23 Buttocks
Summary and Key Features
• The gluteal region is an important component of body beauty
• There is an increasing search for techniques and products to enhance body shape and contours
• Autologous fat is abundant, easily collected, and promotes long-lasting results
• The donor area is chosen to contribute also to the final aspect of the buttocks: while liposuction models its shape, lipotransfer improves its projection
• The best areas to augment firmness and volume are the two upper quarters of the buttocks; the amount of fat tissue used is around 100–200 mL per side
• The hyaluronic acid used for body contouring is a large-particle gel called Macrolane VRF (Volume Restoration Factor)
• Indications include: correction of concave body deformities, trauma scars, and for shaping and augmentation of body areas, like calves, buttocks, chest, and breasts
• Advantages are the known safety record of NASHA™ (non-animal stabilized hyaluronic acid) products, no requirement of donor site, little downtime, reversibility, and performance on an outpatient basis
• The main disadvantage is cost when large amounts of the product are needed
Aesthetic characteristics of the buttocks
The shape of the buttocks is determined by anatomical structures such as the underlying bone component, gluteus maximus muscle, adipose tissue, and skin. Their combination and interaction give individuals their characteristic buttock shape. According to ethnic ideals, some characteristics of the gluteal region should be preserved, recreated, or corrected in order to enable a harmonious result in relation to the rest of the body. They are described here and summarized in Box 23.1.
 Lateral depressions: formed on each buttock at the greater trochanter by the medius gluteus, external vastus, gluteus maximus, and quadratus femoris muscle insertions.
Lateral depressions: formed on each buttock at the greater trochanter by the medius gluteus, external vastus, gluteus maximus, and quadratus femoris muscle insertions.
 Infragluteal fold: formed superiorly by the inferior border of the gluteus maximus and inferiorly by the insertion of the semitendinosus and biceps femoris muscles in the ischial tuberosity. This fold’s length and shape has a pre-eminent role in gluteal aesthetics: a long fold indicates a ptotic buttock, whereas a short one suggests a young buttock.
Infragluteal fold: formed superiorly by the inferior border of the gluteus maximus and inferiorly by the insertion of the semitendinosus and biceps femoris muscles in the ischial tuberosity. This fold’s length and shape has a pre-eminent role in gluteal aesthetics: a long fold indicates a ptotic buttock, whereas a short one suggests a young buttock.
 Supragluteal fossettes: depressions at each side of the sacral region formed by the confluence of the upper portion of the posterior iliac spine, the lumbosacral aponeurosis, and the gluteus maximus.
Supragluteal fossettes: depressions at each side of the sacral region formed by the confluence of the upper portion of the posterior iliac spine, the lumbosacral aponeurosis, and the gluteus maximus.
 Triangle or V-shaped fold: formed superiorly by the supragluteal fossettes and inferiorly by the insertion of the gluteus maximus and coccyx.
Triangle or V-shaped fold: formed superiorly by the supragluteal fossettes and inferiorly by the insertion of the gluteus maximus and coccyx.
 Smooth waist-to-lumbar inward curve: with aging, women tend to develop a more centralized fat distribution with accumulation of subcutaneous adipose tissue at the waist, losing the smooth inward sweep of the lumbosacral area and waist, as described by Roberts and colleagues.
Smooth waist-to-lumbar inward curve: with aging, women tend to develop a more centralized fat distribution with accumulation of subcutaneous adipose tissue at the waist, losing the smooth inward sweep of the lumbosacral area and waist, as described by Roberts and colleagues.
Gluteal augmentation with fat grafting
Fat may be obtained as a single process associated with regional or circumferential liposculpture, or combined with other procedures such as lipectomies. Table 23.1 describes the tumescent solution used for gluteal augmentation. Fat extraction is performed using 3–4 mm blunt-tipped cannulas to avoid the destruction of the adipocyte, with continuous negative aspiration at 0.5 atmospheres of pressure, collected in a sealed vial. For minor procedures 10, 20, or 60 mL syringes may be used.
| 0.9% Saline solution | 1000 mL |
| 2% Lidocaine | 25 mL |
| 1/1000 Ephinephrine | 1 mL |
| 8.4% Sodium bicarbonate | 12.5 mL |
Correction of gluteal depressions with hyaluronic acid gels
Technical aspects
The areas to be treated are marked beforehand with the individual in a standing position. When the patient has been positioned, cleaned, and the incision sites covered with sterilized tissue, these are anesthetized using a 30 G needle. Since the passage of a blunt cannula through fat tissue is not a painful procedure, and in order not to distort the depressions, we use a minimal amount of anesthetic solution, as described in Table 23.2. Only the entry points are infiltrated and extra solution will be added solely to painful adherent locations. An average of two incision sites is planned per side, which are chosen in order to allow the cannula to reach the entire treatment area.
