Chapter 9 Burns
PATHOPHYSIOLOGY
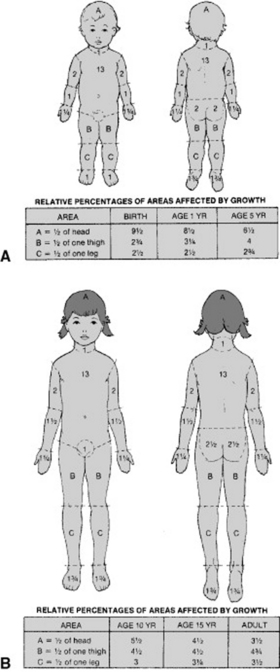
Burns are the tissue damage that results from contact with thermal, chemical, electrical, or radiation agents. Thermal burns are the most common type of injury. A thermal burn occurs when the skin is damaged by heat. Tissue under the skin may also be damaged. Chemical burns occur upon contact with acid, alkali, or organic compounds. Electrical burns occur upon contact with high- or low-voltage electricity. In children, this contact is most often with electrical cords. Radiation burns are least common and are infrequent in children. Burn severity is determined by (1) the depth of burn injury, (2) percentage of body surface area affected, and (3) involvement of specific body parts. See Box 9-1 and Figure 9-1 for descriptions of burn severity and depth.
The severity of the burn determines the degree of change seen in the body’s organs and systems. A thermal injury creates an open wound as a result of destruction of the skin. Following the burn, skin perfusion is decreased as blood vessels are occluded and vasoconstriction occurs. Intravascular volume decreases as fluids are leaked from the intravascular to the interstitial space as a result of increased capillary permeability. Pulmonary injury may occur as a result of inhalation of smoke, steam, or irritants. With a major burn, cardiac output decreases and blood flow to the liver, kidney, and gastrointestinal tract is compromised. The child with a major burn is in a hypermetabolic state, consuming oxygen and calories at a rapid rate. Prognosis is dependent on the severity of the burn.
INCIDENCE
1. Burns are the second leading cause of accidental injury and death in children younger than 14 years of age.
2. Children account for 35% of all burn injuries.
3. Mortality from burns is 2500 children annually; 10,000 experience severe permanent disability.
4. Toddlers account for 85% of children with burn injuries.
5. Burns caused by scalds are the most common and usually occur in the kitchen or the bathroom.
6. Electrical and chemical burns are common in the toddler age group.
CLINICAL MANIFESTATIONS
The following are initial manifestations of second to third degree burns over more than 20% of the body surface area:
LABORATORY AND DIAGNOSTIC TESTS
1. Complete blood count—decreased
2. Arterial blood gas values—metabolic acidosis (decreased pH, increased partial pressure of carbon dioxide [PCO2], and decreased partial pressure of oxygen [PO2])
3. Serum electrolyte levels—decreased because of loss to traumatized areas and interstitial spaces
4. Serum glucose level—increased because of stress-invoked glycogen breakdown or glyconeogenesis
5. Blood urea nitrogen level—increased because of tissue breakdown and oliguria
6. Creatinine clearance—increased because of tissue breakdown and oliguria
7. Serum protein levels—decreased because of protein breakdown for massive energy needs
MEDICAL MANAGEMENT
Burn treatment is based on the size and severity of the burn along with consideration as to its cause. Burn care can be divided into three phases: emergent, acute, and rehabilitative. Emergent care occurs for the first 72 hours of injury. Fluid resuscitation is critical in remedying intravascular fluid losses. Inadequate correction during this time may result in inadequate regional blood flow to the skin, the kidney, the gastrointestinal tract, the heart, and the brain, in that order. Oxygen is delivered by mask or artificial ventilation. The acute phase accounts for the majority of time the patient spends in the hospital. Care is focused on wound care, pain management, infection prevention, nutritional support, and psychosocial support. The burn itself may be covered with either moist or dry sterile dressings. Addition of topical antimicrobial medications such as silver sulfadiazine, mafenide acetate, bacitracin, gentamicin, or mupirocin may also be indicated. The child will receive analgesics or narcotics for pain. The rehabilitative phase lasts from complete wound healing to scar maturation. Depending on the severity of the burn, this may include reconstructive procedures, contracture releases, and reintegration into family, school, and social life.
NURSING INTERVENTIONS
First Aid and Emergency Care
1. Scald burn—stop burning process; remove individual’s clothing and jewelry; apply moist or dry sterile dressing.
2. Flame burn—have individual drop and roll to extinguish; remove nonadherent clothing; apply moist or dry sterile dressing.
3. Chemical burn—flush eyes and skin for 20 minutes with water.
4. Electrical burn—turn off power sources; initiate cardiopulmonary resuscitation.
Hospital Care
2. Monitor child for signs and symptoms of hypovolemic shock.
3. Monitor child for signs and symptoms of electrolyte imbalances (Box 9-2).
4. Monitor child for signs and symptoms of hemorrhage.
5. Provide pain relief measures to alleviate or control child’s pain (see Appendix I).
6. Protect child from potential infections.
7. Promote adequate nutritional intake to counteract nitrogen loss and potential gastrointestinal complications.
8. Promote optimal healing of wounds (see Medical Management section in this chapter).
9. Promote maximal function of joints.
10. Encourage verbalization of feelings regarding altered body image.
11. Provide for child’s developmental needs during hospitalization.