C
CAB Cellulose acetate butyrate is a transparent thermoplastic material that is used in the manufacture of gas permeable contact lenses as it transmits some oxygen. It is a copolymer with varying percentages of cellulose, butyryl and acetyl. CAB lenses vary in their characteristics depending on the percentages of the three components. It is also used to make spectacle frames.
‘café au lait’ spots See disease, von Recklinghausen’s.
calcarine fissure See fissure, calcarine.
caliper A device used to measure distances between structures or surfaces. It usually comprises a scale at one end, while at the other end are two legs, which can be adjusted to the appropriate measurement. Example: lens thickness caliper.
caloric nystagmus See caloric testing.
caloric testing A neuro-ophthalmic technique in which cold and warm water is used to stimulate the vestibular system creating horizontal nystagmus (called caloric nystagmus or Barany’s nystagmus). Cold water placed in the ear induces a fastbeating vestibular nystagmus with the fast phase moving away from the stimulated ear, while warm water causes the fast phase to move in the direction of the stimulated ear. The mnemonic COWS (cold–opposite, warm–same) is used to describe this effect. By placing the subject at a 30-degree upright position, heated or cooled water stimulates the now vertical horizontal semicircular canals.
camera, fundus A camera attached to an indirect ophthalmoscope aimed at photographing the image of the fundus of the eye. This image is produced by the objective of the ophthalmoscope at the first focal point of the objective of the viewing microscope (and of the camera), which forms an image on the film. A flip mirror within the optical path of the viewing microscope allows the observer to view the image of the fundus and focus it, thus ensuring that the image being photographed is as clear as that being viewed. Fundus cameras usually require a dilated pupil of about 4 mm and their fields of view extend up to 45°. They provide an objective photographic record of any condition in the fundus. They can also be used to take photographs of the anterior segment of the eye.
See fundus, ocular; ophthalmoscope, indirect; ophthalmoscope, scanning laser.
camera obscura See camera, pinhole.
camera, pinhole A camera in which the lens is replaced by a pinhole (e.g. the camera obscura).
campimeter An instrument for the measurement of the visual field, especially the central region (usually within a radius of 30°).
See analyser, Friedmann visual field; chart, Amsler; perimeter; screen, tangent.
campimetry Measurement of the visual field with a campimeter.
Canada balsam A transparent resinous substance produced by the sap of the Canadian balsam fir and used to cement glass (doublet, beam-splitting prisms, the segment of a bifocal lens, etc). Its index of refraction is equal to about 1.54. It has nowadays been superseded by modern chemical adhesives.
canal A tubular channel which allows the passage of air, food, blood, excretions, secretions, or anatomical structures such as nerves or blood vessels.
Cloquet’s c. See canal, hyaloid.
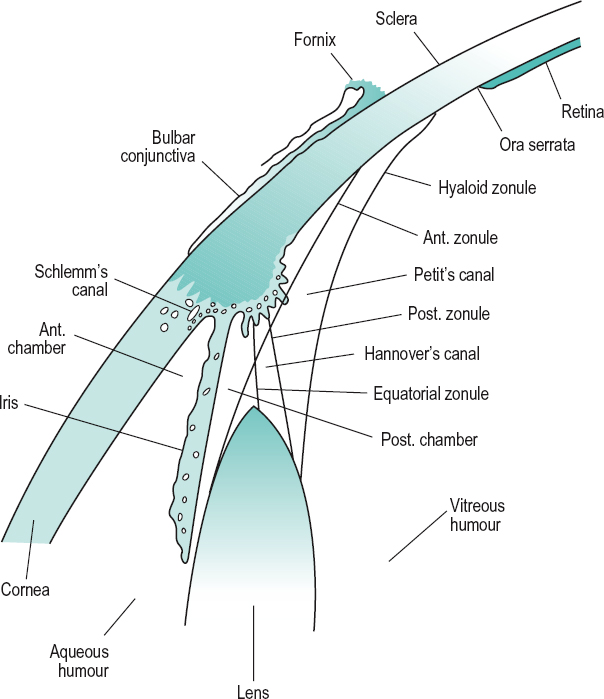
Hannover’s c . A space about the equator of the crystalline lens made up between the anterior and posterior parts of the zonule of Zinn and containing aqueous humour and zonular fibres (Fig. C1).
hyaloid c. A channel in the vitreous humour, running from the optic disc to the crystalline lens. In fetal life this canal contains the hyaloid artery, which nourishes the lens, but it usually disappears prior to birth. Syn. central canal; Cloquet’s canal; Stilling’s canal.
See hyaloid remnant.
infraorbital c. A channel beginning at the infraorbital groove in the floor of the orbit and ending at the infraorbital foramen of the maxillary bone opening onto the face below the inferior orbital margin. It is a channel for the infraorbital artery and the infraorbital nerve.
nasolacrimal c. See Table O4.
optic c. A canal leading from the middle cranial fossa to the apex of the orbit in the small wing of the sphenoid bone through which pass the optic nerve and the ophthalmic artery. Syn. optic foramen.
See Table O4.
c. of Petit A space between the posterior fibres of the zonule of Zinn and the anterior surface of the vitreous humour (Fig. C1).
Schlemm’s c. A circular venous sinus located in the corneoscleral junction, anterior to the scleral spur and receiving aqueous humour from the anterior chamber and discharging into the aqueous and the anterior ciliary veins (Fig. C1). Syn. scleral sinus; sinus circularis iridis; sinus venosus sclerae; venous circle of Leber.
See meshwork, trabecular; scleral spur; vein, aqueous.
Stilling’s c. See canal, hyaloid.
canaliculi See lacrimal apparatus.
canaliculitis Inflammation of a lacrimal canaliculus, most frequently the lower one. The patient presents with a red, irritated eye with ‘pouting’ of the punctum and a slight discharge, which can be expressed by compressing the canaliculus.
candela The candela is the luminous intensity in a given direction of a source emitting monochromatic radiation of frequency 540 × 1012 Hz and the radiant intensity of which in that direction is 1/683 watt per steradian. The candela so defined is the base unit applying to photopic quantities. Symbol: cd.
candela per square metre SI unit of luminance. Syn. nit. Symbol: cd/m2.
candelpower Designates a luminous intensity expressed in candelas.
canthal tendon See ligament, palpebral.
canthus The angle formed by the upper and lower eyelids at the nasal (inner canthus or medial canthus) or temporal (outer canthus or external angle) end. Plural: canthi. Syn. palpebral angle.
See caruncle, lacrimal; conjunctivitis, angular; epicanthus.
capsular fixation Process of inserting an intraocular lens implant into the capsular bag following cataract extraction.
See capsulectomy; phacoemulsification.
capsule, Bonnet’s See Tenon’s capsule.
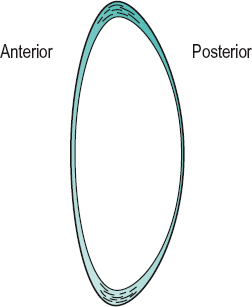
capsule, crystalline lens Transparent elastic capsule covering the crystalline lens. It is made up of collagen fibrils embedded in a glycosaminoglycan matrix. The thickness of the capsule varies; the anterior portion is thicker than the posterior and it is also thicker towards the periphery (or equator). This variation in thickness plays a role in moulding the lens substance, contributing to an increase in the curvature of the front surface, in particular, during accommodation. The capsule increases in thickness with age, and its modulus of elasticity decreases with age, which (besides flattening of the lens, and a hardening of the lens substance) contributes to presbyopia (Fig. C2). Under electron microscopy the capsule appears to have a lamellar structure that disappears with age. The capsule receives the insertion of the zonular fibres.
See fibres, lens; modulus of elasticity; shagreen of the crystalline lens; theory, Fincham’s; Zinn, zonule of.
capsule, Tenon’s See Tenon’s capsule.
capsulectomy The surgical removal of the capsule of the crystalline lens. In extracapsular cataract extraction only the anterior portion of the capsule is removed.
See capsulorhexis; capsulotomy.
capsulorhexis A form of capsulotomy in which the incision of the anterior capsule is made in a smooth circular pattern along the periphery of the lens to enable removal of opaque lens material during extracapsular cataract extraction. It is the preferred method of capsulotomy when inserting a rigid intraocular lens because the incision is less likely to tear than that made by the ‘can-opener’ technique.
capsulotomy Incision of the capsule of the crystalline lens. Capsulotomy of the anterior capsule is performed in extracapsular cataract extraction (anterior capsulotomy) to enable removal of opaque lens material. The cuts are made with a cystotome along the periphery of the lens in a circular, jagged configuration (called ‘can-opener’ capsulotomy). It is also performed on the posterior capsule (posterior capsulotomy) when it has become opaque following extracapsular extraction (manual or phacoemulsification) in order to regain the loss of visual acuity. The most common instrument used in this operation is the neodymium-yag laser.
See after-cataract; capsule, crystalline lens; capsulorhexis; cataract extraction, extracapsular.
carbachol See parasympathomimetic drug.
carbomer See tears, artificial.
carbon dioxide See hypercapnia.
carbonic anhydrase inhibitors Drugs which inhibit the carbonic anhydrase enzyme in the ciliary epithelium of the ciliary body. This enzyme is essential for the formation of aqueous humour; its reduction results in a decrease in intraocular pressure. Those in use are sulfonamide derivatives. They are administered systemically (e.g. acetazolamide) or topically in the treatment of glaucoma. Examples: acetazolamide, brinzolamide, dichlorphenamide, dorzolamide.
carboxymethylcellulose See tears, artificial.
carcinoma A malignant tumour of the epithelium, the tissue that lines the skin and internal organs of the body. It tends to invade surrounding tissues and to metastasize to distant regions of the body via the lymphatic vessels or the blood vessels. It is a form of cancer. Example: carcinoma of the skin.
See epithelioma; keratosis, seborrhoeic.
basal cell c. (BCC) A slow growing tumour derived from the basal cells of the epidermis of the skin. It is mainly located on the head and neck and most commonly on the eyelids, especially the lower eyelid. Old people who have had extensive sun exposure are primarily affected. It appears, initially, as a raised nodule with a pearly surface with small, dilated blood vessels on its surface and it may eventually become ulcerated (rodent ulcer) and invade other tissues but rarely metastasizes. Treatment includes surgical excision or cryotherapy.
sebaceous gland c. A malignant tumour arising from the meibomian glands or occasionally from the glands of Zeis. It frequently affects the upper eyelids of old people. Initially the tumour resembles a chalazion or a chronic blepharitis. However, this tumour is aggressive and may invade the orbit. It may metastasize. Treatment usually consists of thorough surgical excision.
See blepharitis; chalazion.
squamous cell c. A malignant skin cancer that affects the eyelids and conjunctiva. It is aggressive and may metastasize. It occurs most commonly in old people who have had extensive sun exposure. Treatment consists mainly of surgical excision.
Cardiff acuity test See test, Cardiff acuity.
cardinal planes; points See under the nouns.
cardinal positions of gaze See positions of gaze, cardinal.
cardinal rotation A rotation of the eye from the primary position to a secondary position about either the x-axis or the z-axis.
See axis, transverse; axis, vertical; position, primary; position, secondary.
carmellose See tears, artificial.
carrier See lens, lenticular.
carteolol hydrochloride See sympatholytic drugs.
caruncle, lacrimal A small pink fleshy structure situated in the inner canthus.
case-control study See study, case-control.
case history See history, case.
Cassegrain telescope See telescope.
cast See impression, eye.
cat’s eye syndrome See syndrome, cat’s eye.
catadioptric system See system, catadioptric.
cataphoria See kataphoria.
cataract Partial or complete loss of transparency of the crystalline lens substance or its capsule. Cataract may occur as a result of age, trauma, systemic diseases (e.g. diabetes), ocular diseases (e.g. anterior uveitis), high myopia, long-term steroid therapy, excessive exposure to infrared and ultraviolet light, heredity, maternal infections, Down’s syndrome, etc. The incidence of cataract increases with age, amounting to more than 50% in the population over 82 years. It is also more prevalent in Africa, Asia and South America than in Europe and North America. The main symptom is a gradual loss of vision, often described as ‘misty’. Some patients may also notice transient monocular diplopia, others fixed spots (not floaters) in the visual field and others better vision in dim illumination. Cataracts can easily be seen with the retinoscope, the ophthalmoscope and especially with the slit-lamp, although depending on the type, one instrument may be better than the other. At present the main treatment is surgical. Extraction is performed for one of three reasons: visual improvement, medical or cosmetic.
See after-cataract; arthritis, juvenile idiopathic; biometry of the eye; capsule, crystalline lens; disease, Wilson’s; entoptoscope, blue field; glare tester; hyperacuity; lens, crystalline; lens, intraocular; leukocoria; maxwellian view system, clinical; myopia, lenticular; phacoemulsification; syndrome, Down’s; vitreous, persistent hyperplastic primary.
age-related c. Cataract affecting older persons. It is the most common type of cataract and may take several forms: cortical, cuneiform, nuclear, mature or subcapsular. Syn. senile cataract.
anterior capsular c. A small central opacity located on the anterior lens capsule, either of congenital origin or due to a perforating ulcer of the cornea.
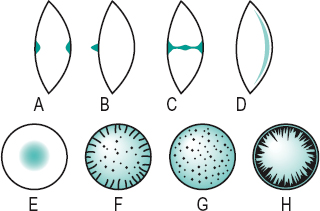
axial c. An opacity situated along the anteroposterior axis of the crystalline lens (Fig. C3).
bipolar c. An opacity involving both the anterior and the posterior poles of the lens (Fig. C3).
blue c. See cataract, blue-dot.
blue-dot c. A developmental anomaly of the crystalline lens characterized by numerous small opacities in the outer nucleus and cortex, which appear as translucent bluish dots. The condition is very common and does not usually affect acuity. Syn. blue cataract; diffuse cataract; punctate cataract.
brown; brunescent c. See cataract, nuclear.
capsular c. An opacity confined only to the capsule of the crystalline lens, anteriorly or posteriorly. It is usually congenital, although it may be acquired as a result of trauma or inflammation.
central c. See cataract, nuclear.
chalky c. A cataract characterized by the presence of lime salt deposits.
Christmas tree c. A rare type of diffuse age-related cataract in which the opacities appear as highly reflective crystals.
complicated c. A cataract caused by or accompanying another intraocular disease, such as glaucoma, cyclitis, anterior uveitis or a hereditary retinal disorder such as retinitis pigmentosa or Leber’s disease. Syn. secondary cataract.
See cataract, cuneiform; Leber’s hereditary optic atrophy; retinitis pigmentosa; syndrome, Down’s; syndrome, Fuchs’; syndrome, rubella.
congenital c. Cataract occurring as a result of faults in the early development of the lens. Some may be hereditary, usually autosomal dominant. The cause of others may be chromosomal abnormalities (e.g. Down’s syndrome, Turner’s syndrome), carbohydrate metabolic disorders (galactosaemia, galactokinase deficiency), rubella syndrome, etc. The condition requires urgent treatment to prevent the development of amblyopia.
See cataract, capsular; cataract, lamellar; cataract, nuclear; cataract, polar; cataract, sutural.
coronary c. A cataract characterized by a series of opacities having the shape of a crown or ring near the periphery of the lens (Fig. C3).
cortical c. Cataract affecting the cortex of the lens. The opacities often begin as spokes or isolated dots or clusters forming the cuneiform or subcapsular types of cataract, but eventually the opacity spreads through the entire cortex.
cuneiform c. Age-related cataract characterized by opacities distributed within the periphery of the cortex of the lens in a radial manner, like spokes on a wheel (Fig. C3).
See cataract, subcapsular.
cupuliform c. See cataract, sub-capsular.
diabetic c. Cataract associated with diabetes. In old eyes this type is similar to that of a non-diabetic person but in young eyes it is typically of the snowflake type.
diffuse c. See cataract, blue-dot; cataract, Christmas tree.
electric c. An opacity caused by an electric shock.
c. extraction, extracapsular (ECCE) Surgical procedure for the removal of a cataractous crystalline lens. The anterior capsule is excised, the lens nucleus is removed and the residual equatorial cortex is aspirated. The posterior capsule may be polished. An intraocular lens implant may then be inserted.
See after-cataract; biometry of the eye; capsulectomy; lens, intraocular; pearls, Elschnig’s; phacoemulsification; ring, Soemmering’s.
c. extraction, intracapsular (ICCE) Surgical procedure for the removal of a cataractous crystalline lens. The entire lens, together with its capsule, is removed. This procedure is rarely performed nowadays.
See ligament of Wieger.
fluid c. Hypermature cataract in which the lens substance has degenerated into milky fluid.
glassblower’s c. See cataract, heat-ray.
heat-ray c. Cataract due to excessive exposure to heat and infrared radiation. Syn. glassblower’s cataract; thermal cataract.
See exfoliation of the lens; infrared.
hypermature c. The last stage in the development of age-related cataract in which the lens substance has disintegrated.
