Calcium regulation and hypocalcaemia
Calcium homeostasis
The amount of calcium present in the extracellular fluid is very small in comparison to that stored in bone. Even in the adult, calcium in bone is not static; some bone is resorbed each day and the calcium returned to the ECF. To maintain calcium balance, an equal amount of bone formation must take place. Figure 35.1 shows how much calcium is exchanged between one compartment and another daily.
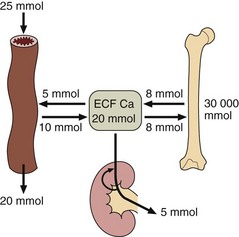
Fig 35.1 Normal calcium balance. Calcium is exchanged each day, in the amounts shown, between the extracellular fluid and the gut, bone and kidney.
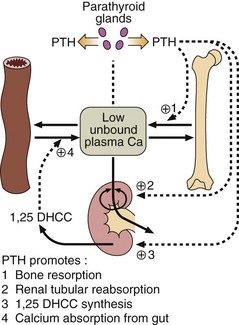
Calcium homeostasis is modulated by hormones (Fig 35.2). Parathyroid hormone (PTH), which consists of 84 amino acids, is secreted from the parathyroid glands in response to a low unbound plasma calcium. PTH causes bone resorption and promotes calcium reabsorption in the renal tubules, preventing loss in the urine. 1,25-dihydroxycholecalciferol (1,25 DHCC) maintains intestinal calcium absorption. This sterol hormone is formed from vitamin D (cholecalciferol), following hydroxylation in the liver (at carbon-25) and kidney (at carbon-1). However, hydroxylation in the kidney is PTH dependent, and so even the absorption of calcium from the gut relies (albeit indirectly) on PTH.
Serum calcium
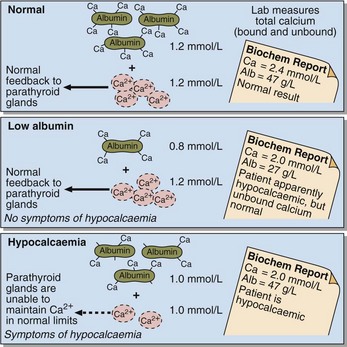
Laboratories routinely measure total calcium concentration (that is both the bound and unbound fractions) in a serum sample. However, this may give rise to problems in the interpretation of results because changes in serum albumin concentration cause changes in total calcium concentration. If albumin concentration falls, total serum calcium is low because the bound fraction is decreased (Fig 35.3). Remember that the homeostatic mechanisms for regulating plasma calcium respond to the unbound fraction, not to the total calcium. Patients with a low albumin have total serum calcium lower than the reference values, yet have normal unbound calcium. These patients should not be thought of as hypocalcaemic.
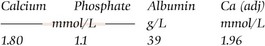
Adjusted calcium (mmol/L) = Total measured calcium + 0.02(47– albumin)
Hypocalcaemia
The causes of hypocalcaemia include:
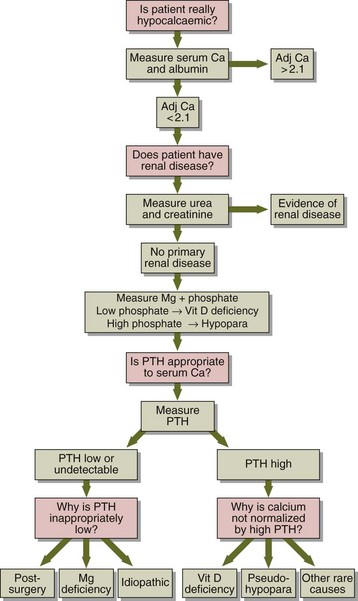
 Vitamin D deficiency. This may be due to malabsorption, or an inadequate diet with little exposure to sunlight. It may lead to the bone disorders, osteomalacia in adults and rickets in children (see pp. 76–77).
Vitamin D deficiency. This may be due to malabsorption, or an inadequate diet with little exposure to sunlight. It may lead to the bone disorders, osteomalacia in adults and rickets in children (see pp. 76–77).
 Magnesium deficiency. This is a common cause in hospital patients.
Magnesium deficiency. This is a common cause in hospital patients.
 Renal disease. The diseased kidneys fail to synthesize 1,25 DHCC (see pp. 28–29). Increased PTH secretion in response to the hypocalcaemia may lead to bone disease if untreated.
Renal disease. The diseased kidneys fail to synthesize 1,25 DHCC (see pp. 28–29). Increased PTH secretion in response to the hypocalcaemia may lead to bone disease if untreated.
 Hungry bone syndrome. There can be severe and potentially fatal hypocalcaemia with accompanying hypophosphataemia after parathyroidectomy, due to rapid remineralization of bone (after sudden decrease in PTH), especially after long-standing primary hyperparathyroidism with severe bone disease.
Hungry bone syndrome. There can be severe and potentially fatal hypocalcaemia with accompanying hypophosphataemia after parathyroidectomy, due to rapid remineralization of bone (after sudden decrease in PTH), especially after long-standing primary hyperparathyroidism with severe bone disease.
 Pseudohypoparathyroidism. PTH is secreted but there is failure of target tissue receptors to respond to the hormone.
Pseudohypoparathyroidism. PTH is secreted but there is failure of target tissue receptors to respond to the hormone.
 Rarer causes such as malignancy, acute rhabdomyolysis, acute pancreatitis, ethylene glycol poisoning or bone marrow transplantation.
Rarer causes such as malignancy, acute rhabdomyolysis, acute pancreatitis, ethylene glycol poisoning or bone marrow transplantation.