CHAPTER 4 Cam-Type Femoroacetabular Impingement
Surgical correction of various hip impingement problems was described even early in the last century.1,2 In 1975, Harris and coauthors described the pistol grip deformity of the femoral head observed in association with early-onset osteoarthritis.3 In 1998, we described arthroscopic correction of impingement caused by post-traumatic osteophytes and also reported an arthroscopic technique of cheilectomy for femoral protuberances associated with Legg-Calvé-Perthes disease.4,5 However, it was Myers, Ganz, Lavigne and colleagues6–8 who formulated the concept of femoroacetabular impingement, describing pincer, cam, and combined types. Subsequently, we have reported arthroscopic methods for correcting this disorder.9–11
We have identified a bimodal population of patients with cam-type femoroacetabular impingement (FAI).11 One is the typical middle-aged patient (average age, 43 years, with a 1.9:1 male-to-female ratio) who presents with early-onset osteoarthritis. The second population is much younger, with an even greater male preponderance (average age, 20 years, with 3.1:1 male-to-female ratio) and most (70%) are involved in athletic activities. These are active individuals who have pushed their hip beyond its diminished physiologic limits and have sustained substantial joint breakdown at a young age.
ANATOMY AND PATHOANATOMY
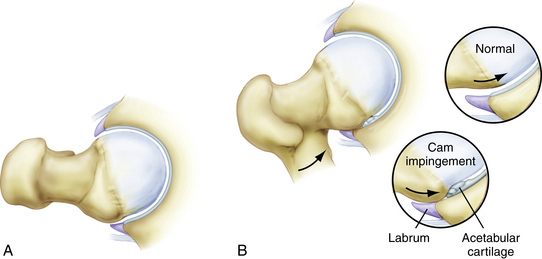
Cam-type FAI refers to the cam effect created by a nonspherical femoral head. During flexion, the prominence of the out-of-round portion rotates into the acetabulum, engaging against its surface and resulting in delamination and failure of the acetabular articular cartilage (Fig. 4-1). Early in the disease process, the labrum is relatively preserved but, with time, it begins to sustain secondary damage.
Cam impingement is classically attributed to a slipped capital femoral epiphysis, resulting in a bony prominence of the anterior and anterolateral head-neck junction. However, the most common cause is the pistol grip deformity, attributed to a developmental abnormality of the capital physis during growth. The exact cause is unclear; it may represent premature asymmetrical closure of the physis; it has been postulated that this could be caused by late separation of the common proximal femoral growth plate that forms the physis of the greater trochanter and femoral head.12
HISTORY AND PHYSICAL EXAMINATION
Patients with cam impingement have typical hip joint–type symptoms.13 The onset may be gradual or associated with an acute episode, which is the culmination of altered wear developing over a protracted period of time. Patients with cam impingement usually have reduced joint motion, which can result in other secondary disorders. Athletes compensate with increased pelvic motion, often resulting in problems with athletic pubalgia.14 More stress is placed on the lumbar spine, resulting in concomitant lumbar disease.
Pain with flexion, adduction, and internal rotation is almost uniformly present and is referred to as the impingement test (Fig. 4-2).7 However, in our experience, this maneuver is uncomfortable for most irritable hips, regardless of the underlying cause, and thus is not specific for impingement. Laterally based cam lesions may result in painful abduction or external rotation (Fig. 4-3). Internal rotation of the flexed hip is usually diminished, but may be preserved in some patients (Fig. 4-4). Limited range of motion may be present bilaterally because the morphologic variation is often present in both hips.