See cataract, incipient; cataract, intumescent cortical; cataract, mature; glaucoma, phacolytic.
incipient c. The first stage in the development of age-related cataract characterized by streaks similar to the spokes of a wheel or with an increased density of the nucleus.
See cataract, intumescent cortical; cataract, mature; lens, crystalline; sight, second.
intumescent cortical c. A stage of development of a cataract in which the lens, especially the cortex, absorbs fluid and swells. It may lead to secondary angle-closure glaucoma. The cataract can progress to the hypermature stage in which case the fluid leaks out, resulting in shrinkage of the lens and wrinkling of the anterior capsule, leaving the harder nucleus free within the capsule.
See cataract, morgagnian.
lamellar c. A congenital cataract affecting one layer of the crystalline lens only. Syn. zonular cataract.
mature c. The middle stage in the development of age-related cataract characterized by a completely opaque lens and considerable loss of vision.
See cataract, hypermature; cataract, incipient.
morgagnian c. A hypermature age-related cataract in which the cortex has shrunk and liquefied and the nucleus floats within the lens capsule. Degraded lens proteins may leak into the aqueous humour and cause phacolytic glaucoma. Syn. cystic cataract; sedimentary cataract.
See cataract, intumescent cortical.
nuclear c. An opacity affecting the lens nucleus. It can be either congenital or age-related in origin. It frequently leads to an increase in myopia (or decrease in hyperopia). In some cases it reaches such a brown colour that it is called brunescent cataract (or brown cataract). Syn. central cataract (Fig. C3).
polar c. A congenital opacity found at either pole of the crystalline lens. Anterior polar cataract may be flat or project as a conical opacity (pyramidal cataract) into the anterior chamber (Fig. C3). Posterior types may be associated with persistent hyaloid remnant (Mittendorf’s dot).
punctate c. See cataract, blue-dot.
pyramidal c. See cataract, polar.
senile c. See cataract, age-related.
secondary c. 1. Syn. for complicated cataract. 2. Syn. for after-cataract.
snowflake c. A cataract characterized by greyish or whitish flakelike opacities. It is usually found in young diabetics or severe cases of diabetes (Fig. C3).
soft c. Cataract in which the lens nucleus is soft.
See lens, crystalline.
subcapsular c. An age-related opacity located beneath the anterior or posterior capsule. It may spread from the periphery of the cortex like spokes on a wheel (cuneiform cataract). This is the most common type of cortical cataract. The opacities may also be confined to the posterior layers of the cortex with a granular or lace-like appearance (cupuliform cataract). Subcapsular cataracts are often the result of radiation exposure, age, toxic damage (e.g. from corticosteroids), or secondary to eye diseases (e.g. uveitis, retinitis pigmentosa). (Fig. C3).
sunflower c. See chalcosis lentis.
c. surgery See capsulectomy; capsulorhexis; capsulotomy; cataract extraction, extracapsular; cataract extraction, intracapsular; phacoemulsification.
sutural c. A congenital cataract in which the opacities are found along the anterior and/or posterior lens sutures. The opacities may appear Y-shaped or flower-shaped. The condition is often associated with Fabry’s disease.
thermal c. See cataract, heat-ray.
traumatic c. Cataract following injury to the lens, its capsule, or to the eyeball itself. It is commonly unilateral. Penetrating trauma of the lens causes rapid opacification of the cortex or even most of the lens contents. Concussion of the lens may result in capsular, subcapsular or cortical opacities.
See ring, Vossius’.
zonular c. See cataract, lamellar.
catoptric image See image, catoptric.
catoptrics The branch of optics which deals with reflection and reflectors.
caustic The concentration of light in the caustic surface of a bundle of converging light rays which represents the focal image in an optical system uncorrected for spherical aberration. It appears as a hollow luminous cusp with its apex at the paraxial focus.
cavernous haemangioma; plexus; sinus See under the nouns.
cecocentral See centrocecal.
ceftazidime See antibiotic.
ceftriaxone See antibiotic.
cefuroxime See antibiotic.
cell 1. In biology, the basic, structural and functional units from which living organisms and tissues are built. A cell consists of a nucleus surrounded by all the cellular contents (cytoplasm) including various organelles (mitochondria, Golgi apparatus, lysosomes, ribosomes, etc.) and inclusions (glycogen, melanin, triglycerides, etc.) suspended in intracellular fluid (water, proteins, carbohydrates, lipids, inorganic and organic substances) all enclosed in a plasma membrane. There are many types of cells (blood cells, connective tissue cells, epithelial cells, muscle cells, nerve cells, secretory cells, etc.). Living cells are capable of reproduction (for body growth, wound healing, etc.) by mitotic activity. 2. In optics, a rim in a trial frame or in an optical instrument into which a lens can be placed.
A c. See cell, M.
acinar c. A type of cell found within the body of the lacrimal gland. This cell lines the lumens of glands in a lobular pattern and produces a serous secretion.
amacrine c. Retinal cell located in the inner nuclear layer connecting ganglion cells with bipolar cells. Some have an ascending axon synapsing with receptors.
B c. See cell, P.
basal c. See corneal epithelium.
binocular c. A cell in the visual cortex that responds to stimulation from both eyes. It may, however, show an ocular dominance for either eye. It responds more strongly when corresponding regions of each eye are stimulated by targets of similar size and orientation.
See column, cortical; hypercolumn.
bipolar c. Retinal cell located in the inner nuclear layer connecting the photoreceptors with amacrine and ganglion cells.
C c. A retinal ganglion cell with slow axonal conduction which sends information to the superior colliculus and to the centre involved in the control of pupillary diameter, rather than to the lateral geniculate body. There are very few such cells. Syn. Pγ cell; W cell (thus called in the cat).
Cajal’s c. See astrocytes.
clump c. Large, pigmented round cells found in the pupillary zone of the iris stroma. They are considered to be macrophages containing mainly melanin granules. The number of these cells increases with age.
colour-opponent c’s. Cells which respond by increasing response to light of some wavelengths and decreasing their response to others (usually complementary). If the light stimulus contains both sets of wavelengths the two responses tend to cancel each other. Two types of cells have been identified: red-green cells and blue-yellow cells. These cells are found mainly in the lateral geniculate bodies but also among retinal ganglion cells, and they form the blobs in the visual cortex. The responses of these cells support Hering’s theory of colour vision. Syn. opponent-process cell (although this term also includes a cell that increases its response to white light and decreases its response to dark).
See blobs; theory, Hering’s of colour vision.
complex c. A cell in the visual cortex whose receptive field consists of a large responsive area, approximately rectangular in shape, surrounded by an inhibitory region. The stimulus, which is usually a slit or a straight line, gives an optimum response if appropriately orientated but falling anywhere within the excitatory area. These cells tend to respond optimally to the movement of a specifically orientated slit. Many complex cells also respond better when the optimally orientated slit is moved in one direction rather than in the opposite direction. In general, complex cells show non-linear spatial summation properties.
See area, visual; cell, hypercomplex; cell, simple; field, receptive; summation.
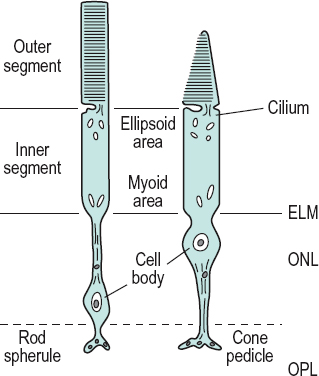
cone c. Photoreceptor of the retina which connects with a bipolar cell and is involved in colour vision and high visual acuity and which functions in photopic vision. The outer segment of the cell is conical in shape, except in the fovea centralis where it is rodlike. In the outer segment (i.e. the part closest to the pigment epithelium) are contained hollow discs (or lamellae), the membranes of which are joined together and are also continuous with the boundary membrane of the cone cell. The visual pigments are contained in these discs. There are three types of cones, each containing a different pigment sensitive to a different part of the light spectrum. They are referred to as long-wave-sensitive (or L-cones), medium-wave-sensitive (or M-cones) and short-wave-sensitive (or S-cones). There are about six million cones in the retina, with the greatest concentration in the macular area (Fig. C4).
See cone pedicle; effect, Stiles–Crawford; ellipsoid; foveola; macula; pigment, visual; theory, duplicity; vision, photopic.
fixed c. See corneal corpuscle.
ganglion c. 1. Retinal cell that connects the bipolars and other cells in the inner plexiform layer with the lateral geniculate body. The axons of the ganglion cells constitute the optic nerve fibres. There are many types of ganglion cells. The two major types are: the magno (M or parasol) ganglion cells which project mainly to the magnocellular layers of the lateral geniculate bodies; and the parvo (P) ganglion cells which project to the parvocellular layers of the lateral geniculate bodies. Two types of P ganglion cells are noted: P1, which are midget cells and have small dendritic fields and P2, which have large dendritic fields. M and P cells comprise about 10% and 82% of the ganglion cells respectively. 2. One of a collection of nerve cell bodies found in a ganglion.
See cell, C; cell, M; cell, P; melanopsin.
glial c’s. Cells found throughout the nervous system. They provide support and nutrition for neurons, as well as being involved in the operation of the brain, especially the fluid surrounding the neurons and their synapses. They are also believed to be involved in the reuptake of neurotransmitters from within the synaptic cleft. There are three types of glial cells: astrocytes; microglia; oligodendroglia. Syn. glia; neuroglia.
goblet c. Cell of the conjunctival epithelium which secretes mucin.
See glands of Henle; mucin; xerophthalmia.
horizontal c. Retinal cell located in the inner nuclear layer which connects several cones and rods together.
hypercomplex c. A cell in the visual cortex that receives inputs from several simple and complex cells and therefore has an even more elaborate receptive field than a complex cell. It is most effectively stimulated by a stimulus of a specific size and of a specific orientation and which is moved in a specific direction.
See cell, complex; cell, simple.
Langerhans’ c’s. Dendritic cells located mainly in the epidermis, mucous membranes and lymph nodes. They have surface receptors for immunoglobulin (Fc), complement (C3) and surface HLA–DR (la) antigen. Langerhans’ cells are also found in the conjunctival epithelium and among the basal cells, mainly of the peripheral corneal epithelium. They have antigenic functions, stimulate T-lymphocytes, prostaglandin production and participate in cutaneous delayed hypersensitivity and corneal graft rejection. Extended wear of contact lenses tends to induce an increase of these cells. They are also found in histiocytic tumours.
Table C1
Main distinguishing features of the two principal types of ganglion cells of the retina
| properties | P cell (X cell) | M cell (Y cell) |
| size of cell body | small | large |
| dendritic spread | small | medium/large |
| receptive field size | small | medium/large |
| retinal distribution | 90% of these at the macula | 5% of these at the macula; about 13% overall |
| projection | LGN parvocellular layers | LGN magnocellular layers |
| type of response | sustained | transient |
| light sensitivity | low | high |
| wavelength response | selective (except P cells) | non-selective |
| spatial sensitivity | fine target detail | large target detail |
| temporal sensitivity | low target velocity | high target velocity |
M c. A retinal ganglion cell, mainly located in the periphery of the retina and which assists in movement perception. M cells tend to give transient responses to stimuli and to have non-linear spatial summation properties. This cell transmits information principally to the magno cells of the lateral geniculate bodies. Syn. A cell; Pαcell; Y cell (thus called in the cat).
magno c. See cell, ganglion; geniculate bodies, lateral.
Mueller’s c. Neuroglial cell in the retina with its nucleus in the inner nuclear layer and with fibres extending from the external to the internal limiting membrane. These cells support the neurons of the retina and possibly assist in their metabolism. Syn. Müller cell.
orientation-specific c. A cell that responds best to specifically orientated lines. This is the case for almost all cells in the visual cortex. Examples: complex cell; simple cell.
See cell, complex; cell, simple; field, receptive.
P c. A retinal ganglion cell, mainly located in the central region of the retina and which assists in high acuity and colour vision. P cells tend to give sustained responses to stimuli and to have linear spatial summation properties. This is the most common type of ganglion cells (about 82%). This cell transmits information principally to the parvo cells of the lateral geniculate bodies. Syn. B cell; Pβcell; X cell (thus called in the cat).
parasol c. See cell, ganglion.
parvo c. See cell, ganglion; geniculate bodies, lateral.
rod c. Photoreceptor cell of the retina which connects with a bipolar cell. It contains rhodopsin and is involved in scotopic vision. The molecules of rhodopsin are contained in about 1000 hollow discs (double lamellae or membranes), which are isolated from each other and from the boundary membrane of the rod cell. These discs are found in the outer segment (i.e. the part closest to the pigment epithelium) of the cell. There are about 100 million rod cells throughout the retina; only a small area, the foveola, is free of rods (Fig. C4).
See eccentricity; ellipsoid; foveola; rhodopsin; rod spherule; theory, duplicity; vision, scotopic.
Schwann c. A cell whose membrane spirals around the axon with layers of myelin in between each coil, as well as being a source of the myelin sheath. The cell provides insulation to the axon. It covers about one millimetre, so that hundreds may be needed to completely cover an axon. It also allows for an increase in the speed of the nervous impulse without an increase in axonal diameter. The gaps between the segments covered by the cells are called nodes of Ranvier.
simple c. A cell in the visual cortex whose receptive field consists of an excitatory and an inhibitory area separated by a straight line, or by a long narrow strip of one response flanked on both sides by larger regions of the opposite response. Responses occur only to a straight line or a narrow strip orientated approximately parallel to the boundary/ies between the two areas. In general, simple cells show linear spatial summation properties. They are presumably the first cells where the nervous impulses are processed as they enter the visual cortex.
See area, visual; cell, complex; field, receptive.
squamous c. See corneal epithelium.
W c. See cell, C.
wing c. See corneal epithelium.
X c. See cell, P.
Y c. See cell, M.
cellulose acetate butyrate See CAB.
cellulitis, preseptal Swelling or infection of the eyelid tissue in front of the orbital septum. There is redness, swelling and tenderness of the eyelid. The condition is treated with systemic antibiotics.
cellulitis, orbital Infection of the orbital contents caused by Staphylococcus aureus, Streptococcus or Haemophilus influenzae. It is often caused by the spread of infection from adjacent structures, especially the sinuses. The clinical signs are fever, pain, proptosis, redness, swelling of the lid and orbital tissue and restricted eye movements which may occasionally lead to diplopia and, as the condition worsens, visual acuity decreases. Initial management consists of parenteral antibiotics but surgery may become necessary.
See lamina papyracea.
central corneal optical zone See optical zone of cornea.
central fusion See fusion, sensory.
central retinal artery; vein See under the nouns.
central retinal artery occlusion See retinal arterial occlusion.
central retinal vein occlusion See retinal vein occlusion.
central serous retinopathy; vision; visual acuity
See under the nouns.
centration distance; near distance; point See under the nouns.
centre, boxing The point midway between the two horizontal and the two vertical sides of the rectangle enclosing the lens, in the boxing system. Syn. geometric centre of a cut lens.
centre, optical That point (real or virtual) on the optical axis of a lens which is, or appears to be, traversed by rays emerging parallel to their original direction. Applied to an ophthalmic lens, it is commonly regarded as coinciding with the vertex of either surface (British Standard).
centre of rotation of the eye When the eye rotates in its orbit, there is a point within the eyeball that is more or less fixed relative to the orbit. This is the centre of rotation of the eye. In reality, the centre of rotation is constantly shifting but by a small amount. It is considered, for convenience, that the centre of rotation of an emmetropic eye lies on the line of sight of the eye 13.5 mm behind the anterior pole of the cornea when the eye is in the straight ahead position (straightforward position), that is when the line of sight is perpendicular to both the base line and the frontal plane.
See axis, anteroposterior; line of sight.
centre, standard optical position A reference point specific to each spectacle lens shape. The standard optical position is on the vertical line passing through the boxed centre, and is at the boxed centre.
See centre, boxing; system, boxing.
centre, visual Centre of the brain concerned with vision.
See area, visual; fissure, calcarine.
centrocecal An area of the retina which includes the macula, the optic disc and the area in between. Note: also spelt centrocaecal. Syn. cecocentral.
cephalosporin See antibiotic.
cerium oxide A pink powder derived from the metallic element cerium. It is used to polish lenses and it is also added to ophthalmic glass to absorb ultraviolet radiations.
