Yeast grows best in a warm, moist environment. Infection usually confined to mucous membranes and intertriginous areas. • Factors that predispose to infection include infancy, pregnancy, oral contraceptive use, systemic antibiotic therapy, diabetes, skin maceration, topical and systemic steroid therapy, decreased cell-mediated immunity.
PHYSICAL FINDINGS
• Primary lesion is a superficial pustule. The contents of the pustule dissect horizontally under the stratum corneum and peel it away. Clinically, this process results in a red, denuded, glistening surface with a long, cigarette paper-like scaling and advancing border. Itching and burning are common symptoms. • In potassium hydroxide wet mount preparation and culture, the pseudohyphae and hyphae may be difficult to distinguish from dermatophytes. • Culture results must be interpreted carefully, because the yeast is part of the normal flora in many areas. • Nickerson’s media is used to isolate and identify Candida species.
TREATMENT
Azole antifungal creams such as miconazole, clotrimazole, ketoconazole, oxiconazole, or econazole effective. Apply cream twice daily for 7 days. A single 150-mg dose of fluconazole also effective. Use caution in diabetic patients on oral hypoglycemic agents.