DIAGNOSTIC IMAGING
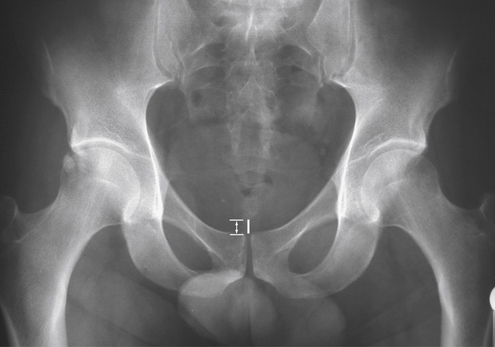
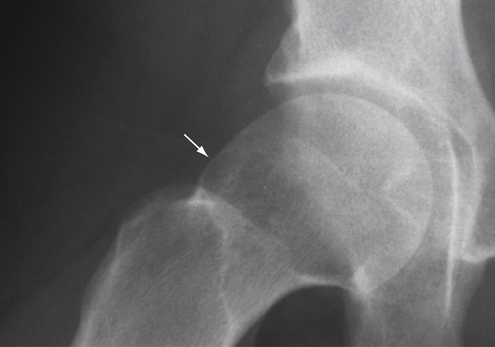
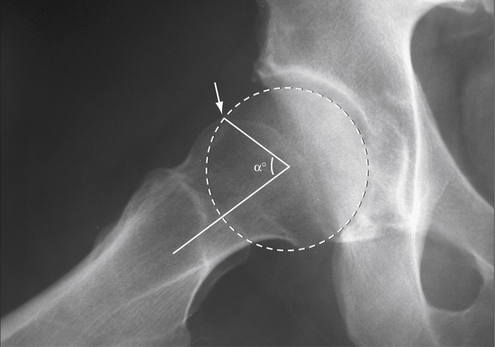
Radiographs are essential for the routine evaluation of impingement. A well-centered anteroposterior (AP) pelvis x-ray is important for assessing the acetabular indices of pincer impingement, but also allows observations on the cam lesion comparing both hips (Fig. 4-5).15 The epicenter and shape of the cam lesion are variable. Thus, although the 40-degree Dunn view has been reported as the best image, we have found that no single lateral radiographic view is reliable for optimally assessing the cam lesion in all cases (Fig. 4-6).16 Sometimes, the cam lesion is more anteriorly based and sometimes more lateral. The characteristic feature is loss of sphericity of the femoral head. The alpha angle has been described to quantitate this observation (Fig. 4-7).17 However, imaging will underinterpret this measurement unless it catches the maximal location of the cam lesion. Also, no studies have shown a significant correlation between the amount of correction of the alpha angle and the results of surgery, indicating that there may be other factors at play.
Magnetic resonance imaging (MRI) and gadolinium arthrography with MRI (MRA) aid in assessing secondary damage to the articular cartilage and labrum associated with cam impingement.18 These studies are better at detecting labral pathology but reveal the severity of articular involvement less often. The alpha angle can again be recorded, but is still variable, depending on whether the cross-sectional images catch the maximal location of the cam lesion.
INDICATIONS AND CONTRAINDICATIONS
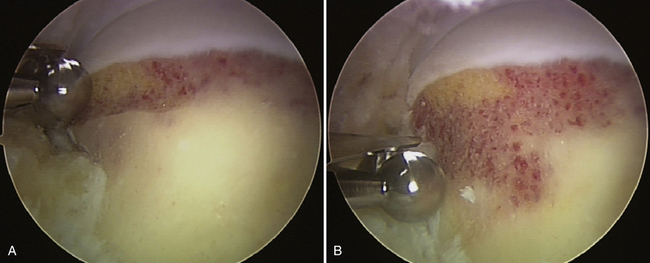
The indication for hip arthroscopy is imaging evidence of intra-articular pathology amenable to arthroscopic intervention, or sometimes recalcitrant hip pain that remains refractory to efforts at conservative treatment. It must be kept in mind that imaging studies may often underestimate the severity of intra-articular pathology. Correction of an accompanying cam lesion has been performed, when present, especially when there was arthroscopic evidence that it was responsible for the concomitant joint pathology. This secondary joint damage is best characterized by failure of the anterolateral acetabular articular surface. The failure is most typically represented by articular delamination with the peel-back mechanism, but earlier in the disease process may be characterized by deep, closed, grade I articular blistering, referred to as the wave sign.19
It is our opinion that radiographic findings of impingement, in the absence of clinical findings of a joint problem, are not solely an indication for arthroscopy. Some individuals with impingement morphology may function for decades without developing secondary joint damage and symptoms. For some, it is unclear when, or if, they will develop problems warranting surgical intervention. For example, many individuals may present with symptoms in one hip when radiographic findings of impingement are present in both. Although intervention in the asymptomatic joint would not be appropriate, it is important to educate the patient about warning signs of progressive joint damage. It is a clinical challenge in the decision not to intercede too early or too late. In our experience, 93% of patients undergoing arthroscopy for cam impingement demonstrate Grade III or IV articular damage, reflecting that the disease process is already substantially advanced at the time of intervention.11
Contraindications include advanced disease states, such as grade III Tonnis changes, and sometimes there are patients who do not have reasonable expectations of what can be accomplished with the procedure.20 Because the success of the operation is ultimately dictated by the patient’s impressions, it may be important to modulate the patient’s goals. Also, in the presence of secondary degenerative disease, the potential advantages of a joint-preserving procedure must be weighed against the high level of satisfaction associated with arthroplasty procedures.