See polishing.
cetirizine See antihistamine.
cetrimide See antiseptic.
chalazion A chronic inflammatory lipogranuloma due to retention of the secretion (such as blocked ducts) of a meibomian gland in the tarsus of an eyelid. It is characterized by a gradual painless swelling of the gland without marked inflammatory signs and sometimes astigmatism which is induced by the cyst pressing on the cornea (Fig. C5). Small chalazia may disappear spontaneously but large ones usually have to be incised and curetted (i.e. removal of the pus with a scraper) through a tarsal incision. Resolution may also occur after local injection of a corticosteroid drug (e.g. dexamethasone or triamcinolone). Syn. meibomian cyst (although it is not a true cyst because its walls are made of granulomatous tissue and not lined with epithelium).
chalcosis lentis A cataract caused by excessive amount of copper in the eye. It appears as small yellowish-brown opacities in the subcapsular cortex of the lens and pupillary zone with petal-like spokes that extend towards the equator. It may be due to an intraocular foreign body containing copper, or from eyedrops that contain copper sulfate, or as part of Wilson’s disease. Management consists mainly of removal of the foreign body. Syn. sunflower cataract.

chamber In anatomy, a small cavity.
anterior c. (AC) Space within the eye filled with aqueous humour and bounded anteriorly by the cornea and posteriorly by the iris and the part of the anterior surface of the lens which appears through the pupil. Its average axial length is 3.2 mm.
See angle of the anterior chamber; flare, aqueous; gonioscope; method, van Herick, Shaffer and Schwartz; method, Smith’s; optics of the eye; test, shadow.
c’s. of the eye The anterior, posterior and vitreous chambers of the eye.
posterior c. Space within the eye filled with aqueous humour and bounded by the posterior surface of the iris, the ciliary processes, the zonule and the anterior surface of the lens.
vitreous c. Space within the eye filled with vitreous humour and bounded by the retina, ciliary body, canal of Petit and the postlenticular space of Berger.
Chandler’s syndrome See syndrome, Chandler’s.
channel A concept relating to the evidence that information about a particular feature of an image is transmitted and processed in the visual pathway approximately independently of information about other domains. The evidence was obtained from various experiments: matching, threshold elevation, after-effect, etc. Examples: the three channels of colour vision theory; the spatial frequency channels.
See after-effect, waterfall.
chaos, light See light, idioretinal.
Charles Bonnet syndrome See syndrome, Charles Bonnet.
chart 1. A tabular presentation of test targets for assessing vision. 2. A recording of clinical data relating to a patient’s case.
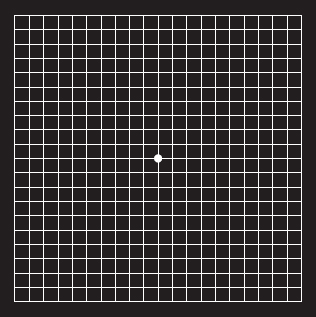
Amsler c. One of a set of charts used to detect abnormalities in the central visual field which are so slight that they are undetected by the usual methods of perimetry. There are various patterns, each on a different chart, 10 cm square. One commonly used chart consists of a white grid of 5 mm squares on a black background. Each pattern has a dot in the centre, which the patient fixates. When fixated at a distance of 30 cm the entire chart subtends an angle of 20°. If there is any visual impairment (usually as a result of macular disease) it is demonstrated by the absence or irregularities of the lines (Fig. C6). Syn. Amsler grid.
See macular degeneration, age-related; metamorphopsia.
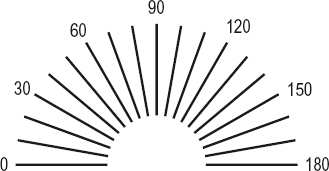
astigmatic fan c. A test pattern consisting of a semicircle of radiating black lines on a white background for determining the presence and the amount, as well as the axis of ocular astigmatism. If the chart resembles the ‘clock face’ type it is called an astigmatic dial or clock dial chart (Fig. C7).
Bailey–Lovie c. A visual acuity chart with letter sizes ranging from 6/60 (20/200) to 6/3 (20/10) in 14 rows of 5 letters. Each row has letters which are approximately 4/5 the size of the next larger letters and the letters in each row have approximately the same legibility (within ±10%). It is most useful with low vision patients. This is the most commonly used type of log MAR charts (Fig. C8). There is also a Bailey–Lovie Word Reading Chart for near vision. It is composed of words rather than letters. The size progression of each line is logarithmic. The typeface used is the lower case Times Roman customarily used in newspapers and books, and the range of sizes varies between 80-point and 2-point print (or the Snellen equivalent at 40 cm of 6/144 or 20/480 to 6/3.6 or 20/12, respectively). There are 20 such charts, each with a different set of words.
See acuity, near visual.
clock dial c. See chart, astigmatic fan.
contrast sensitivity c. A chart designed to test contrast sensitivity. Such a test is useful with patients having low vision and in the early detection of diseases. Examples: Pelli–Robson chart; reduced contrast Bailey–Lovie near log MAR letter chart.
See acuity cards, Teller; test, Arden grating; Vistech.
illiterate E c. Chart for carrying out a subjective visual acuity test on a person who cannot read. It consists of a graduated series of the Snellen letter E orientated in various directions which the subject must recognize. This procedure is sometimes called the ‘E’ test or ‘E’ game.
See acuity cards, Teller; ‘E’ game; test, Cardiff acuity.
Landolt broken ring c. A visual acuity chart using a graduated series of Landolt rings in which the target thicknesses and gaps are equal to one-fifth of the outer diameter. The subject must indicate the orientation of the gap, which usually appears in one of four directions: right, left, up or down. This test is less subjective than the Snellen chart. Syn. Landolt C chart.
log MAR c. A visual acuity chart in which the rows of optotypes vary in a logarithmic progression. The multiplier of the geometric progression is usually equal to 1.2589 or 0.1 log unit. On one side of such a chart the rows of optotypes are usually labelled with the traditional Snellen notation. On the other side of each row visual acuity is labelled as the logarithm of the minimum angle of resolution (log MAR), which is the logarithm to the base 10 of the angular subtense of the stroke widths of the optotypes at a standard distance.
See chart, Bailey–Lovie; Glasgow acuity cards.
Pelli–Robson c. A contrast sensitivity chart consisting of eight lines of letters, all of the same size, subtending 3 degrees at a viewing distance of 1 m. On each line there are two groups, each containing three different letters; the letters in each group have the same contrast. The contrast of the different letters in each group decreases by a factor of 1/2 and the range of contrast varies between 100 and 0.6% in 16 steps. The subject is asked to read the letters starting with those of high contrast and continuing until two or three letters in one group are incorrectly named. The contrast threshold is represented by that of the previous group of letters. The chart gives the results in log contrast sensitivity. This test provides a measurement of contrast sensitivity at low to intermediate spatial frequencies depending upon the viewing distance. Syn. Pelli–Robson contrast sensitivity test.
Raubitschek c. A test target for determining the axis and the amount of astigmatism of the eye. It consists of two parabolic lines (known as wings) in an arrowhead pattern, parallel and closely spaced at one end, and each diverging from each other through a 90° angle at the other end. There are several methods of using this test. Syn. Raubitschek arrows; Raubitschek dial.
reduced contrast Bailey–Lovie near log MAR letter c. A set of 30 Bailey–Lovie charts designed to measure contrast sensitivity. Each chart has a different contrast, half of the charts contains the letters of the distance Bailey–Lovie chart and the other half contains the letters of the near Bailey–Lovie chart. All the charts have the same average reflectance and the contrast of the charts ranges from 0.95 to 0.0013%. The charts are presented to the subject in order of increasing contrast and the subject reads the letters from the largest to the smallest lines that they are able to. Threshold resolution in log min arc is determined for each of the 30 charts and a contrast sensitivity curve can thus be determined.
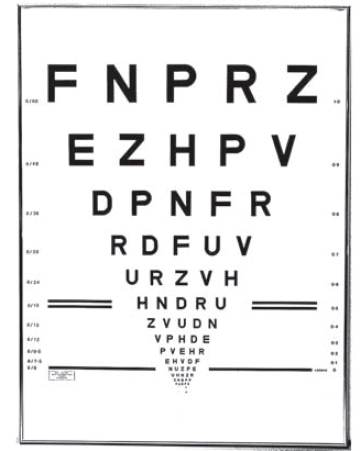
Snellen c. A visual acuity test using a graduated series of Snellen letters (or Snellen test types), in which the limbs and the spaces between them subtend an angle of one minute of arc at a specified distance. The letters are usually constructed so that they are 5 units high and 4 units wide, although some charts use letters that fit within a square subtending 5 minutes of arc at that distance.
See acuity, Snellen; Snellen fraction.
Table C2
Relationship between the Snellen fraction and the log MAR notation for distance visual acuity
| Snellen fraction | log MAR | |
| (m) | (ft) | |
| 6/150 | 20/500 | 1.4 |
| 6/120 | 20/400 | 1.3 |
| 6/95 | 20/320 | 1.2 |
| 6/75 | 20/250 | 1.1 |
| 6/60 | 20/200 | 1.0 |
| 6/48 | 20/160 | 0.9 |
| 6/38 | 20/125 | 0.8 |
| 6/30 | 20/100 | 0.7 |
| 6/24 | 20/80 | 0.6 |
| 6/19 | 20/63 | 0.5 |
| 6/15 | 20/50 | 0.4 |
| 6/12 | 20/40 | 0.3 |
| 6/9.5 | 20/32 | 0.2 |
| 6/7.5 | 20/25 | 0.1 |
| 6/6 | 20/20 | 0 |
| 6/4.75 | 20/16 | –0.1 |
| 6/3.75 | 20/12.5 | –0.2 |
| 6/3 | 20/10 | –0.3 |
test c. A board externally illuminated, an internally illuminated transparent sheet, a slide for projection or a computer based system which projects optotypes or other tests used in the subjective determination of refraction. Syn. letter chart.
See legibility; optotype.
Chavasse lens See lens, Chavasse.
check ligament See ligament, check.
checkerboard pattern See pattern, checkerboard.
cheiroscope An instrument used in the management of amblyopia, suppression and hand and eye coordination. It consists of presenting a line drawing to one eye (usually the dominant one), which is traced by a pencil or crayon in the field of view of the other eye. The two fields of view are separated by a septum and a small mirror is used to reflect the line drawing. Stereoscopes can easily be adapted into cheiroscopes.
chemical burn An injury caused, usually, by alkali (e.g. ammonia, caustic potash, lime, sodium hydroxide) or acid (e.g. hydrochloric, sulphuric). The type and severity of the injury depends on the properties of the chemical and upon which ocular tissue is involved. However, alkali burns are more severe than acid burns because they penetrate the tissues more rapidly and more deeply. In all cases, immediate copious irrigation is crucial, followed by a topical anaesthetic to relieve pain. Irrigation is continued until repeated measurements of ocular pH reach and retain a normal value. Treatment includes cycloplegics, antibiotics, steroids, ascorbate (only in alkali burns) to restore collagen synthesis, and glaucoma medication may be needed to prevent an increase of intraocular pressure. In some cases, surgery may also be required.
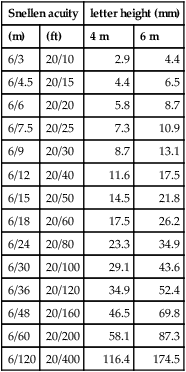
Table C3
Relationship between Snellen visual acuity and letter height at two viewing distances (the letter corresponding to an acuity of 6/6 subtends 5’ and the gap in the letter 1’)
| Snellen acuity | letter height (mm) | ||
| (m) | (ft) | 4 m | 6 m |
| 6/3 | 20/10 | 2.9 | 4.4 |
| 6/4.5 | 20/15 | 4.4 | 6.5 |
| 6/6 | 20/20 | 5.8 | 8.7 |
| 6/7.5 | 20/25 | 7.3 | 10.9 |
| 6/9 | 20/30 | 8.7 | 13.1 |
| 6/12 | 20/40 | 11.6 | 17.5 |
| 6/15 | 20/50 | 14.5 | 21.8 |
| 6/18 | 20/60 | 17.5 | 26.2 |
| 6/24 | 20/80 | 23.3 | 34.9 |
| 6/30 | 20/100 | 29.1 | 43.6 |
| 6/36 | 20/120 | 34.9 | 52.4 |
| 6/48 | 20/160 | 46.5 | 69.8 |
| 6/60 | 20/200 | 58.1 | 87.3 |
| 6/120 | 20/400 | 116.4 | 174.5 |
chemodenervation A technique in which a pharmacologic compound (e.g. atropine, botulinum toxin) is used to paralyse a muscle or group of muscles. This technique is most often used in the treatment of certain forms of strabismus as well as blepharospasm.
chemosis Severe oedema of the conjunctiva.
See ophthalmopathy, thyroid.
cherry-red spot See spot, cherry-red.
Cheshire cat effect See effect, Cheshire cat.
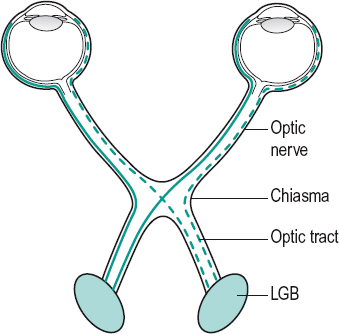
chiasma, optic A structure located above the pituitary gland and formed by the junction and partial decussation (crossing-over) of the optic nerves. The fibres from the nasal half of the retina of the left eye cross over to join the fibres from the temporal half of the right retina to make up the right optic tract and vice versa. About 53% of the axons of the optic nerves cross to the opposite tract (Fig. C9). A lesion of the chiasma produces a typical field defect (heteronymous hemianopia). Note: also spelt chiasm.
See circle of Willis; decussation; pathway, visual; stereo-blindness; tracts, optic.
chiastopic fusion See fusion, chiastopic.
Chievitz, transient layer of See layer of Chievitz, transient.
chlamydial infection See conjunctivitis, adult inclusion; keratitis, epithelial; ophthalmia neonatorum; trachoma.
chlorambucil See immunosuppressants.
chloramphenicol A broad-spectrum antibiotic effective against a wide variety of Gram-negative and Gram-positive bacteria (but not Pseudomonas aeruginosa). It is commonly used in solution 0.5% or ointment 1% to treat bacterial conjunctivitis or blepharitis.
chlorbutanol See antiseptic.
chlorhexidine See antiseptic.
chlorolabe See pigment, visual.
chlorphenamine See antihistamine.
chlorophobia An abnormal aversion to green. See chromatophobia.
chlortetracycline See antibiotic.
chloropsia See chromatopsia.
choked disc See papilloedema.
cholinergic Relates to neurons or nerve fibres in which acetylcholine (ACh) is the neurotransmitter, or have actions similar to those caused by ACh. Cholinergic receptors are of two types: nicotinic receptors, which are situated in striated muscles (e.g. the extraocular muscles) and muscarinic receptors, which are situated in parasympathetically innervated structures (e.g. the iris and ciliary body).
See acetylcholine; nicotine; parasympathomimetic drug.
choriocapillaris Layer of the choroid adjacent to Bruch’s membrane and consisting of a network of capillaries which supplies nutrients to the retina.
chorioretinitis Inflammation of the retina and the choroid. It originates in the choroid and subsequently spreads to the retina.
See nystagmus.
chorioretinopathy, central serous See retinopathy, central serous.
choroid The highly vascular tunic of the eye lying between the retina and sclera. Its main function is to nourish the retina (oxygen and nutrients) and remove waste products. It is a thin membrane extending from the optic nerve to the ora serrata. It contains blood vessels, capillaries, nerves, collagen and melanocytes, as well as fibroblasts, macrophages, mast cells and plasma cells. It consists of five main layers from without inward: the suprachoroid (lamina fusca), the layers of vessels (Haller’s layer and Sattler’s layer), the choriocapillaris and the membrane of Bruch (lamina vitrea). The blood supply is provided mostly by the short posterior ciliary arteries and to a lesser extent by the long posterior ciliary arteries, as well as some branches from anterior ciliary arteries. Venous blood drains into the vortex veins. The posterior choroid is thickest in hyperopia and thinnest in myopia. Note: some authors consider the suprachoroid as belonging to the sclera. However, when choroid and sclera are separated, part of the suprachoroid adheres to the choroid and part to the sclera.
See choroiditis; epichoroid; naevus, choroidal; neovascularization, choroidal; space, suprachoroidal.
choroidal detachment A separation of the choroid from the sclera, usually resulting from intraocular surgery, a severe contusion, hypotony, or from a vascular disease. Fluid accumulates in the suprachoroidal space. The ciliary body may be involved. Ophthalmoscopic examination reveals dark, convex, smoothly rounded elevations of both the retina and the choroid. Intraocular pressure may be very low and some visual field defects may be present. Syn. choroidal effusion.
See hypotony, ocular; syndrome, uveal effusion.
choroidal flush This is the first evidence of fluorescein dye reaching the eye during the method of fluorescein angiography. It occurs approximately 1 second before reaching the retinal circulation because the route from the ophthalmic artery to the choroidal circulation is shorter.
choroidal folds A condition characterized by lines, grooves or striae in the posterior fundus. Clinically they appear as alternating light and dark lines possibly corresponding to folds in Bruch’s membrane and the retinal pigment epithelium. They are most easily seen with fluorescein angiography. They may occur as a result of a retrobulbar tumour, choroidal tumour, posterior scleritis, ocular hypotony, in hyperopic eyes, or without any discernible cause.
