18 Cancers of unknown primary
Evaluation
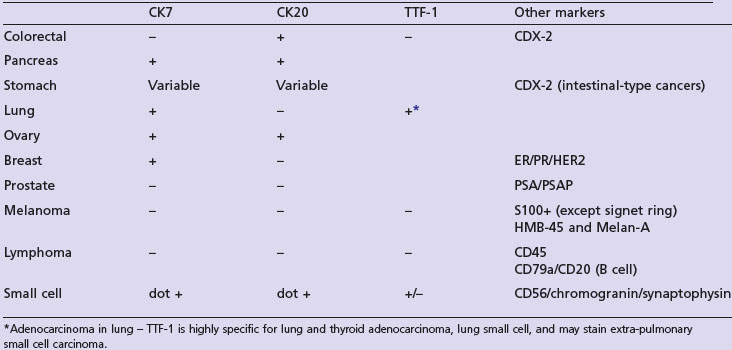
Clinicopathological evaluation aims to identify a primary site, a clinicopathological subset and to rule out non-epithelial tumours. The first step includes clinical history to establish risk factors, clinical examination, investigations and pathological evaluation. Initial investigations include blood tests, urinalysis, faecal occult blood test and CT scan of the chest, abdomen and thorax. Endoscopic evaluation is guided by symptoms and/or signs. In patients suspected to have extragonadal germ cell tumours a serum beta-hCG and AFP should be estimated. Other tumour markers depending on the clinical context include PSA, CEA, CA-125 and CA19-9. Pathological evaluation includes light microscopy and expedient use of immunohistochemical techniques. Immunohistochemistry is useful in differentiating epithelial from non-epithelial tumours, such as sarcoma and lymphoma (Table 18.1). The majority of epithelial tumours are adenocarcinoma (65–80%) followed by squamous cell carcinoma (10–15%) and undifferentiated carcinoma (5–10%).
The outcome of first step evaluation is identification of a specific clinicopathological entity which may be a favourable (15% patients) or unfavourable (85% patients) (Box 18.1).
Management
Women with isolated axillary lymphadenopathy
Women presenting like this are treated like stage II breast cancer. Previous studies showed an occult primary in 50–60% of cases after mastectomy. However, if MRI of the breast failed to show any primary, breast surgery or radiotherapy may not be warranted. Axillary lymphadenopathy is treated with lymph-node dissection followed by regional radiotherapy based on breast cancer radiotherapy principles (p. 124). Adjuvant systemic treatment is similar to stage II breast cancer. The reported 5-year survival for patients with 1–3 nodes are 87% and those with >3 nodes are 42%.
Women with peritoneal carcinomatosis
Women with peritoneal carcinomatosis are treated like stage III ovarian cancer with initial cytoreduction followed by combination chemotherapy or vice versa depending on performance status and co-morbidities (p. 201). CA-125 may be used as a tumour marker if elevated and the reported long-term survival is 15%.
Patients presenting with inguinal lymphadenopathy
In this group of patients investigations are to rule out a primary site in the perineal area. If no primary tumour is detected, treatment is node dissection with or without postoperative radiotherapy.
Pavlidis N, Fizazi K. Carcinoma of unknown primary (CUP). Crit Rev Oncol Hematol. 2009;69:271-278.
Greco FA, Erlander MG. Molecular classification of cancers of unknown primary site. Mol Diagn Ther. 2009;13:367-373.
Morris GJ, Greco FA, Hainsworth JD, et al. Cancer of unknown primary site. Semin Oncol. 2010;37:71-79.
Varadhachary GR, Abbruzzese JL, Lenzi R. Diagnostic strategies for unknown primary cancer. Cancer. 2004;100:1776-1785.
Pavlidis N, Briasoulis E, Pentheroudakis. Cancer of unknown primary site: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21(suppl 5):v228-v231.