TREATMENT
Conservative Management
Conservative management begins with an emphasis on early recognition of the underlying impingement disorder. The mainstay of treatment is identifying and modifying offending activities that precipitate symptoms. Some individuals can modify their lifestyles and stabilize the process for years. Efforts can be made to optimize mobility of the joint, but these are only modestly effective because motion is limited by the bony architecture, which cannot be corrected with manual techniques. Decompensatory disorders are those secondary problems that develop as individuals struggle to compensate for the chronic limitations imposed by the impingement. A conservative strategy must include assessment and treatment of the secondary problems, which can contribute substantially to the patient’s symptoms.
Surgical Technique
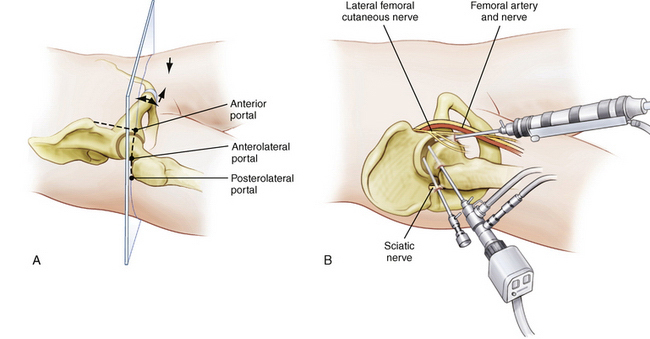
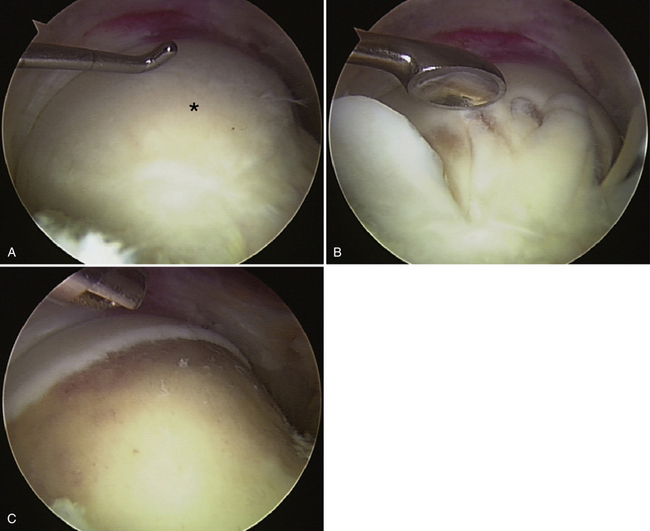
The procedure begins with arthroscopy of the central compartment to assess for the pathology associated with cam impingement. This is carried out with the standard supine three-portal technique that has been well described in the literature (Fig. 4-8).21–23 The characteristic feature of pathologic cam impingement is articular failure of the anterolateral acetabulum. The femoral head remains well preserved until late in the disease course. Early stages of the disease are characterized by closed grade I chondral blistering, which sometimes must be distinguished from normal articular softening. Our experience has been that most patients already have grade III or IV acetabular changes by the time of surgical intervention.11 The articular surface is seen to separate or peel away from its attachment to the labrum (see Fig. 4-16D); this is caused by the shear effect of the cam lesion. The labrum may be relatively well preserved but, with time, progressive fragmentation occurs. Often, the damaged articular surface of the labrum can be selectively débrided, preserving the capsular margin and potentially some of its labral seal function. If there is good-quality tissue that has been detached, repair can be performed with suture anchors. In cases of combined impingement with concomitant pincer lesions, the acetabulum is reshaped, either by takedown and subsequent refixation of the labrum or by débridement when the labral damage is advanced. The articular pathology is addressed with chondroplasty and microfracture as dictated by its severity.