See haemangioma, cavernous.
choroidal melanoma; naevus; neovascularization See under the nouns.
choroideremia A bilateral, X-linked, recessive inherited degeneration of the choroid and retinal pigment epithelium characterized by night blindness (nyctalopia) which begins in early youth. Most males are myopic. The condition is mild and non-progressive in females. Both males and females display a salt and pepper appearance of the fundus, but in males it advances to complete atrophy and eventually blindness. Syn. progressive choroidal atrophy; progressive tapetochoroidal atrophy.
See chromosome; inheritance.
choroiditis Inflammation of the choroid. The ophthalmoscopic appearance is a whitish-yellow area stippled with pigment. However, it is most often associated with an inflammation of the retina (chorioretinitis) and of the other tissues of the uvea. Vision is blurred if the lesion is in the macular area.
See iritis; uveitis, posterior.
choroiditis, Tay’s See drusen, familial dominant.
chroma See Munsell colour system.
chromatic Pertaining to colour.
chromatic aberration; adaptation; dispersion; parallax See under the nouns.
chromatic stereopsis See chromostereopsis.
chromatic vision See vision, colour.
chromaticity Colour quality of a colour stimulus definable by its chromaticity coordinates, or by its dominant (or complementary) wavelength and its purity taken together (CIE).
See saturation; wavelength, dominant.
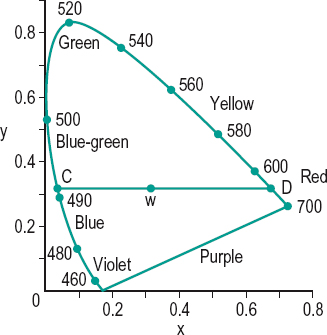
chromaticity diagram Plane diagram showing the results of mixtures of colour stimuli, each chromaticity being represented by a single point on the diagram (Fig. C10). Syn. colour triangle.
See ellipses, MacAdam; illuminants, CIE standard; light, white; purple; spectrum locus.
chromatophobia An abnormal aversion to colours or to certain colours (e.g. erythrophobia, an abnormal aversion to red). It may be psychological or physiological, such as an abnormal sensitivity to some short wavelengths following cataract extraction. Syn. chromophobia.
See chlorophobia; cyanophobia.
chromatopsia Abnormal condition in which objects appear falsely coloured. Depending upon the colour seen, the chromatopsia is called xanthopsia (yellow vision), erythropsia (red vision), chloropsia (green vision) or cyanopsia (blue vision). This condition may appear after a cataract operation (blue and red vision) or following exposure to an intense illumination (red vision) or in people suffering from carbon monoxide poisoning and oxygen deprivation. This may cause some damage to the areas of the visual cortex involved in the processing of colour perception, because these areas are supplied with more blood vessels than other areas of the visual cortex. Syn. chromopsia.
See euchromatopsia; xanthopsia.
chromophobia See chromatophobia.
chromoretinoscopy An objective method of measuring the longitudinal chromatic aberration of the eye by carrying out retinoscopy through various coloured filters (usually a red and a green filter). However, it is necessary to use a retinoscope source of high luminance (e.g. halogen). The difference in the retinoscopic value obtained with the two coloured filters represents the longitudinal chromatic aberration of the eye between these two dominant wavelengths.
chromosome One of the thread-like structures located within the cell nucleus composed of an extremely long, double-stranded DNA (deoxyribonucleic acid) helix tightly folded around proteins called histones. Each chromosome carries genes that contain the hereditary material that controls the growth and characteristics of the body. There are 46 chromosomes in each human somatic cell organized in 23 pairs, of which 22 pairs are similar in appearance but differ at the molecular level. They are called autosomal chromosomes or autosomes and are designated by a number (with chromosome 1 being the longest, followed by chromosome 2, etc.). The other pair, the sex chromosomes determines the sex of the individual. In mammals the two sex chromosomes of females are alike (homologous) and are referred to as X chromosomes. Males carry one X chromosome along with a much shorter chromosome, the Y chromosome. Each chromosome has a centromere that divides it into two arms, the short arm ‘p’ and the long arm ‘q’. Disorders of chromosome number in which the number of chromosomes is above or below the normal (46) are called aneuploidy. Common forms of aneuploidy are trisomy in which there is one extra chromosome and monosomy in which there is one less, than the normal 46. They rarely cause specific eye diseases but affected individuals present ocular manifestations. Examples: Down’s syndrome (trisomy of chromosome 21), Edwards’ syndrome (trisomy 18), Turner’s syndrome (monosomy 45 XO). There are other chromosome abnormalities such as translocation (one segment of a chromosome is transferred to another chromosome) as may occur in congenital anterior polar cataract, deletion (a loss of a piece of chromosome) as in aniridia, choroideremia, retinoblastoma, etc. Other cases involve damage of a chromosome (e.g. fragile X syndrome).
See colour vision, defective; gene; mitosis; mutation.
chromostereopsis A sensation of apparent depth among coloured objects placed at the same distance from the subject and viewed binocularly, when the pupils are eccentric to the achromatic axes or the visual axes do not coincide with the achromatic axes. This phenomenon is attributed to the retinal disparity created by the chromatic aberration of the eye. If the objects are red and blue (or green), the red appears closer than the blue (or green) in many people. Other people see the reverse impression and a few others do not see any apparent depth at all. The phenomenon can be enhanced, eliminated or reversed by using prisms or pinhole pupils placed in different regions of the pupil. If the pinhole pupils are decentred symmetrically temporally in front of the natural pupils, the red object will appear closer than the blue (positive chromostereopsis) and if they are decentred nasally, the blue object appears closer than the red (negative chromostereopsis). Apparent depth is eliminated when the pinholes are centred on the achromatic axes or when using prisms of appropriate power and direction. Syn. chromatic stereopsis; colour stereoscopy.
See aberration, longitudinal chromatic; parallax, chromatic.
chrysiasis A deposition of gold in tissues, especially the cornea and conjunctiva and the lens leading to cataract. It occurs as a result of prolonged gold therapy (e.g. gold tablets, which are occasionally used in the treatment of rheumatoid arthritis).
cicatricial ectropion; entropion; pemphigoid See under the nouns.
ciclosporin (cyclosporine) An immunosuppressant used in the treatment of the ocular manifestation of autoimmune diseases, uveitis, scleritis, keratoconjunctivitis sicca, ligneous conjunctivitis, and to prevent rejection of corneal grafts, etc. It is believed to exert its immunosuppressive effect by inhibiting the activation of cytotoxic T-lymphocytes.
See immunosuppressants.
CIE standard illuminants See illuminants, CIE standard.
cilia The eyelashes (singular: cilium).
ciliares, striae See stria.
ciliary arteries See arteries, ciliary.
ciliary block glaucoma See glaucoma, ciliary block.
ciliary body Part of the uvea, anterior to the ora serrata and extending to the root of the iris where it is attached to the scleral spur. It comprises the ciliary muscle and the ciliary processes and is roughly triangular in sagittal section. The whole ciliary body forms a ring. The part just beyond the ora serrata is smooth and is thus known as pars plana (orbiculus ciliaris). Anterior to this lies a region of ridges, which are the ciliary processes; this region is called the pars plicata (corona ciliaris). From the sclera inward the ciliary body consists of: the supraciliaris (supraciliary layers) which is made up of strands of collagen containing melanocytes and fibroblasts; the ciliary stroma which contains blood vessels, melanocytes and the ciliary muscle; and the ciliary epithelium which comprises an inner non-pigmented layer and an outer pigmented layer and is a continuation of the internal limiting membrane of the retina and of the retinal pigment epithelium, respectively. The cells of these layers (particularly those of the non-pigmented layer) appear to be actively engaged in ion and water transport and the production of aqueous humour.
See angle recession; cyclitis; iridodialysis; space, supraciliary; stria; ultrafiltration.
ciliary epithelium See ciliary body.
ciliary flush See injection, ciliary.
ciliary ganglion; injection See under the nouns.
ciliary margin See iris, plateau.
ciliary muscle See muscle, ciliary.
ciliary nerve See nerve, long ciliary.
ciliary processes About 70 ridges, some 2 mm long and 0.5 mm high, arranged meridionally and forming the pars plicata of the ciliary body. The ciliary processes consist essentially of blood vessels which are the continuation forward of those of the choroid. The region of the ciliary processes is the most vascular of the whole eye. The ciliary epithelium of the processes, which projects from the ciliary body, is involved in the secretion of aqueous humour.
See diffusion; humour, aqueous rate of outflow; stria; transport, active; ultrafiltration.
ciliary ring See annulus ciliaris.
ciliary sulcus See sulcus, ciliary.
ciliosis Spasmodic twitching of the eyelids.
cilium An eyelash (plural: cilia).
ciprofloxacin See antibiotic.
circadian rhythm See rhythm, circadian.
circle, blur; of confusion See blur circle.
circle of Haller See circle of Zinn.
circle of least confusion The smallest cross-section of a circular bundle of an astigmatic pencil formed by an astigmatic lens and situated between the two focal lines.
See astigmatism; Sturm, conoid of.
circle of Vieth–Müller See horopter, Vieth–Müller.
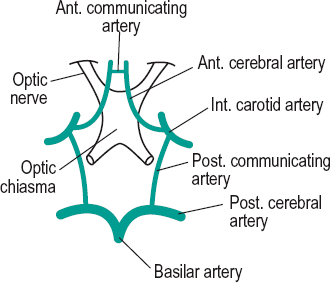
circle of Willis An arterial ring surrounding the optic chiasma and hypothalamus. It is formed anteriorly by the anterior cerebral arteries which are linked by the anterior communicating artery; posteriorly, by the division of the basilar artery into the posterior cerebral arteries and, laterally the latter are united by the posterior communicating arteries to the internal carotid arteries. An aneurysm in one part of the circle of Willis may compress the optic chiasma, resulting in a visual field loss. As the terminal branches of the internal carotid arteries are called the middle cerebral arteries, the circle of Willis is sometimes considered to be formed laterally by the latter (Fig. C11).
See artery, internal carotid; haemorrhage, preretinal; hemianopia, heteronymous.
circle of Zinn Anastomosing circle of short ciliary arteries which have pierced the sclera about the optic nerve. Branches pass forward to the choroid, inward to the optic nerve and backward to the pial network. Syn. circle of Haller.
citric acid cycle See cycle, Krebs.
City University test See test, City University colour vision.
CLARE See contact lens acute red eye.
clearance, apical The distance between the posterior surface of a contact lens and the apex of the cornea.
cliff, visual A device for testing depth perception. It consists of two identically patterned horizontal surfaces, one well below the other; the upper is extended over the lower by means of a sheet of transparent glass. A subject (usually a newborn of a species) placed in the centre of the upper surface and who is unwilling to move onto the transparent glass that projects over the lower surface is assumed to possess depth perception. Many species have been found to possess depth perception at birth, indicating an innate sense, unaffected by learning experience.
clinical interferometer See maxwellian view system, clinical.
clinical trial See trial, randomized controlled.
clinometer Apparatus used to measure ocular torsion.
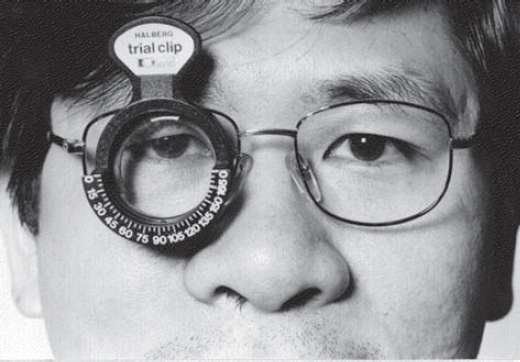
clip, Halberg Trade name for a plastic device with two cells used for holding trial lenses which is clipped over a lens of a pair of spectacles (Fig. C12).
clip-on See clipover.
clipover An attachment holding an auxiliary lens or lenses (an add, a prism or a tint) in front of spectacles by spring action. There are many (albeit similar) types of clips that fit over one lens of a pair of spectacles (e.g. Bernell clip, Bommarito clip, Halberg clip, Jannelli clip). They are used extensively in the refraction of low vision patients. Syn. clip-on; fit-over; trial lens clip.
clip, trial lens See clipover.
clobetasone See antiinflammatory drug.
clock dial chart See chart, astigmatic fan.
Cloquet’s canal See canal, hyaloid.
chloramphenicol See antibiotic.
closed-angle glaucoma See glaucoma, angle-closure.
clotrimazole See antifungal agent.
clouding, central corneal Diffuse, hazy appearance of the cornea due to oedema of the central region of the cornea, usually associated with the wearing of hard contact lenses (mainly PMMA), but it may also occur in keratoconus, Fuch’s endothelial dystrophy or disciform keratitis. It is most easily seen with a slit-lamp using retroillumination against the pupil margin or sclerotic scatter illumination. This condition may give rise to Sattler’s veil.
coating Process of depositing a thin film of transparent material on the surface of an optical element (e.g. lens, mirror, prism) for the purpose of decreasing or increasing reflection. Reflection from specific wavelengths can be reduced or eliminated by varying the thickness of the film and by multilayer coating. Syn. blooming.
See anti-reflection coating; body, white; filter, bandpass; Fresnel’s formula.
Coats’ disease; white ring See under the nouns.
cobalt-blue glass See lens, cobalt.
cobblestones See conjunctivitis, giant papillary; conjunctivitis, vernal.
cocaine Alkaloid derivative from coca leaves used as a local anaesthetic. It also produces a small dilatation of the pupil but does not act on the ciliary muscle.
Cochet–Bonnet aesthesiometer See aesthesiometer.
Cogan’s lid twitch sign See sign, Cogan’s lid twitch.
Cogan’s microcystic epithelial dystrophy See dystrophy, Cogan’s microcystic epithelial.
Cogan’s syndrome See keratitis, interstitial.
Cogan–Reese syndrome See syndrome, ICE.
cognitive retinoscopy See retinoscopy, dynamic.
coherence Property of electromagnetic waves to remain in phase, the maxima and minima of all waves being coincident.
coherent sources If light beams from two independent sources reach the same point in space, there is no fixed relationship between the phases of the two light beams and they will not combine to form interference effects. Such light waves are called incoherent. If, on the other hand, the two light beams are superimposed after reaching the same point by different paths but are both radiated from one point of a source, interference effects will be seen because the phase difference in the two beams is constant. The two virtual sources from which these two beams are apparently coming are called coherent sources and any rays in which there is a constant phase difference are called coherent rays. Prior to the advent of the laser, the only way in which one could obtain coherent rays was by dividing the light coming from a point source into two parts.
See experiment, Young’s; holography; maxwellian view system, clinical; tomography, optical coherence.
collagen The major protein of the white fibres of connective tissue, cartilage, tendons and bones. It is strong, fibrous, insoluble in water, rich in glycine and proline and can be hydrolysed into gelatin by boiling. In the eye it forms the primary structural component of the cornea, lens capsule, ciliary body, vitreous base and sclera. Collagen material is also used to make punctal occlusion plugs used to treat keratoconjunctivitis sicca, and dissolvable therapeutic contact lenses to deliver high-dose drugs to the cornea. Mutations in collagen genes are a common cause of connective tissue disorders.
See connective tissue disorders; occlusion, punctal.
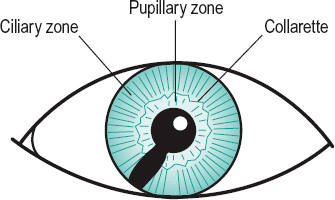
collarette Line separating the pupillary zone and the ciliary zone which can be seen on the anterior surface of the iris. In the normal iris it is an irregular circular line lying about 1.5 mm from the pupillary margin (Fig. C13).
See arterial circle of the iris, minor; Fuchs, crypts of.
colliculi, inferior Two small rounded elevations situated on the dorsal aspect of the midbrain just below the two superior colliculi. They are relay centres for auditory fibres. Syn. inferior corpora quadrigemina.
colliculi, superior Two small rounded elevations situated on the dorsal aspects of the midbrain, just below the thalamus. Besides receiving fibres from each other, they receive a small number of axons from the optic tracts and serve as a relay centre for movements of the eyes, head and neck in response to visual and other stimuli. Singular: colliculus. Syn. superior corpora quadrigemina.
See brachium; pathway, retinotectal; pretectum; syndrome, Parinaud’s.