Table 23.2 Anesthetic solution used for Macrolane injections
| 0.9% Unpreserved saline solution | 180 mL |
| 2% Lidocaine | 10 mL |
| epinephrine concentration | 1 mg/mL |
| Epinephrine | 0.4 mL |
| 8.4% Sodium bicarbonate | 10 mL |
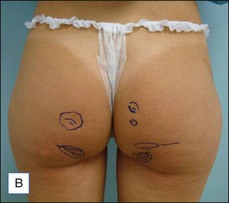
After 1 month, if the final aesthetic correction proves suboptimal, touch-up injections may be planned. Figures 23.1 and 23.2 illustrate two treated cases.
Conclusion
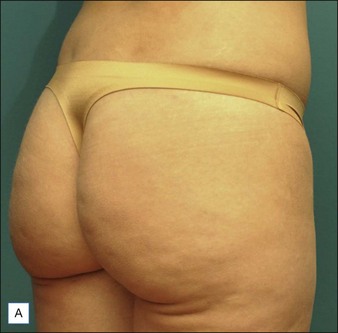
Figure 23.3 shows a 38-year-old woman who underwent liposuction and fat grafting in different layers of the buttocks: intramuscular, and between the deep fat tissue. Fat graft was mixed with growth factors. She also received superficial fat injections in banana folds. Part A shows the preoperative condition. B is postoperative, 4 months after the procedure.
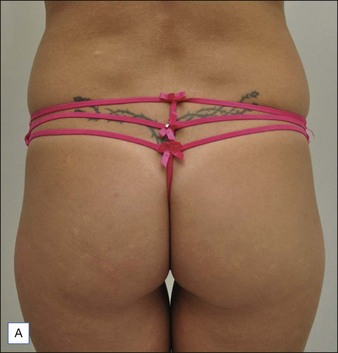
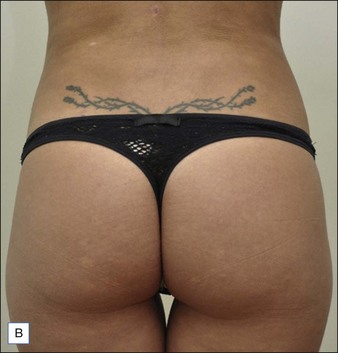
Figure 23.4 shows a woman, 36 years old, who underwent liposuction of the flanks, and a fat-grafting procedure. The fat graft was mixed with growth factors, and injected in several layers, obtaining an improvement in the shape and also in the volume of the buttocks. Part A shows the preoperative condition. B is postoperative, 3 months after the procedure.
Altman AM, Abdul Khalek FJ, Seidensticker M, et al. Human tissue-resident stem cells combined with hyaluronic acid gel provide fibrovascular-integrated soft-tissue augmentation in a murine photoaged skin model. Plastic and Reconstructive Surgery. 2010;125:63.
Centeno RF, Young VL. Clinical anatomy in aesthetic gluteal body contouring surgery. Clinical Plastic Surgery. 2006;33(3):347–358.
Cuenca-Guerra R, Lugo-Beltran I. Beautiful buttocks: characteristics and surgical techniques. Clinical Plastic Surgery. 2006;33(3):321–332.
DeLorenzi C, Weinberg M, Solish N, et al. The long-term efficacy and safety of a subcutaneously injected large-particle stabilized hyaluronic acid-based gel of nonanimal origin in esthetic facial contouring. Dermatologic Surgery. 2009;35:313–321.
Gonzalez R. Augmentation gluteoplasty: the XYZ method. Aesthetic Plastic Surgery. 2004;28:417–425.
Hedén P, Sellman G, Von Wachenfeldt M, et al. Body shaping and volume restoration: the role of hyaluronic acid. Aesthetic Plastic Surgery. 2009;33:274–282.
Hedén P, Olenius M, Tengvar M. Macrolane for breast enhancement: 12-month follow-up. Plastic and Reconstructive Surgery. 2011;127:850–860.
Macrolane 2008 Q-Med AB, Uppsala, Sweden [package insert]
McCleave MJ. Is breast augmentation using hyaluronic acid safe? Aesthetic Plastic Surgery. 2010;34:65–68.
Mendieta CG. Classification system for gluteal evaluation. Clinical Plastic Surgery. 2006;33(3):333–346.
Nicareta B, Pereira LH, Sterodimas A, et al. Autologous gluteal lipograft. Aesthetic Plastic Surgery. 2011;35:216–224.
Roberts TL, 3rd., Weinfeld AB, Bruner TV, et al. ‘Universal’ and ethnic ideals of beautiful buttocks are best obtained by autologous micro fat grafting and liposuction. Clinical Plastic Surgery. 2006;33(3):371–394.
Ullmann Y, Shoshani O, Fodor A, et al. Searching for the favorable donor site for fat injection: in vivo study using the nude mice model. Dermatologic Surgery. 2005;31(10):1304–1307.