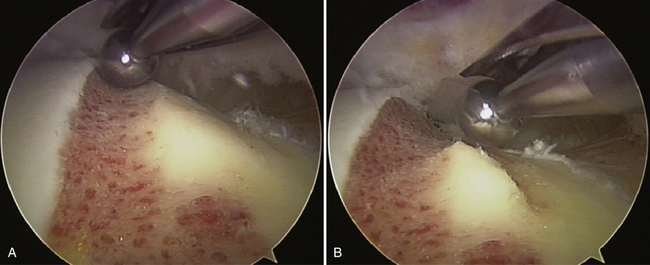
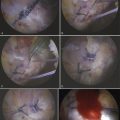
After completing arthroscopy of the central compartment, the cam lesion is addressed from the peripheral compartment. A capsulotomy is created by connecting the anterior and anterolateral portals (Fig. 4-9). The posterolateral portal can be removed and the anterior and anterolateral cannulas are backed out of the central compartment. The traction is released and the hip is flexed approximately 35 degrees. As the hip is flexed under arthroscopic visualization, the line of demarcation between healthy femoral cartilage and abnormal fibrocartilage that covers the cam lesion can usually be identified.
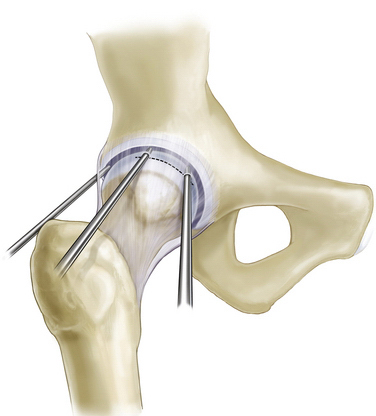
A cephalad anterolateral portal is established approximately 5 cm above the anterolateral portal, entering through the capsulotomy that has already been established. These proximal and distal anterolateral portals work well for accessing and addressing the cam lesion (Fig. 4-10). The anterior portal can be removed or maintained if it is needed for better access to the medial side of the femoral neck.
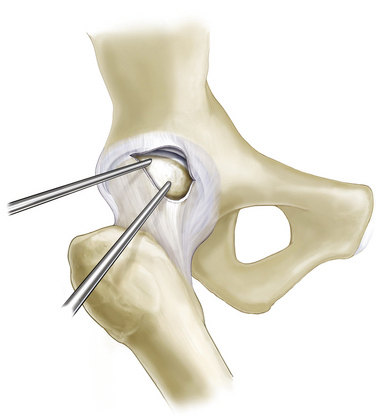
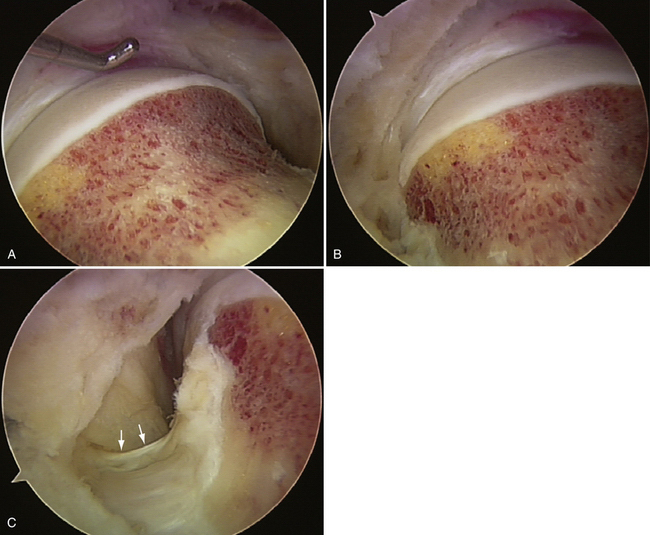
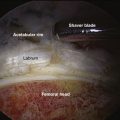
Most of the work for performing the recontouring of the cam lesion (femoroplasty) lies in the soft tissue preparation. This includes capsular débridement, as necessary, to ensure complete visualization of the lesion and then removal of the fibrocartilage and scar that cover the abnormal bone (Fig. 4-11). With the hip flexed, the proximal portal provides better access for the lateral and posterior portion, whereas the distal portal is more anterior relative to the joint and provides the best access for the anterior part of the lesion. The lateral synovial fold is identified as the arthroscopic landmark for the retinacular vessels, and care is taken to preserve this structure during the recontouring (Fig. 4-12). Switching between the portals is important for full appreciation of the three-dimensional anatomy of the recontouring.