Collier’s sign See sign, Collier’s.
collimation 1. The making of a bundle of light rays parallel. 2. In radiography, limiting the size of the beam to the required region on the patient, thereby protecting the remainder of the patient from radiation.
collimator An optical apparatus for producing parallel rays of light. It usually consists of a positive achromatic lens, with an illuminated object (a slit, a graticule, a scale, etc.) placed at one of its focal points, so that light from any point on the object emerges from the collimator parallel.
colloid bodies See drusen.
collyrium An eye lotion. It does not, usually, contain any ocular medication. Example: physiological saline.
coloboma Congenital, pathological or operative anomaly in which a portion of the structure of the eye is lacking, e.g. coloboma of the choroid, coloboma of the eyelid, coloboma of the iris, coloboma of the lens, coloboma of the retina, etc. Typical colobomas result from defective closure of the embryonic fissure of the optic cup. Congenital iris colobomas are usually located inferiorly. They are often associated with Crouzon’s syndrome (Fig. C13). Lid colobomas are commonly associated with Treacher–Collins syndrome. Coloboma of the optic disc is characterized by a glistening, white excavation, decentred inferiorly. It is sometimes confounded with glaucomatous cupping, especially when it is accompanied by a field defect. The condition is often associated with microphthalmia and several syndromes (e.g. Edward’s syndrome, Patau’s syndrome).
coloboma, Fuchs’ See crescent, congenital scleral.
color See colour.
colorimeter An instrument for measuring a coloured stimulus by matching it with a known coloured sample.
Table C4
Principal colours of the visible spectrum (approximate range)
| colour | wavelength (nm) |
| violet | 380–450 |
| blue | 451–490 |
| green | 491–560 |
| yellow | 561–590 |
| orange | 591–630 |
| red | 631–780 |
colorimeter, photoelectric Colorimeter using a photoelectric cell and appropriate filters instead of the eye.
colorimetry The measurement of colour in terms of hue, saturation and brightness or other standard (spectral purity, spectral energy, etc.).
colour An aspect of visual perception, characterized by the attributes of hue, brightness and saturation, and resulting from stimulation of the retina by visible photopic light levels. Note: also spelled color.
achromatic c. A visual sensation resulting from a stimulus having brightness, but devoid of hue or saturation, e.g. white, grey.
c. agnosia See agnosia.
c. blindness See blindness, colour.
complementary c. One of a pair of colours which, when mixed additively, produce white or grey (that is to say an achromatic sensation). Examples: green is the complementary colour of red-purple and yellow is the complementary colour of blue.
See chromaticity diagram.
confusion c’s. Colours that are confused by a dichromat. The colours confused by a deuteranope, a protanope and a tritanope are not the same. For example, the deuteranope will confuse reds, greens and greys, whereas the protanope will confuse reds, oranges, blue-greens and greys.
See plates, pseudoisochromatic.
c. constancy See constancy, colour.
c. contrast See contrast, colour.
defective c. vision Marked departure of an individual’s colour vision aptitude from that of a normal observer. This is indicated by various tests, e.g. anomaloscope, pseudoisochromatic plates, Farnsworth test. The following types of defective colour vision are usually recognized: anomalous trichromatic vision or anomalous trichromatism; dichromatic vision or dichromatism; monochromatic vision or monochromatism (total colour blindness), anomaly of vision in which there is perception of luminance but not of colour. Both anomalous trichromatism and dichromatism occur in three distinct forms called respectively protanomalous vision and protanopia, deuteranomalous vision and deuteranopia, tritanomalous vision and tritanopia.
The causes of defective colour vision may be an impairment of a cone pigment or a reduced number of cone cells. The majority of cases of defective colour vision are inherited and thus bilateral. Acquired defects are rare, mostly tritanopic and appear in one eye or are asymmetric, and affect males and females equally. They may be due to glaucoma, retinal or optic nerve disease, drug or chemical toxicity, diabetes, retinitis pigmentosa, etc. Hence it is essential to test colour vision under monocular conditions. The inherited type occurs as a sex-linked disorder in which the defective gene is on the X chromosome. Since men have only one X chromosome while women have two, sex-linked disorders (most being X-linked recessive) affect mainly males who inherit the genetic defect from their mother. Inherited tritanopia and tritanomaly are usually autosomal dominant. For women to show the defect, both of their X chromosomes have to carry the defective gene, a rare occurrence. Defective colour vision occurs in about 8% of the male population and 0.5% of the female population. Syn. daltonism.
See achromatopsia; anomaloscope; deuteranomaly; deuteranopia; inheritance; lens, ChromaGen; lens, X-Chrom; monochromat; pigment, visual; protanomaly; protanopia; rule, Kollner’s; test, colour vision; tritanomaly; tritanopia.
c. fringes Coloured edges around images formed by a lens or an optical system which is not corrected for chromatic aberration.
fundamental c’s. See colours, primary.
c. induction See induction, colour.
c. matching Action of making a colour appear the same as a given colour.
metameric c. Spectrally different radiations that produce the same colour under the same viewing conditions. Note: The corresponding property is called metamerism. Syn. metamers (CIE).
c. mixture The production of a colour by mixing two or more lights of different colours (additive colour mixture) or two or more pigments (subtractive colour mixture).
See colour, complementary; colours, primary.
Munsell c. See Munsell colour system.
non-spectral c. Any colour that does not exist as a single wavelength. Example: purple, which is a mixture of blue and red radiations.
See purple.
primary c’s. Any sets of three colours such as, for example, red, green and blue, which, by additive colour mixture of the stimuli in varying proportions, can produce any colour sensation. Syn. fundamental colours.
spectral c’s. The colours produced by the various radiations of the visible spectrum. See light.
c. stereoscopy See chromostereopsis.
surface c. Colour perceived as belonging to a surface of an object which is not self-luminous.
c. temperature The temperature of the surface of an ideal black body which emits radiations of the same chromaticity as that from the source being specified. As the temperature increases, the amount of radiations increases and the source changes colour from red through to white to bluewhite. Unit: Kelvin (symbol: K).
c. triangle See chromaticity diagram.
c. vision, aetiology of See colour vision, defective.
colour-opponent cells See cells, colour-opponent.
column, cortical In the visual cortex, neurons with similar properties are arranged in columns (about 2 mm high) perpendicular to the surface of the cortex. The columns traverse the six cortical layers until they reach the white matter. Neurons throughout a column respond either to stimuli oriented at the same angle (orientation column) or to the inputs from the same eye (ocular dominance column, ocular dominance slab). A neighbouring column will then have neurons responding to a slightly different orientation from the one next to it and perhaps the same eye or the other eye. Neurons in layer 4 represent an exception, as they may respond to any orientation or to one eye only. Strabismus in early childhood disrupts the development of ocular dominance columns, thus preventing the development of depth perception.
Table C5
Approximate colour temperature (in K) of some light sources
| clear blue sky | 12000–26000 |
| overcast sky | 6600 |
| sun | 5000–6000 |
| electronic flash | about 5600 |
| moonlight | 4000 |
| tungsten-halogen lamp | 3000 |
| tungsten filament lamp | 2600 |
| candle flame | 2000 |
Table C6
Prevalence (%) and classification of colour vision defects
| anomalous trichromats | |||
| deuteranomal | protanomal | tritanomal | |
| male | 4.6% | 1% | 0.0001% |
| female | 0.35% | 0.03% | unknown |
| colour response | slight green deficiency | red deficiency | blue deficiency |
| dichromats | |||
| deuteranope | protanope | tritanope | |
| male | 1% | 1.1% | 0.005% |
| female | 0.01% | 0.01% | 0.003% |
| colour response | green deficiency | insensitive to red | blue deficiency |
| neutral point | 498 nm | 493 nm | 570 nm |
| monochromats | |||
| cone monochromat | rod monochromat | ||
| unknown | 0.003% | ||
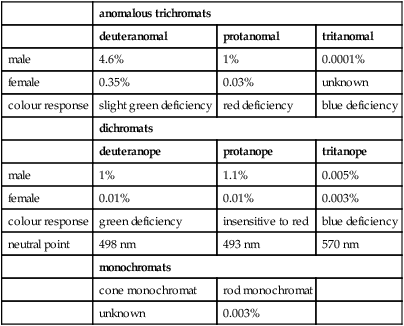
See area, visual; blobs; hypercolumn.
coma Monochromatic aberration of an optical system produced when the incident light beam makes an angle with the optical axis. The image appears like a comet with the tail pointing towards the axis.
See lens, aplanatic; sine condition.
combination lens See lens, combination.
combination system See lens, piggy-back.
comitance See concomitance.
commissure Band of nerve fibres connecting corresponding structures in the brain or spinal cord.
See corpus callosum.
commotio retinae See disease, Berlin’s.
compensated heterophoria See heterophoria, compensated.
compensating prism See prism, relieving.
compensatory eye movements See reflex, static eye.
complementary after-image; colour See under the nouns.
complex cell See cell, complex.
compliance The willingness to strictly follow the instructions given by a clinician. Example: following the cleaning instructions and wearing schedule given after contact lens fitting.
compound astigmatism; eye; optical system See under the nouns.
computer vision syndrome See syndrome, computer vision.
computerized perimeter; tomography See under the nouns.
concave Pertaining to a surface shaped like the inside of a sphere.
See lens, diverging; mirror, concave.
concomitance The condition in which the two eyes move as a unit, that is maintaining a constant angle between them for all directions of gaze when fixating at a fixed distance. Syn. comitance.
See incomitance; strabismus, concomitant.
concretions, conjunctival Minute, hard, whitish spots of calcium present in the palpebral conjunctiva due to cellular degeneration. This condition occurs most commonly in the elderly or in people with prolonged conjunctivitis. They are asymptomatic but may be removed with a needle. Syn. conjunctival lithiasis.
condenser An optical system with a large aperture and small focal length used in microscopes and projectors in order to concentrate as much light as possible onto an object. Syn. condensing lens.
condenser, Abbé’s Microscope substage condenser consisting of a doublet with a high numerical aperture.
See aperture, numerical; doublet; triplet.
condensing lens See condenser.
cone degeneration; dystrophy See dystrophy, cone.
cone monochromat See monochromat.
cone pedicle The wide synaptic terminal of a cone photoreceptor located in the outer molecular (outer plexiform) layer of the retina. There are deep pits (invaginations) in the base of the terminal that contain the dendrites of bipolar and horizontal cells, often two of the former and one of the latter, in each invagination. The neurotransmitter is glutamate, which is stored in vesicles contained in the terminals, and when the photoreceptors are stimulated by light the release of glutamate is decreased.
See cell, cone; hyperpolarization; neurotransmitter
cone-rod dystrophy See dystrophy, cone-rod.
confocal Having the same focus. Example: in a slit-lamp, the microscope and the illumination system have the same focus, i.e. they are confocal.
See microscope, confocal; ophthalmoscope, confocal scanning laser.
confrontation test See test, confrontation.
confusion, circle of See blur circle.
confusion colours See colours, confusion.
congenital Pertaining to a condition that dates from the time of birth. It may be inherited or caused by an environmental factor.
See acquired; familial; hereditary.
congruous scotomas See scotomas, congruous.
conical cornea See keratoconus.
conjugate distances See distances, conjugate.
conjugate movements See version.
conjugate pointsSee distances, conjugate.
conjunctiva A thin transparent mucous membrane lining the posterior surface of the eyelids from the eyelid margin and reflected forward onto the anterior part of the eyeball where it merges with the corneal epithelium at the limbus. It thus forms a sac, the conjunctival sac, which is open at the palpebral fissure and closed when the eyes are shut. The depths of the unextended sac are 14–16 mm superiorly and 9–11 mm inferiorly. The conjunctiva is divided into three portions: (1) The portion that lines the posterior surface of the eyelids is called the palpebral conjunctiva. It is itself composed of the marginal conjunctiva, which extends from the eyelid margin to the tarsal conjunctiva; the tarsal conjunctiva, which extends from the marginal conjunctiva to the orbital conjunctiva; and the orbital conjunctiva, which extends from the tarsal conjunctiva to the fornix. (2) That lining the eyeball is the bulbar conjunctiva. It is itself composed of the limbal conjunctiva, which is fused with the episclera at the limbus and the scleral conjunctiva, which extends from the limbal conjunctiva to the fornix. (3) The intermediate part forming the bottom of the conjunctival sac, unattached to the eyelids or the eyeball and joining the bulbar and the palpebral portion is called the fornix (conjunctival fold, cul-de-sac).
See dyskeratosis; eversion, lid; gland, conjunctival; Krause’s end bulbs; sulcus, subtarsal.
conjunctiva, corneal The stratified squamous epithelium of the cornea.
conjunctival injection See injection, conjunctival.
conjunctival lithiasis See concretions, conjunctival.
conjunctival naevus See naevus, conjunctival.
conjunctival sac See conjunctiva.
conjunctivitis Inflammation of the conjunctiva. It may be acute, subacute or chronic. It may be due to an allergy, an infection (e.g. Staphylococcus, Streptococcus, Haemophilus, etc.), a virus inflammation, an irritant (dust, wind, chemical fumes, ultraviolet radiation or contact lenses), or as a complication of gonorrhoea, syphilis, influenzae, hay fever, measles, etc. Conjunctivitis is characterized by various signs and symptoms, which may include conjunctival injection, oedema, small follicles or papillae, secretions (purulent, mucopurulent, membranous, pseudomembranous or catarrhal), pain, itching, grittiness and blepharospasm. The most common type of conjunctivitis is that due to a bacterium and in many cases is self-limiting and subsides without treatment. Treatment of that type includes irrigation of the lid and the use of topical antibiotics.
See concretions, conjunctival; herpes zoster ophthalmicus; injection, conjunctival; mycophthalmia; ophthalmia neonatorum; syndrome, Stevens–Johnson; trachoma.
actinic c. See keratoconjunctivitis, actinic.
acute c. Conjunctivitis characterized by an onset of hyperaemia (most intense near the fornices), purulent or mucopurulent discharge and symptoms of irritation, grittiness and sticking together of the eyelids on waking. In severe cases there will be chemosis, eyelid oedema, subconjunctival haemorrhages and photophobia. The bacterial type is caused by Staphylococcus epidermidis, Staph. aureus, Haemophilus influenzae (H. aegyptius, Koch–Weeks bacillus), Streptococcus pneumoniae (pneumococcus). A rare form of acute conjunctivitis is caused by the Neisseria species (gonococcus, meningococcus, e.g. gonococcal conjunctivitis), which produce a more severe form of the disease referred to as hyperacute bacterial conjunctivitis or acute purulent conjunctivitis. These require immediate treatment with systemic and topical antibiotics. Acute conjunctivitis is also caused by viruses (viral conjunctivitis), such as herpes simplex or adenoviruses. All forms of acute conjunctivitis occasionally spread to the cornea. Bacterial conjunctivitis often resolves without treatment within two weeks. Management consists of topical antibiotic therapy (e.g. chloramphenicol, erythromycin) and cold compresses to relieve symptoms. Acute allergic conjunctivitis most typically resolves spontaneously, otherwise treatment includes sodium cromoglicate. Acute viral conjunctivitis caused by herpes simplex is treated with antiviral agents (e.g. acyclovir), although viral conjunctivitis caused by other viruses does not respond well to any drug therapy. Supportive treatment such as cold compresses relieves symptoms.
acute haemorrhagic c. A highly contagious viral infection of the anterior segment resulting in haemorrhage of the bulbar conjunctiva. The infection is caused by a picornavirus, often associated with pre-auricular adenopathy and a follicular conjunctivitis. The infection is self-limited and lasts 7–10 days. No specific treatment is presently available.
adult inclusion c. An acute conjunctivitis caused by the serotypes D to K of Chlamydia trachomatis and typically occurring in sexually active adults in whom the genitourinary tract is infected. Signs in the eye usually appear one week following sexual exposure. It may also occur after using contaminated eye cosmetics or soon after having been in a public swimming pool, or in newborn infants (called neonatal inclusion conjunctivitis or neonatal chlamydial conjunctivitis), which is transmitted from the mother during delivery and appears some 5 to 14 days after birth. The conjunctivitis is mucopurulent with follicles in the fornices, which often spread to the limbal region. The condition is commonly associated with punctate epithelial keratitis, preauricular lymphadenopathy, marginal infiltrates and, in long-standing infection, micropannus in the superior corneal region may also appear. Differentiation from viral follicular conjunctivitis is made through culture, serological and cytological studies. Treatment consists of using both systemic and topical tetracyclines, although in pregnant or lactating women erythromycin is preferable. Syn. trachoma-inclusion conjunctivitis (TRIC).
See follicle, conjunctival; keratitis, punctate epithelial; lymphadenopathy; ophthalmia neonatorum; trachoma.
allergic c. Conjunctivitis which is due to a type 1 hypersensitivity reaction to allergens. Common allergens are pollens associated with hay fever, grass (seasonal allergic conjunctivitis) and air pollutants, house dust mites, smoke (perennial allergic conjunctivitis). It is characterized by hyperaemia, itching, burning, swelling, tearing, discharge and small papillae. Conjunctival scrapings contain a large number of eosinophils and serum IgE is elevated. The condition is commonly associated with rhinitis (allergic rhinoconjunctivitis) in which there is also sneezing and nasal discharge. Treatment commonly includes decongestants, oral antihistamines, mast cell stabilizers (e.g. lodoxamine, sodium cromoglicate) and if severe, topical corticosteroid eyedrops.