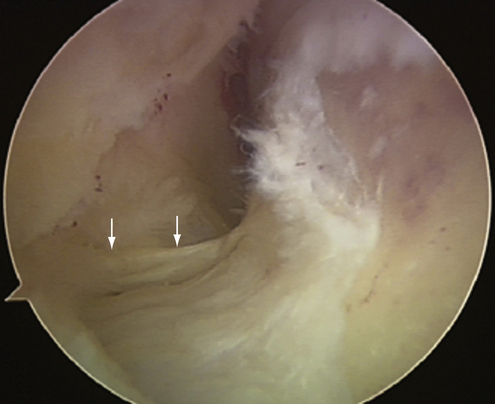
FIGURE 4-12 Viewed laterally, underneath the area of the lateral capsulotomy, the lateral synovial fold (arrows) is identified along the lateral base of the neck, representing the arthroscopic landmarks of the lateral retinacular vessels.
Once the bone has been fully exposed, recontouring is performed with a spherical burr. The goal is to remove the abnormal bone identified on the preoperative CT scan and re-create the normal concave relationship that should exist where the femoral neck meets the articular edge of the femoral head. It is best to begin by creating the line and depth of resection at the articular margin. The resection is then extended distally, tapering with the normal portion of the femoral head (Figs. 4-13 and 4-14). We recommend beginning the resection at the lateral posterior limit of the cam lesion, with the arthroscope in the more distal portal and instrumentation in the more proximal portal. The posterior extent of the resection is usually the most difficult; the resection is also the most critical to avoid notching the tensile surface of the femoral neck, and particular attention must be given to avoiding and preserving the lateral retinacular vessels. Then, switching the arthroscope to the proximal portal, the burr is introduced distally and the reshaping is completed along the anterior head and neck junction. Finally, attention is given to ensure that all bone debris is removed as thoroughly as possible to lessen the likelihood of developing heterotopic ossification. The quality of the recontouring is assessed and preservation of the lateral retinacular vessels is confirmed (Fig. 4-15).
PEARLS& PITFALLS
Case Reports
Case 1
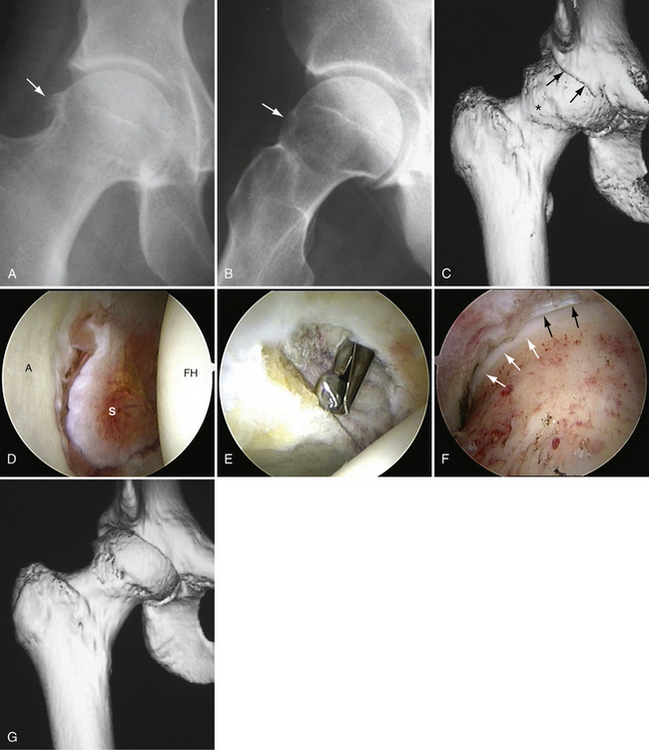
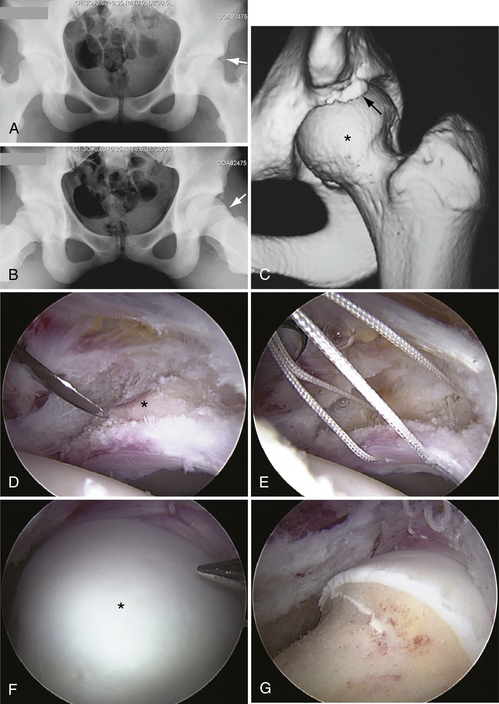
A 20-year-old hockey player was evaluated, with a 4-year history of worsening right groin pain. Examination revealed diminished internal rotation of both hips (10 degrees). Forced flexion, adduction, and internal rotation of the right hip re-created the characteristic pain that he experienced with activities (Fig. 4-16).