See conjunctivitis, vernal; decongestants; hypersensitivity.
angular c. Subacute bilateral inflammation of the conjunctiva due to the diplobacillus of Morax–Axenfeld. It involves the conjunctiva in the region of the canthi.
bacterial c. See conjunctivitis, acute.
catarrhal c. Type of conjunctivitis associated with the common cold or catarrhal irritation. It can appear in the acute or chronic form.
contagious c. Acute conjunctivitis caused by Koch–Weeks bacillus, adenovirus types 3, 7 or 8 and 19, or a pneumococcus infection. It may be transmitted by respiratory or ocular infections, contaminated towels or equipment (e.g. tonometer heads). It is characterized by acute onset, redness, tearing, discomfort and photophobia. The condition is often self-limiting but keratitis is a common complication. Syn. epidemic conjunctivitis; epidemic keratoconjunctivitis; pink eye (colloquial).
eczematous c. See conjunctivitis, phlyctenular.
egyptian c. See trachoma.
epidemic c. See conjunctivitis, contagious.
flash c. Conjunctivitis due to exposure to an electric arc, as from a welder’s torch.
follicular c. Conjunctivitis characterized by follicles (usually in one eye only) caused by adenoviruses or chemical or toxic irritation and frequently associated with lymphadenopathy.
See conjunctivitis, adult inclusion; follicle, conjunctival; lymphadenopathy.
fungal c. See mycophthalmia.
giant papillary c. (GPC) Conjunctivitis, characterized by the appearance of ‘cobblestones’ (large papillae of 0.5 mm or more) on the tarsal conjunctiva of the upper eyelid (and sometimes the lower eyelid). Symptoms include itching, discomfort, mucous discharge and poor vision due to the presence of mucus. The condition may be induced by contact lens wear, ocular prosthesis, or exposed sutures following surgery. This conjunctivitis closely resembles vernal conjunctivitis and is also believed to be an allergic condition. In its early stages as a contact lens-induced condition, it is often referred to as contact lens papillary conjunctivitis or contact lens associated papillary conjunctivitis (CLPC, CLAPC). In these cases the regular use of surfactant and protein removal tablets as well as frequent lens replacement reduce the incidence of this condition, which is less prevalent with the wear of rigid gas permeable than soft contact lenses. Management may also include mast cell stabilizers (e.g. sodium cromoglicate) or antihistamine (e.g. levocabastine) and cessation of lens wear.
See conjunctivitis, vernal; deposits, contact lens; enzyme; surfactant.
gonococcal c. See conjunctivitis, acute.
granular c. See trachoma.
lacrimal c. Chronic conjunctivitis caused by an infection of the lacrimal passages.
See lacrimal apparatus.
ligneous c. A rare, chronic conjunctivitis characterized by the formation of a firm, whitish membrane or pseudomembrane on the tarsal conjunctiva, usually of the upper eyelid. It is typically bilateral, begins in childhood although it may present in patients up to age 85, is more common in females than in males and may persist for months or years. Its cause is unknown but the predisposing factors include bacterial and viral infections, trauma, hypersensitivity reactions and increased vascular permeability, and it is often associated with inflammations of other mucous membranes. The most effective treatment is surgical excision followed by topical cyclosporine drops, but the condition has a tendency to recur.
See conjunctivitis, pseudomembranous.
membranous c. See conjunctivitis, pseudomembranous.
neonatal c. See ophthalmia neonatorum.
phlyctenular c. See keratoconjunctivitis, phlyctenular.
pseudomembranous c. A non-specific inflammatory reaction characterized by the formation on the conjunctiva of a coagulated fibrinous plaque consisting of inflammatory cells and an exudate containing mucus and proteins. This plaque forms either a membrane or a pseudomembrane. The latter is loosely adherent to the conjunctival epithelium and can be peeled off without bleeding or damage to the underlying epithelium. A true membrane, on the other hand, usually occurs with intense inflammation (membranous conjunctivitis). In this case the conjunctival epithelium becomes necrotic and adheres firmly to the overlying membrane which when peeled leaves a raw, bleeding surface. The cause of either condition may be an infection, of which the common sources are herpes simplex virus, adenovirus, beta-haemolytic Streptococcus, Neisseria gonorrhoeae or as a result of the Stevens–Johnson syndrome, ligneous conjunctivitis, ocular cicatricial pemphigoid, atopic keratoconjunctivitis, chemical burns (especially alkali burns), radiation injury or post-surgical complications.
sun lamp c. See keratoconjunctivitis, actinic.
swimming pool c. See conjunctivitis, adult inclusion.
vernal c. Chronic, bilateral conjunctivitis which recurs in the spring and summer and is more often seen in boys than girls. Its origin is probably due to an allergy. It is characterized by hard flattened papillae of a bluish-white colour separated by furrows and having the appearance of ‘cobblestones’ located in the upper palpebral portion of the conjunctiva with mucus deposition between the papillae. A second type of vernal conjunctivitis exists which affects the limbal region of the bulbar conjunctiva, characterized by the formation of small, gelatinous white dots called Trantas’ dots or Horner–Trantas’ dots. The chief symptom of the disease is intense i tching. Treatment consists mainly of cold compresses and limited (because of side effects) use of topical corticosteroids (e.g. dexamethasone, prednisolone). Sodium cromoglicate or lodoxamide have also been found to be very successful in treating this condition and with fewer side effects than corticosteroids. Syn. vernal keratoconjunctivitis (VKC) (although this is not strictly speaking a synonym since the condition often involves the cornea; spring catarrh; vernal catarrh (Fig. C14).
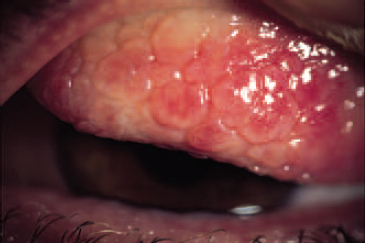
See antihistamine; keratoconjunctivitis, atopic; mast cell stabilizers.
viral c. Conjunctivitis caused by a virus. A variety of viruses can produce the disease.
See conjunctivitis, acute.
connective tissue disorders Inherited conditions resulting from mutations that adversely affect the structure of connective tissues, such as the cornea, sclera, tendons and ligaments. Examples: Ehlers–Danlos syndrome, Marfan’s syndrome, osteogenesis imperfecta, pseudoxanthoma elasticum, rheumatoid arthritis, scleroderma, Sjögren’s syndrome, Stickler’s syndrome.
conoid of Sturm See Sturm, conoid of.
consecutive esotropia; exotropia; strabismus See strabismus, consecutive.
consensual See reflex, pupil light.
consent A voluntary approval from a person to be examined, treated or subjected to any test undertaken upon them. Consent must be obtained prior to any such intervention.
constancy Perceptual phenomenon whereby the properties of certain objects appear to remain relatively constant, despite changes in the stimulus characteristics which induced the perception. All constancies occur only within a limited range.
brightness c. Perceptual phenomenon whereby the brightness of an object appears to remain relatively constant, despite changes in the level of its illumination. Example: white paper appears white whether it is seen in sunlight or in the weaker or yellower illumination of a light bulb. Syn. lightness constancy.
colour c. Perceptual phenomenon whereby the colour of an object appears to remain relatively constant, despite changes in the spectral composition of the incident light.
shape c. Perceptual phenomenon whereby the shape of an object appears to remain relatively constant, despite changes in the viewing angle. Example: A circle held obliquely to the line of sight appears more circular than it should due to shape constancy although its retinal projection is oval.
size c. Perceptual phenomenon whereby the size of an object appears to remain relatively constant, despite changes in the viewing distance (and therefore of its retinal image size).
constants of the eye Average dimensions of the various parameters of the eye adopted to represent a typical eye. These vary slightly depending upon the authors, such as Donders, Gullstrand, Bennett–Rabbetts, etc.
See eye, reduced; eye, schematic.
constant, Planck’s See photon.
constringence A positive number (symbol: V) which specifies any transparent medium. It is equal to
< ?xml:namespace prefix = "mml" />
where nD, nF and nC are the refractive indices for the Fraunhofer spectral lines d (587.6 nm), F (486.1 nm) and C (656.3 nm). A material with a high constringence (e.g. V = 50) produces less chromatic aberration than one with a low constringence (e.g. V = 30). The reciprocal of the constringence is called the dispersive power. Syn. Abbé’s number; V-value.
See dispersion; glass, crown; glass, flint; lines, Fraunhofer’s.
contact arc See arc of contact.
contact lens See lens, contact.
contact lens acute red eye (CLARE) An acute corneal inflammation caused by overnight wear of soft contact lenses. It is characterized by pain, usually unilateral, redness, tearing, photophobia, corneal infiltrates and blurred vision that suddenly appears upon waking. The lens is, in most cases, tight or immobile and it is the breakdown of debris accumulated behind the lens that caused the inflammatory reaction. The lens must be removed immediately and patching of the eye and antiinflammatory therapy may be necessary. Syn. immobile lens syndrome; non-ulcerative keratitis; tight lens syndrome.
Table C7
Optical constants of an average adult Caucasian eye
| structure or surface | refractive index | radius of curvature (mm) | distance from ant. surface of cornea (mm) |
| cornea | 1.376 | – | – |
| aqueous humour | 1.336 | – | – |
| lens (total) | 1.42 | – | – |
| vitreous humour | 1.336 | – | – |
| ant. corneal surface | – | 7.8 | 0 |
| post. corneal surface | – | 6.7 | 0.5 |
| ant. lens surface | – | 10.6 | 3.6 |
| accommodated | – | 6.1 | 3.2 |
| post. lens surface | – | –6.2 | 7.2 |
| accommodated | – | –5.3 | 7.2 |
| retina | 1.363 | – | 24.1 |
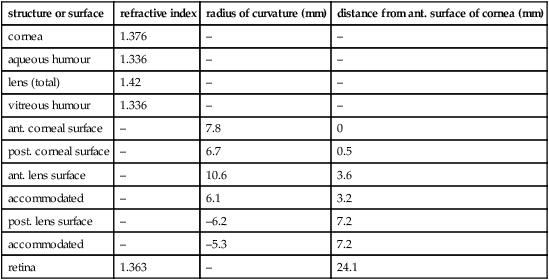
Table C8
Constringence (V) of some transparent media (index of refraction n)
| n | V | |
| glass | ||
| spectacle crown | 1.523 | 59 |
| dense barium crown | 1.620 | 60 |
| lanthana crown | 1.713 | 54 |
| zinc crown | 1.508 | 61 |
| light flint | 1.581 | 41 |
| dense flint | 1.620 | 36 |
| extra dense flint | 1.706 | 30 |
| titanium oxide | 1.701 | 31 |
| polymer | ||
| PMMA | 1.492 | 57 |
| CR-39 | 1.498 | 59 |
| Polycarbonate | 1.586 | 30 |
| Polystyrene | 1.590 | 31 |
| Water (at 37°C) | 1.331 | 56 |
| Aqueous and vitreous (at 37°C) | 1.334 | 56 |
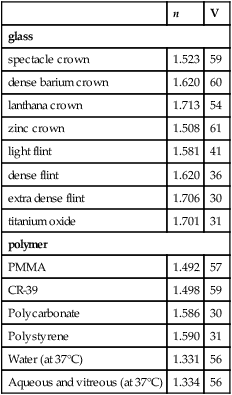
See lens, steep.
contour The outline of a part of a retinal image where the light intensity changes abruptly corresponding to the boundaries of objects in the visual field. The physiological basis of contour perception and edge detection is thought to be mediated by the responses of complex and hypercomplex cells in area V1 of the primary visual cortex.
Illusory c’s. (subjective contours) are contours perceived in the absence of a lightness or colour difference as in the Kanizsa figure. They are thought to be processed in area V2 of the visual cortex.
See areas, visual association; system, parvocellular visual.
c. interaction See Glasgow acuity cards; phenomenon, crowding.
contraindication The presence of a condition or disease which renders some particular type of treatment undesirable. Example: contact lenses are contraindicated in very dusty, dry and smoky atmospheres.
contralateral A term relating to the opposite side.
See geniculate bodies, lateral; ipsilateral.
contraocular Pertaining to the opposite eye.
contrast 1. Subjective sense: subjective assessment of the difference in appearance of two parts of a field of view seen simultaneously or successively. Hence, luminosity contrast, lightness contrast, colour contrast, simultaneous contrast, successive contrast. 2. Objective sense: quantities defined by the formulae for luminance contrast.
Note: Example (c) is better known as luminance ratio (CIE). L2 is the maximum luminance and L1 is the minimum luminance.
See frequency, spatial; sensitivity, contrast; threshold, differential.
brightness c. The enhanced apparent darkening of an area when viewed near, or following a lighter stimulus (or lightening, near or after a darker stimulus).
colour c. 1. A difference in the appearance of surfaces based on hue or saturation. 2. The enhanced difference in the colour of two surfaces induced by their proximity (simultaneous colour contrast) or successive stimulation (successive colour contrast). The appearance of the smaller area shifts towards the complementary colour of the surround or background. Example: a yellow area appears reddish when surrounded by a green background.
c. sensitivity function See function, contrast sensitivity.
c. sensitivity test See chart, contrast sensitivity; sensitivity, contrast.
simultaneous c. A difference in the appearance of two adjacent areas occurring at the same time.
successive c. A difference in the appearance of stimuli following each other.
c. threshold See sensitivity, contrast; threshold, differential.
convention, sign See sign convention.
convergence 1. Movement of the eyes turning inward or towards each other (Fig. C15). 2. Characteristic of a pencil of light rays directed towards a real image point.
See angle of convergence ; vergence.
c. accommodation See accommodation, convergence.
accommodative c. That component of convergence which occurs reflexly in response to a change in accommodation. It is easily demonstrated by having one eye fixate from a far point to a near point along its line of sight, while the other eye is occluded. The occluded eye will be seen to make a convergence movement in response to the accommodation. Alternatively, one eye fixates while the other is occluded. If a minus lens is placed in front of the fixating eye, the occluded eye will be seen to converge. Syn. accommodative vergence; associative convergence.
See convergence, fusional; convergence, initial; convergence, proximal; fusion, motor.
amplitude of c. The angle through which each eye is turned from the far to the near point of convergence. Syn. amplitude of triangulation.
correction induced c. Convergence induced when changing from spectacles to contact lenses in near vision. Spectacles centred for distance vision induce base-in prisms in myopes and base-out prisms in hyperopes, in near vision. Thus, a spectacle-wearing myope converges less and a spectacle-wearing hyperope converges more than an emmetrope fixating at a given distance (Fig. C16). Optically centred contact lenses do not induce any prismatic effect and the amount of convergence remains the same for all refractive errors. Consequently, myopes require more convergence and hyperopes less convergence when they transfer from spectacles to contact lenses. However, this change in convergence is accompanied by a similar change in accommodation, so that a myope transferring to contact lenses converges and accommodates more than with spectacles and the reverse applies for a hyperope.
See accommodation, correction induced; prism, induced.
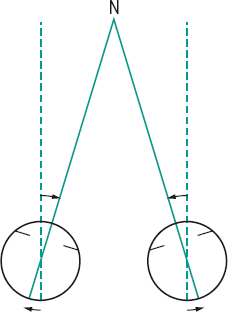
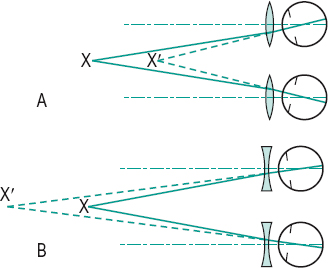
c. excess A high esophoria at near, associated with a relatively orthophoric condition at distance. It usually gives rise to complaints of headaches and other symptoms of asthenopia accompanying prolonged close work.
See accommodative excess.
far point of c. The farthest point where the lines of sight intersect when the eyes diverge to the maximum.
fusional c. That component of convergence which is induced by fusional stimuli or which is available in excess of that required to overcome the heterophoria. It is usually a positive fusional convergence, but in some cases the eyes need to diverge to obtain fusion and this is called negative fusional convergence. An example is the movement of the eyes from the passive (one eye covered, the other fixating an object) to the active (both eyes fixating foveally the same object) position. However, as disparate retinal stimuli are a more powerful component of convergence than fusion, the concept of fusional convergence is being substituted by motor fusion (or disparity vergence).
See convergence, accommodative; convergence, initial; convergence, proximal; convergence, relative; fusion, chiastopic fusion, motor; fusion, orthopic; vergence facility.
fusional reserve c. See convergence, relative.
initial c. Movement of the eyes from the physiological position of rest to the position of single binocular fixation of a distant object in the median plane and on the same level as the eyes. Initial convergence is triggered by the fixation reflex.
See convergence, accommodative; convergence, fusional; position of rest, physiological.
instrument c. See convergence, proximal.
c. insufficiency An inability to converge, or to maintain convergence, usually associated with a high exophoria at near and a relatively orthophoric condition at distance. It results in complaints of fatigue or even diplopia due to the inability to maintain (and sometimes even to obtain) adequate convergence for prolonged close work. Treatment includes orthoptic exercises (e.g. the pencil-to-nose exercise or pencil push-up in which the tip of a pencil is moved slowly towards the eyes while it is maintained singly for as long as possible and this procedure is repeated until the pencil can be brought within 10 cm before doubling occurs), or a reading addition sometimes with BI prisms.
See accommodative insufficiency.
near point of c. (NPC) The nearest point where the lines of sight intersect when the eyes converge to the maximum. This point is normally about 8–10 cm from the spectacle plane. If further away, the patient may have convergence insufficiency.
negative c. See divergence.
proximal c. That component of convergence initiated by the awareness of a near object. For example, when looking into an instrument the image may be at optical infinity yet proximal convergence may be initiated. Syn. instrument convergence; psychic convergence; proximal vergence.
See accommodative, proximal.
psychic c. See convergence, proximal.
relative c. That amount of convergence which can be exerted while the accommodation remains unchanged. Clinically, it is measured by using prisms base-out (positive relative convergence or positive fusional convergence) (Fig. C17) and/or base-in (negative relative convergence or negative fusional convergence) to the limits of blur but single binocular vision. Beyond that limit accommodation changes. If the power of the base-out prism is increased the image, though blurred, will still appear single until the limit of fusional convergence is reached and the image appears double (break point). The prism before the eyes now represents the positive fusional reserve convergence (positive fusional reserve). Similarly, increasing the base-in prism, one reaches the break point, which represents the negative fusional reserve convergence (negative fusional reserve). Syn. relative vergence.
See criterion, Percival; criterion, Sheard; zone of clear, single, binocular vision.
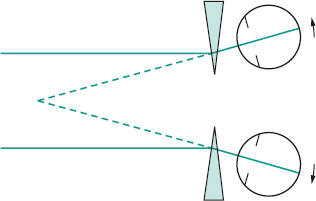
total c. See angle of convergence.
voluntary c. Ability to converge the eyes without the aid of a fixation stimulus. Few people possess this ability but it can be trained in most people.
convergence-retraction nystagmus See nystagmus, convergence-retraction.
convex Having a surface curved like the exterior of a sphere.
See lens, converging; mirror, convex.
copper deposits See chalcosis lentis; disease, Wilson’s.
copper wire artery See arteriosclerosis.
coquille An unsurfaced lens, approximately plano, made by allowing sheet material to sag onto a shaped former (British Standard). This lens is often used in goggles.
corectopia A condition in which the pupil is not situated in the centre of the iris. It may occur as a result of iris melanoma, ocular surgery (e.g. trabeculectomy), trauma or from a congenital defect (e.g. coloboma). Syn. ectopia pupillae.
See luxation of the lens.
coreometer See pupillometer.
cornea The transparent anterior portion of the fibrous coat of the globe of the eye. It has a curvature somewhat greater than the rest of the globe, so a slight furrow marks its junction with the sclera. Looked at from the front the cornea is about 12 mm horizontally and 11 mm vertically. It is the first and most important refracting surface of the eye, having a power of about 42 D. The anterior surface has a radius of curvature of about 7.8 m, the posterior surface 6.5 mm, and the central thickness is about 0.5 mm. It consists of five layers, starting from the outside: (1) the stratified squamous epithelium; (2) Bowman’s layer; (3) the stroma (substantia propria); (4) Descemet’s membrane; and (5) the endothelium. The cornea is avascular, receiving its nourishment by permeation through spaces between the lamellae. The sources of nourishment are the aqueous humour, the tears and the limbal capillaries. The cornea is innervated by the long ciliary and other nerves of the surrounding conjunctiva, which are all branches of the ophthalmic division of the trigeminal nerve. Innervation is entirely sensory. Within the cornea there are only unmyelinated nerve endings. The density of nerves in the cornea is very high, making it the most sensitive structure in the body. The major structural component of the cornea is collagen, mostly type I, and most of the ground substance between the collagen fibrils in the corneal stroma is proteoglycans whose core proteins bind with keratan sulfate and dermatan sulfate (chondroitin sulfate B). The cornea owes its transparency to the regular arrangement of the collagen fibrils, but any factor that affects this lattice structure (e.g. swelling, pressure) results in a loss of transparency. The cornea contains some 78% water, some 15% collagen and some 5% of other proteins (Fig. C18).
See bedewing, endothelial; corneal stroma; corneal topography; dellen; deturgescence; dyskeratosis; glycosaminoglycan; keratitis; keratomycosis; line, Hudson–Stahli; layer, Bowman’s; membrane, Descemet’s; microcornea; microscope, specular ; optical zone of cornea; pachometer; theory, Maurice’s; syndrome, Hurler’s; videokeratoscope.
conical c. See keratoconus.
c. farinata A bilateral corneal degeneration characterized by faint dust-like opacities in the deep stroma. They do not impair vision and are usually age-related.
c. guttata Dystrophy of the endothelial cells of the cornea which may result from corneal trauma, cataract surgery, keratic precipitates, tonography, ageing, continuous contact lens wear, or as part of the early stages of Fuch’s endothelial dystrophy (a disease associated with ageing and with females more than males). It is seen clinically by slit-lamp examination as black spherules in the endothelial pattern. The condition is bilateral, although one eye may be affected more than the other. As the condition progresses the cornea becomes oedematous with a consequent loss of vision and eventually turns into bullous keratopathy. If the degenerated cells are located at the periphery of the cornea they are called Hassall–Henle bodies and are of no clinical significance except as an indication of ageing. Syn. corneal guttae; endothelial corneal dystrophy.
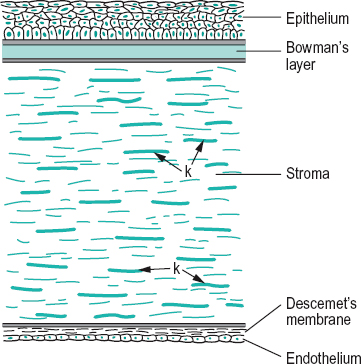
See illumination, specular reflection; keratic precipitates.
optical zone of c. See optical zone of cornea.
c. plana A rare, congenital, usually bilateral condition in which the corneal curvature is flatter than normal with a significant decrease in refractive power. The eye is usually hyperopic with a shallow anterior chamber often resulting in angle-closure glaucoma. There is some degree of peripheral scleralization and it is closely associated with sclerocornea.
corneal Pertaining to the cornea.
corneal abrasion An area of the cornea that has been removed by rubbing. The condition ranges from punctate staining with fluorescein to a total removal of the epithelium. Corneal abrasions may result from overwear of contact lenses, foreign bodies, fingernail scratches, etc. There is pain, photophobia, tearing and blepharospasm. The condition usually heals quickly if not severe and if infection has not occurred. Treatment consists of removal of the foreign bodies, if any, usually by irrigation, tight patching of the eye, and antibiotic ointment; if due to contact lenses, discontinue wear until full recovery. Local anaesthetics should not be used in the treatment as they tend to delay the regeneration of the corneal epithelium.
See mitosis; syndrome, overwear; rose bengal.
corneal acidosis See acidosis.
corneal apex See apex, corneal; optical zone of cornea.
corneal arcus A greyish-white ring (or part of a ring) opacity occurring in the periphery of the cornea, in middle and old age. It is due to a lipid infiltration of the corneal stroma. With age the condition progresses to form a complete ring. That ring is separated from the limbus by a zone of clear cornea. The condition can also appear in early or middle life and is referred to as arcus juvenilis (or anterior embryotoxon); it is somewhat whiter than corneal arcus. Arcus juvenilis is often associated with heart disease in men (Fig. C19). Syn. arcus senilis; gerontoxon.
See furrow, marginal.
corneal bullae See bulla; keratopathy, bullous.
corneal cap See optical zone of cornea.
corneal clouding, central See clouding, central corneal.
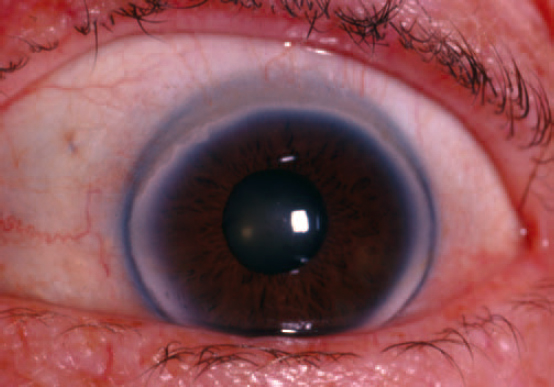
corneal corpuscle Main cellular element of the corneal stroma. It is a flattened, dendritic cell located between the lamellae with a large flattened nucleus and lengthy processes which may communicate with neighbouring cells. These cells have fibroplastic and phagocytic functions. Syn. corneal fibrocyte; fixed cell; keratocyte.
corneal degeneration See degeneration, pellucid marginal corneal; ectasia, corneal; Vogt’s white limbal girdle.
corneal dellen See dellen.
corneal dystrophy; ectasia See under the nouns.
corneal endothelium The posterior layer of the cornea consisting of a single layer of cells, about 5 μm thick, bound together and predominantly hexagonal in shape. The posterior border is in direct contact with the aqueous humour while the anterior border is in contact with Descemet’s membrane. The endothelium is the structure responsible for the relative dehydration of the corneal stroma. The endothelium receives most of its energy from the oxidative breakdown of carbohydrates via the Krebs cycle. In the normal adult eye the cell density varies from around 3000 cells/mm2 in the centre of the cornea to about 2000 cells/mm2 in the periphery. With age, disease or trauma the density of cells decreases but with disease or trauma this reduction may affect corneal transparency, as some fluid then leaks into the cornea.
See bedewing, endothelial; blebs, endothelial; cornea guttata; illumination, specular reflection; microscope, specular; phacoemulsification; polymegethism, endothelial.
corneal epithelium The outermost layer of the cornea consisting of stratified epithelium mounted on a basement membrane. It is made up of various types of cells; next to the basement membrane are the basal cells (columnar in shape), then two or three rows of wing cells and near the surface are two or three layers of thin surface squamous cells (or superficial cells). The outer surfaces of the squamous cells have projections (called microvilli and microplicae), which extend into the mucin layer of the precorneal tear film and are presumed to help retain the tear film. The epithelium in humans has a thickness of about 51 μm. Some dendritic cells of mesodermal origin are also normally present. Epithelial stem cells are located at the limbus; they give rise to the basal cells. The corneal epithelium receives its innervation from the conjunctival and the stromal nerves. The life cycle of epithelial cells is about a week (Fig. C20).
See cell, Langerhans’; epikeratoplasty; mitosis; pachometer; palisades of Vogt.
corneal erosion, recurrent Periodic loss of some of the corneal epithelium, due to its detachment from the basement membrane. It may be the result of trauma (e.g. fingernail scratch) or of some corneal dystrophy. There is severe pain, redness, lacrimation and photophobia, typically upon awakening. Management usually begins with artificial teardrops and a lubricating ointment but the acute phase requires antibiotic ointment and pressure patching or a therapeutic soft contact lens or debridement.
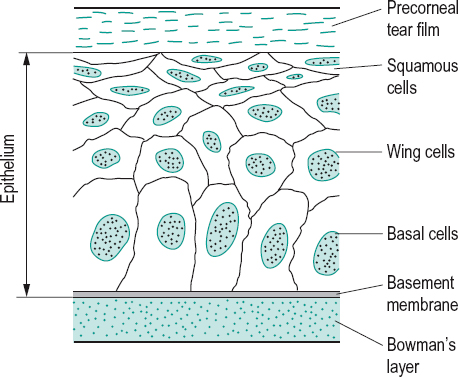
See desmosome; dystrophy, Cogan’s microcystic epithelial; dystrophy, lattice; dystrophy, Reis–Buckler’s.
corneal exhaustion syndrome See syndrome, corneal exhaustion.
corneal facet 1. Small flattened depression on the outer surface of the cornea, due to a healed ulcer which has failed to fill with tissue. 2. The corneal element in the ommatidium of the compound eye.
See eye, compound; ulcer, corneal.
corneal fibrocyte See corneal corpuscle.
corneal fold See oedema.
corneal fragility The ability of the cornea to withstand damage. It is quantified by measuring the corneal damage threshold (CDT) (or corneal epithelial fragility threshold (CFT)), that is the lowest pressure exerted on the cornea (using, e.g., a Cochet–Bonnet aesthesiometer) which produces some ruptured epithelial cells; they can be seen after fluorescein instillation with a slit-lamp and UV filter.
corneal graft See graft, corneal; keratoplasty.
corneal granular dystrophy See dystrophy, granular.
corneal hydrops; hyperaesthesia; hypoxia; image See under the nouns.
corneal infiltrates Small hazy greyish areas (local or diffuse) composed of inflammatory cells, proteins, etc. surrounded by oedema and located in the cornea typically near the limbus. The adjacent conjunctiva is usually hyperaemic. They appear as a result of corneal inflammation (e.g. marginal keratitis, microbial keratitis), reaction to solution preservatives and some contact lens wear (especially extended wear) which causes prolonged hypoxia. Management depends on the cause; for example, if due to contact lenses, cessation of wear is usually indicated, otherwise drug therapy is required.
See keratitis, acanthamoeba; keratoconjunctivitis, superior limbic.
corneal keratocyte See corneal corpuscle.
corneal lens See lens, contact.
corneal limbus See limbus, corneal.
corneal neovascularization See pannus.
corneal opacity See leukoma.
corneal parallelepiped A section of the cornea illuminated by the thin slit of light of a slit-lamp, when viewed obliquely.
corneal reflex; sensitivity See under the nouns.
corneal stria See oedema; stria.
corneal stroma The thickest layer of the cornea located behind Bowman’s layer and in front of Descemet’s membrane. It represents approximately 90% of the total corneal thickness and gives the cornea its strength. The stroma consists of about 300 lamellae of parallel collagen fibrils in the centre of the cornea reaching to nearly 500 lamellae at the limbus. In between the fibrils are proteoglycans whose core proteins bind one with keratan sulfate and the other with dermatan sulfate (chondroitin sulfate B). The orientation of the alternate lamellae differs with each other, but they are all parallel with the corneal surface. In the central part of the cornea the majority of the collagen fibrils are orientated in the inferiorsuperior and nasal-temporal directions, whereas at the limbus they are orientated circumferentially, providing greater resistance to forces perpendicular to the axes of the fibrils. Between the lamellae are found the elongated flattened keratocytes (corneal corpuscles) from which the collagen fibrils are produced during development. When the cornea becomes oedematous due to trauma, disease or hypoxia, some of the fibrils lose their usual uniform calibre, become displaced and fluid accumulates between the lamellae, the stroma then loses its transparency. Syn. substantia propria.
corneal topography A map of the variations in the curvature (and power) of the anterior surface of the cornea. The typical map shows that the average adult cornea is steeper in the vertical than in the horizontal meridian and has the form of a flattening ellipsoid. It is typically done with a photokeratoscope or a videokeratoscope. Corneal topography can also be determined with a scanning-slit topographer, in which a computerized system integrates a series of slit-beam images to produce a map of the curvature and elevation of the anterior and posterior surfaces enabling a diagnosis of anterior and posterior keratoconus, and indirectly providing a measurement of corneal thickness.
See keratoscope; photokeratoscopy; videokeratoscope.
corneal touch threshold (CTT) The minimum pressure (in force per unit area, such as mg/mm2) exerted against the cornea which can just be felt.
See aesthesiometer; hyperaesthesia; sensitivity, corneal.
corneal transplant See keratoplasty.
corneal ulcer See ulcer, corneal.
corneal warpage A relative change in the shape of the corneal surface produced by contact lenses, especially rigid lenses with low or no oxygen transmissibility. It affects vision. It is easily observed with corneal topography. The cornea recovers following cessation of contact lens wear.
See videokeratoscope.
corneoscleral junction See limbus, corneal.
corneoscleral meshwork See meshwork, trabecular.
corona ciliaris See ciliary body.
corpora quadrigemina See colliculi, inferior; colliculi, superior.
corpus callosum Transverse white fibres connecting the two cerebral hemispheres.
See commissure; stereoblindness.
correction 1. Term used to designate the prescription of spectacle or contact lenses to compensate for ametropia (Figs. C21 and C22). Syn. refractive correction. 2. The process whereby the aberrations of an optical system are minimized.