Case 2
A 38-year-old woman presented with a 3-year history of progressively worsening pain and loss of motion of both hips, right worse than left. Symptoms were initially precipitated by horseback riding, but have now become troublesome with daily activities. Examination revealed an antalgic gait. Range of motion was restricted in both hips (35 degrees external rotation, 5 degrees internal rotation), with pain at all end ranges (Fig. 4-17).
Case 3
A 15-year-old level 10 female gymnast presented with a 6-month history of left hip pain unresponsive to conservative treatment, including a protracted period of rest. Examination revealed a 20-degree loss of motion of the left hip compared with the right, with pain re-created on flexion, adduction, and internal rotation (Fig. 4-18).
OUTCOMES
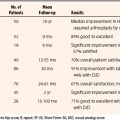
We have reported on 200 patients (207 hips) with 100% follow-up at 1 to 2 years.11 The average age was 33 years (range, 13 to 63 years). There were 138 males and 62 females, with 120 right and 87 left hips, and 163 patients underwent femoroplasty to correct cam impingement alone, whereas 44 patients underwent femoroplasty combined with correction of associated pincer impingement. Overall, the average improvement was 20 points (preoperative, 66; preoperative, 86). Using the Harris classification, 83% were improved, with 83% good and excellent results Viewing the results over time (see Fig. 4-8), continued improvement was noted throughout the first year, with results maintained in those with 2-year follow up. Most had Outerbridge grade IV (107) or grade III (83) articular damage on at least one side of the joint, and 58 underwent microfracture, with an average 20-point improvement (preoperative, 65; postoperative, 85). Comparing the results of cam and combined lesions, the results were comparable, with 20- versus 19-point improvement. The cam patients tended to be slightly younger, with an average age of 33 versus 35 years for combined lesions. A bimodal age distribution was identified, with a peak at age 20 and a second peak at age 43 years; 94 (45%) were sports-related. For those patients younger than 30 (N = 88), 62 (70%) were associated with athletic activities; after the third decade (N = 119), only 30 (25%) were associated with athletics. The under 30 group was also more male-dominated, with a male-to-female ratio of 3.1:1 compared with the over 30 group, with a male-to-female ratio of 1.9:1. One patient (0.5%) was converted to a total hip arthroplasty whereas 3 patients underwent a second arthroscopic procedure. There were three complications, but none were significant. There was one each of a transient neuropraxia of the pudendal nerve and lateral femoral cutaneous nerve, which resolved uneventfully. One patient was incidentally noted to have developed heterotopic ossification within the capsule, which did not preclude a successful outcome.
Other authors have reported outcomes of arthroscopic management of FAI specifically in regard to correction of the cam lesion. Ilizaliturri and colleagues have reported improvement in 16 of 19 patients (84%), with a minimum 2-year follow-up.24 Bardakos and associates25 have reported on femoral osteoplasty in 24 patients with 1-year follow-up compared with a control group in which arthroscopic débridement was performed without excising the impingement lesion. The modified Harris hip score was better in the study group (83) compared with the control group (77), and there was a significantly higher proportion of good to excellent results in the study group (83%) compared with the control group (60%). Brunner and coworkers26 have reported on 45 athletically active individuals; 31 (69%) were able to resume their activities, with an average 2.4-year follow-up.