See doublet; lens, aplanatic; triplet.
correspondence, abnormal retinal See retinal correspondence, abnormal.
corresponding points See retinal corresponding points.
cortex of the crystalline lens See lens, crystalline.
cortex, motor Area of the frontal lobe of the brain just anterior to the central sulcus which is responsible for voluntary movements of the eyes (as well as other voluntary movements of other parts of the body). The motor cortex in each hemisphere controls mainly muscles on the opposite side of the body. It is laid out according to the parts of the body, with the region controlling the feet at the top and the region controlling the legs, the trunk, the arms and the head in descending order.
cortex, occipital The superficial grey matter on the posterior part of each hemisphere comprising Brodmann’s areas 17, 18 and 19.
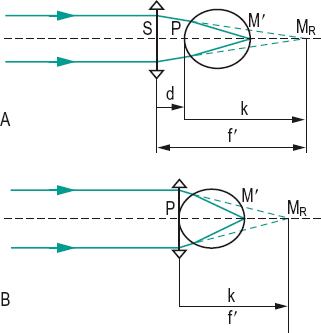
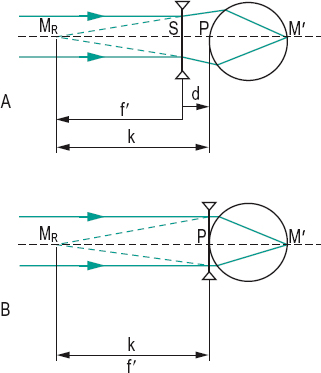
cortex, prestriate See areas, visual association.
cortex, striate; visual See area, visual.
cortical blindness See blindness, cortical.
cortical magnification See magnification, cortical.
cortical vision screening test See test, cortical vision screening.
corticosteroid See antiinflammatory drug.
cosine law See diffusion.
‘cotton balls’ See uveitis, intermediate.
cotton thread test See test, phenol red cotton thread.
cotton-wool spots See bodies, cytoid; exudate.
counting fingers (CF) A method of recording vision in patients who are unable to identify any optotype on an acuity chart. If a patient correctly counts the numbers of the examiner’s fingers shown, this is recorded with the distance at which it is performed.
CR-39 material Allyl diglycol carbonate or Columbia Resin. CR-39 is a light transparent plastic material (refractive index 1.498, V = 59) used in the manufacture of spectacle lenses and much harder than polymethyl methacrylate. It is not quite as hard as glass. Syn. hard resin.
See constringence; lens, plastic.
crescent, congenital scleral A white semilunar patch of sclera seen adjacent to the optic disc due to the fact that the choroid and retinal pigment epithelium do not extend to the optic disc. This condition is present at birth, unlike myopic crescent, and is often associated with defective vision and tilted disc or situs inversus of the disc. Syn. Fuch’s coloboma (if located at the lower edge of the disc).
See disc, situs inversus; disc, tilted.
crescent, myopic A white area of sclera seen adjacent to the temporal side of the optic disc mainly in pathological myopia, but also sometimes in non-pathological myopia. The choroid and retinal pigment epithelium have atrophied in the crescent area, allowing the sclera to be seen. Syn. myopic conus; myopic scleral crescent.
crest, lacrimal See lacrimal crest, anterior; lacrimal crest, posterior.
Crete’s prism See prism, rotary.
cribbing The process of breaking or chipping of excess glass from an uncut lens blank. It is carried out sometimes prior to edging.
cribriform plate This is a part of the sclera which is situated at the site of attachment of the optic nerve, 3 mm to the inner side of and just above the posterior pole of the eye. There, the sclera is a thin sieve-like membrane through which pass fibres of the optic nerve. Syn. lamina cribrosa (although this term also refers to the striated portion of the bulbar optic nerve which includes the cribriform plate).
See fibres, myelinated nerve.
criterion, Percival Rule proposed by Percival to establish whether a patient is going to experience discomfort in binocular vision. It states that if Donders’ line (or demand line) lies within the zone of comfort, which is the middle third of the total range of relative convergence (to the blur points), Percival’s criterion of comfortable binocular vision is fulfilled. If it is not, appropriate prisms, spherical lenses or visual training can be used to shift the demand point within the zone of comfort. In this criterion, no reference is made to the actual phoria of the subject and for this reason it has been criticized by several authors. Syn. middle third technique.
See convergence, relative; zone of clear, single, binocular vision.
criterion, Rayleigh Observation first made by Rayleigh that the images of two point objects will be resolved when the central maximum in the diffraction pattern of one image coincides with the first minimum of the diffraction pattern of the other image. For a perfect eye, with a 2 mm pupil, this criterion corresponds to a theoretical tolerance in focusing equal to about 0.075 D.
See disc, Airy’s; diffraction; resolution, limit of .
criterion, Sheard Rule proposed by Sheard to establish whether a patient is going to experience discomfort in binocular vision. It states that the amount of heterophoria should be less than half the opposing fusional convergence in reserve. If the criterion is not met, appropriate prisms, spherical lenses or visual training can be used. If a patient has 10 Δ of exophoria, the positive fusional vergence should be at least 20 Δ to satisfy this criterion.
See convergence, relative; zone of clear, single, binocular vision.
critical angle See angle, critical.
critical fusion frequency See frequency, critical fusion.
critical oxygen requirement See oxygen requirement, critical.
critical period See period, critical.
crocodile shagreen; tears See under the nouns.
Crohn’s disease See disease, Crohn’s.
cromolyn sodium See mast cell stabilizers.
cross-cylinder lens See lens, cross-cylinder.
cross-cylinder test for astigmatism See , cross-cylinder.
cross-fixation A condition often found in infantile, large-angle esotropia in which the eyes tend to stay adducted so that the right eye fixates objects in the left field of gaze and the left eye fixates objects in the right field of gaze.
See strabismus, infantile.
cross, Maddox See Maddox cross.
crossed cylinder, obliquely Two cylindrical lenses combined together with their axes neither parallel nor perpendicular. The combination can be replaced by a single sphero-cylindrical lens in which the two focal lines are perpendicular to each other. The powers and axis of this new lens can be determined graphically or mathematically. An analogous situation obtains when the cylindrical correction of an eye is corrected by a cylindrical lens placed at an incorrect axis before the eye.
crossed disparity See , disparity, crossed.
crossed eyes See strabismus, convergent.
crowding phenomenon See phenomenon, crowding.
crown glass See glass, crown .
crutch, ptosis See ptosis.
cryopexy See retinal break.
cryotherapy Method of treating a disease by the use of cold as a destructive medium. It may be used in the treatment of retinal detachment and breaks, conjunctival melanomas, lid tumours, uveitis, distichiasis and trichiasis.
cryptophthalmia A very rare congenital defect in which the skin of the eyelids is continuous over the eyeball, resulting in an absence of palpebral fissure. Eyelashes may or may not be present. The cornea is fused with the overlying skin into one structure. Note: also spelt cryptophthalmos or cryptophthalmus.
crypts of Fuchs See crypts of Fuchs.
crypts of Henle See glands of Henle.
crystal, anisotropic A crystal that exhibits birefringence (double refraction).
crystal, dichroic A birefringent crystal which absorbs the ordinary and extraordinary rays unequally. Natural light passing through a plate of a dichroic material becomes partially or totally polarized.
See birefringence; dichroism.
crystal, isotropic A crystal which has the same optical properties in all directions.
crystal, tourmaline See polarizer.
crystalline lens See lens, crystalline.
crystalline lens, equator of the See equator of the crystalline lens.
cues, monocular See perception, depth.
cul-de-sac See conjunctiva.
cup-disc ratio See ratio, cup–disc.
cup, glaucomatous A large and deep excavation within the optic disc due to a raised intraocular pressure. It is characterized by overhanging walls over which the blood vessels bend sharply and reappear at the bottom of the depression.
See disc, cupped; ratio, cup–disc.
cup, ocular; ophthalmic See cup, optic.
cup, optic 1. A double layered cup-shaped structure attached to the forebrain of the embryo by means of a hollow stalk. It develops into the retina and inner layers of the ciliary body and iris. It is formed by the invagination of the outer wall of the optic vesicle. Subsequently, nerve cells develop in its invaginated layer and some of these send their axons back along the hollow stalk (optic stalk or lens stalk) to form the optic nerve. Syn. ocular cup; ophthalmic cup; secondary optic vesicle. 2. Synonym for physiological cup.
See anophthalmia; ectoderm; fissure, optic; vesicle, optic.
cup, physiological A funnel-shaped depression at or near the centre of the optic disc through which pass the central retinal vessels. Syn. optic cup (although it would be preferable not to use this synonym since this term has another meaning); physiological excavation.
See disc, cupped; neuroretinal rim.
curettage See chalazion.
curl side See side; side, curl.
curvature ametropia See ametropia, refractive.
curvature of field Aberration of an optical system due to the obliquity of the incident rays of light relative to the optical axis. The image corresponding to a plane object lies on a curved surface. This aberration does not usually affect the eye, as the retina is itself curved.
See Petzval surface.
curvature of a surface A measure of the shape of a curved surface. It is expressed in a unit called reciprocal metre, usually written as m–1, which is equal to the reciprocal of the radius of curvature of a surface in metres. Example: if a surface has a radius of curvature r of +0.5 m, its curvature R will be R = 1/r = 1/+0.5 = 2 m–1.
curve, base (BC) 1. The shallower principal meridian of a toroidal surface of a toric lens. The other meridian of the toroidal surface which has the maximum power is called the cross curve. 2. In a meniscus lens, the shallower of the two surfaces. 3. Of a range of lenses of different powers, a surface power common to all the lenses in that range.
See lens, periscopic; optic zone radius, back.
cyanolabe See pigment, visual.
cyanophobia An abnormal aversion to blue. See chromatophobia.
cyanopsia See chromatopsia.
cycle, citric acid See cycle, Krebs.
cycle per degree Unit of spatial frequency. It is equal to the number of cycles of a grating (one dark and one light band) that subtends an angle of one degree at the eye. Abbreviated: c/deg; cpd. This unit was developed because there is no finite width in a bar of a sine grating.
cycle, Krebs A series of reactions in which the intermediate products of carbohydrate, fat and protein metabolism are converted to carbon dioxide and hydrogen atoms (electrons and hydrogen ions). This cycle can only operate in the presence of oxygen. Further oxidation yields carbon dioxide, water and ATP. This cycle occurs in the mitochondria that are found in the cytoplasm of cells of living organisms. It forms one of the processes in the metabolism of glucose providing energy (stored in ATP) to maintain the vital functions of the cells (e.g. mitosis). This cycle represents the principal energy pathway of the corneal endothelium. Syn. citric acid cycle; tricarboxylic acid cycle.
See mitosis.
Table C9
Relationship between the minimum angle of resolution, the Snellen fraction and the equivalent spatial frequency of a sine wave
| Snellen fraction | |||
| resolution (min of arc) | (m) | (ft) | Spatial frequency (cpd) |
| 0.5 | 6/3 | 20/10 | 60 |
| 0.6 | 6/3.6 | 20/12 | 50 |
| 0.75 | 6/4.5 | 20/15 | 40 |
| 1.0 | 6/6 | 20/20 | 30 |
| 1.25 | 6/7.5 | 20/25 | 24 |
| 1.5 | 6/9 | 20/30 | 20 |
| 2.0 | 6/12 | 20/40 | 15 |
| 2.5 | 6/15 | 20/50 | 12 |
| 4.0 | 6/24 | 20/80 | 7.5 |
| 5.0 | 6/30 | 20/100 | 6 |
| 8.0 | 6/48 | 20/160 | 3.8 |
| 10.0 | 6/60 | 20/200 | 3 |
| 20.0 | 6/120 | 20/400 | 1.5 |
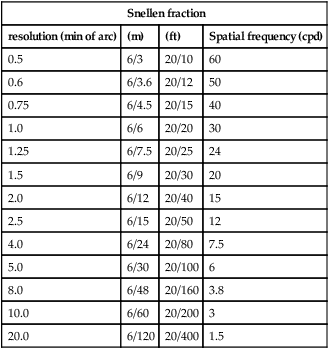
cycle, tricarboxylic acid See cycle, Krebs.
cyclic heterotropia; strabismus See strabismus, cyclic.
cyclitis Chronic or acute inflammation of the ciliary body frequently associated with iritis and choroiditis.
See cataract, complicated; syndrome, Fuchs’; uveitis, intermediate.
cyclodialysis Disinsertion of the ciliary body from the scleral spur which may produce a cyclodialysis cleft resulting in hypotony. It is performed occasionally in the treatment of glaucoma to reduce the intraocular pressure, as it forms a communication between the anterior chamber and the suprachoroidal space. It may also occur as a result of trauma or intraocular surgery (e.g. trabeculectomy).
See angle, recession; pathway, uveoscleral.
cyclodiode laser therapy A surgical procedure aimed at lowering intraocular pressure by decreasing aqueous secretion by means of small burns of the ciliary body with pulses of laser energy passed through the eye.
cycloduction Rotation of an eye around its anteroposterior axis. Syn. cyclorotation; cyclotorsion.
See torsion.
cyclofusion Rotation of the eyes about their anteroposterior axes in an attempt to align the two views of the visual field so as to stimulate corresponding retinal areas, in response to an appropriate stimulus.
cycloparesis A weakness of the ciliary muscle.
cyclopean eye See eye, cyclopean.
cyclopentolate hydrochloride An antimuscarinic (or parasympatholytic) drug used as a short duration mydriatic and cycloplegic. Common concentrations are 0.5% and 1.0% as cycloplegic and 0.1% as mydriatic.
See acetylcholine; cycloplegia; mydriasis.
cyclophoria When binocular vision is dissociated (i.e. when stimuli to fusion are eliminated) one eye or both rotate about its/their respective anteroposterior axes to take up the passive position. If the upper portion of the eye rotates inward, it is called incyclophoria and if it rotates outward, it is called excyclophoria. It is usually caused by an anomaly of the oblique muscles. Cyclophoria is commonly associated with hyperphoria. There are various methods which can be used to detect cyclophoria: the Maddox rod test; the double prism test; the synoptophore with appropriate slides; the fixation disparity unit; Fresnel’s bi-prism. Syn. periphoria.
See cyclotropia; test, double prism; test, Maddox rod.
cyclophosphamide See immunosuppressants.
cycloplegia Paralysis of the ciliary muscle resulting in a loss of accommodation. It is usually accompanied by dilatation of the pupil.
See acetylcholine; anisocycloplegia; hyperopia, latent; mydriatic.
cycloplegic 1. Pertaining to cycloplegia. 2. A drug which produces cycloplegia. Cycloplegic drugs, which act by inhibiting the action of acetylcholine at muscarinic receptors in the ciliary muscle, include atropine, cyclopentolate hydrochloride, homatropine hydrobromide, hyoscine hydrobromide (scopolamine hydrobromide) and tropicamide. Syn. anticholinergic; antimuscarinic; cholinergic antagonist; cholinergic blocking agent; parasympatholytic.
See mydriatic.
cycloplegic refraction See refraction, cycloplegic.
cyclorotation Rotation of an eye about an anteroposterior axis. Syn. cyclotorsion.
cyclosporine See ciclosporin.
cyclotonic A state of constant accommodation. See tonus.
cyclotropia Type of strabismus in which there is a deviation around the anteroposterior axis of one eye (or both eyes) relative to the vertical meridian.
See cyclophoria.
cycloversion Rotation of both eyes in the same direction, around their respective anteroposterior axes.
See dextrocycloversion; laevocycloversion.
cylinder axis See axis, cylinder.
cylinder lens, cross- See lens, cross-cylinder.
cylindrical error See prescription.
cylindrical lens See lens, astigmatic.
cyst, dermoid A tumour containing keratin, sebum, fibrous tissue, hair or fat globules which may be found in the cornea, interior of the eye, or in the subcutaneous tissue of the superotemporal orbital rim. It presents as a round mass, about 1 to 2 cm in diameter, pink to yellow in colour. Limbal dermoids may be associated with Goldenhar’s syndrome. There may be induced astigmatism. If vision is impaired or it is cosmetically disfiguring, treatment is by excision.
cyst, macular See macular cyst.
cyst, meibomian See chalazion.
cystoid macular oedema See oedema, cystoid macular.
cytoid bodies See bodies, cytoid.
cytology A study of cells to detect diseases. The usual procedure is to obtain a sample, to fix it on a glass slide, treat it with various dyes and inspect it under a microscope. Differential staining allows identification of the cells and their state of health.
cytology, impression A simple, non-invasive means of studying cells on the conjunctiva. It is carried out by pressing a small piece of special filter paper against the anaesthetized bulbar conjunctiva for a few seconds, after which it is removed. The operation is usually repeated two or three times over the same area. The filter paper is then fixed to a glass slide, stained and examined under a microscope. Mucin, goblet cells and many epithelial cells which stain in different colours, depending on the dyes used, can be assessed and facilitate the diagnosis of many external eye diseases, such as keratoconjunctivitis sicca and xerophthalmia.
See Gram stain.
cytomegalovirus retinitis See retinitis, cytomegalovirus; syndrome, acquired immunodeficiency.