SUMMARY
The arthroscope is instrumental in the treatment algorithm for cam impingement. Because cam morphology can exist in the absence of secondary associated joint pathology, the arthroscopic findings substantiate the need for correction of the underlying impingement. Most cases of cam impingement can be addressed arthroscopically. This is a technically demanding procedure that requires meticulous preparation for visualizing the cam lesion and careful orientation in recontouring of the bone to avoid inadequate or excessive resection. The results of the arthroscopic approach are at least comparable to those of the open method, with few complications. Successful results can be expected in most patients, including athletes and individuals seeking to return to an active lifestyle, with low morbidity.
1. Vulpius O, Stoffel A. Orthopaadische Operationslehre. Stuttgart, Germany: F. Enke; 1913.
2. Smith-petersen MN. Treatment of malum coxae senilis, old slipped upper femoral epiphysis, intrapelvic protrusion of the acetabulum, and coxa plana by means of acetabuloplasty. J Bone Joint Surg Am. 1936;18:869-880.
3. Stulberg SD, Cordell LD, Harris WH, et al. Unrecognized childhood hip disease: a major cause of idiopathic osteoarthritis of the hip. In: Hip Society, ed. The Hip: Proceedings of the Third Open Scientific Meeting of the Hip Society. St. Louis: Mosby; 1975:212-228.
4. Byrd JWT. Arthroscopy of select hip lesions. In: Byrd JWT, editor. Operative Hip Arthroscopy. New York: Thieme; 1998:153-170.
5. Byrd JWT. Hip arthroscopy: evolving frontiers, Special Issue. Novel Techniques in Hip Surgery. Oper Tech Orthop. 2004;14:58-67.
6. Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:81-92.
7. Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement. a cause for osteoarthritis in the hip. Clin Orthop Relat Res. 2003;417:112-120.
8. Lavigne M, Parvizi J, Beck M, et al. Anterior femoroacetabular impingement. part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61-66.
9. Byrd JWT. Hip morphology and related pathology. In: Johnson DH, Pedowitz RA, editors. Practical Orthopaedic Sports Medicine and Arthroscopy. Philadelphia: Lippincott, Williams & Wilkins; 2007:491-503.
10. Byrd JWT, Jones KS. Arthroscopic management of femoroacetabular impingement. Instr Course Lect. 2009;58:231-239.
11. Byrd JWT, Jones KS. Arthroscopic “femoroplasty” in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:739-746.
12. Siebenrock KA, Wahab KHA, Werlen S, et al. Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Orthop Relat Res. 2004;418:54-60.
13. Byrd JWT. Physical examination. In: Byrd JWT, editor. Operative Hip Arthroscopy. 2nd ed. New York: Springer; 2005:36-50.
14. Meyers WC, Foley DP, Garrett WE, et al. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28:2-8.
15. Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg. 2007;15:561-570.
16. Meyer DC, Beck M, Ellis T, et al. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181-185.
17. Notzli H, Wyss TF, Stoecklin CH, et al. The contour of the femoral head/neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556-560.
18. Byrd JWT, Jones KS. Diagnostic accuracy of clinical assessment, MRI, gadolinium MRI, and intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32:1668-1674.
19. Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25:299-308.
20. Tonnis D, Heinecke A. Acetabular and femoral anteversion. relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747-1770.
21. Byrd JWT. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10(3):275-280.
22. Byrd JWT. The supine approach. In: Byrd JWT, editor. Operative Hip Arthroscopy. 2nd ed. New York: Springer; 2005:145-169.
23. Byrd JWT. Hip arthroscopy by the supine approach. Instr Course Lect. 2006;55:325-336.
24. Ilizaliturri VM, Orozco-Rodriguez L, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of cam-type femoroacetabular impingement. J Arthroplasty. 2008;23:226-234.
25. Bardakos NV, Vasconcelos JC, Villar RN. Early outcome of hip arthroscopy for femoroacetabular impingement. the role of femoral osteoplasty in symptomatic improvement. J Bone Joint Surg Br. 2008;90:1570-1575.
26. Brunner A, Horisberger M, Herzog RF. Sports and recreation activity of patients with femoroacetabular impingement before and after arthroscopic osteoplasty. Am J Sports Med. 2009;37:917-922.