BURNS
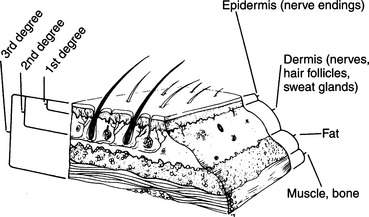
DEFINITIONS (Figure 93)
First-degree burn. This is a burn that involves the outermost layer of skin, the epidermis. It is often quite painful. The skin is reddened, but there is no blister formation. When a large surface area is involved, as with an extensive sunburn, the victim may become quite ill, with fever, weakness, chills, and vomiting.
Second-degree burn. This is a burn that involves the epidermis and portions of the next-deeper layer of the skin, called the dermis, which contains the sweat glands, hair follicles, and small blood vessels. It is usually more painful than a first-degree burn, and blisters are present. Large areas of second-degree injury impair the body’s ability to control temperature and retain moisture. Thus, a severely burned victim loses large amounts of fluid and can rapidly become hypothermic in a cold environment.
Third-degree burn. This is a burn that has penetrated the entire thickness of the skin, and may involve muscle, bone, and so on. It is typically painless because of nerve destruction. The appearance is dry, hard, leathery, and charred. Occasionally, the skin will appear waxy and white with small clotted blood vessels visible as purple or maroon lines below the surface. Because a third-degree burn is usually surrounded by an area of second-degree injury, the edges of the wound may be quite painful. Third-degree burns nearly always require a skin graft for coverage.
Partial-thickness burn. First-degree or second-degree burn.
Full-thickness burn. Third-degree burn.
Inhalation injury. This is a burn that involves any portion of the airway. Inhalation injury occurs when a victim is trapped in a fire and inhales smoke, steam, or superheated air (see page 114).
TREATMENT FOR BURNS
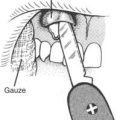
1. Remove the victim from the source of the burn. If his clothing is on fire, roll him on the ground or smother him in a blanket to extinguish the flames. Remove all materials that are hot or burned. If the victim has been burned with chemicals, gallons of water should be used to wash off the harmful agents. If chemicals may be present in an article of clothing, remove it. If the eyes are involved, they should be irrigated copiously. Phosphorus ignites on contact with air, so any phosphorus in contact with the skin must be kept covered with water. Do not attempt to neutralize acid burns with alkaline solutions or vice versa; the resultant chemical reaction may liberate heat and worsen the injury. Stick to irrigation with water. If clothing remains stuck to the skin and does not fall away with irrigation, do not tear the clothing away. Cut around it.
2. Evaluate the airway. Look for evidence of an inhalation injury: burns of the face and mouth, singed nasal hairs, soot in the mouth, swollen tongue, drooling and difficulty in swallowing saliva, muffled voice, coarse or difficult breathing, coughing, and wheezing. If it appears that an inhalation injury has occurred, administer oxygen (see page 431) by face mask at a flow rate of 5 to 10 liters per minute, and transport the victim to a hospital as quickly as possible.
3. Examine the victim for other injuries. Unless the airway is involved or the victim is horribly burned, the burn injury will not be immediately life threatening. In your eagerness to treat the burn, don’t overlook a serious injury such as a broken neck. Control all bleeding and attend to broken bones before applying burn dressings.
After the wound is clean and dry, cover it with a soft, bulky dressing made of gauze or cloth bandages, taking care to keep the dressing snug but not tight. If antiseptic cream such as silver sulfadiazine (Silvadene) is available, it should be applied under the dressing. Silver sulfadiazine should not be used on the face or in victims who are pregnant, infants, or nursing mothers with children younger than 2 months. An alternative is mupirocin ointment or cream, or bacitracin ointment. A nonadherent dressing layer directly over the antiseptic is easier to change than coarse gauze. Another excellent covering is Spenco 2nd Skin underneath an absorbent sterile dressing. Spenco 2nd Skin is an inert hydrogel composed of water and polyethylene oxide. It absorbs fluids (so long as it doesn’t dry out), which “wicks” serum and secretions away from the wound and promotes wound healing. Other occlusive hydrogel-type dressings are NU-GEL (preserved polyvinyl pyrrolidone in water) and Hydrogel, which can absorb up to 2 ½ times its weight in exuded (from the wound) fluids. Yet another covering for a burn is a layer of petrolatum-impregnated Aquaphor gauze under a dry (absorbent) gauze dressing.
A victim with large areas of second-degree burns may need to be treated for shock (see page 60).
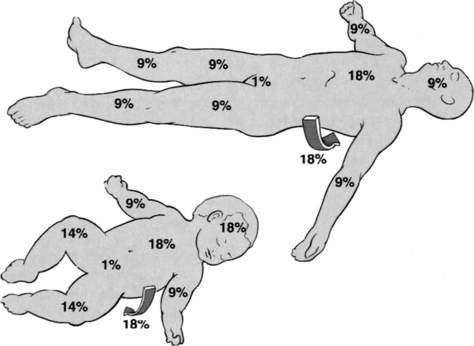
If a first-degree burn involves more than 20% of the body surface area and the victim suffers from fever, chills, or vomiting, a physician evaluation is required. If a second-degree burn involves a significant portion of the face, eyes, hands, feet, genitals, or an area greater than 5% of the total body surface area, a physician evaluation is required. Body surface area can be estimated using the “rule of nines” (Figure 94). For an adult, each upper limb equals 9% of total body surface area (TBSA), each lower limb equals 18%, the anterior and posterior trunk equal 18% each, the head and neck combined equal 9%, and the genital/groin area (perineum) equals 1%. For a small child, each upper limb equals 9% of TBSA, each lower limb equals 14%, the anterior and posterior trunk equal 18% each, the head and neck combined equal 18%, and the perineum equals 1%. Another method to estimate involved body surface area is the “palm of hand” rule: The surface area of the victim’s palm with the fingers represents approximately 1% to 1.5% of his TBSA. All third-degree burns are serious and should be seen by a physician.
Wet versus Dry Dressings
If the burn surface area is small (less than 10% of total body surface area), cool, moist dressings (not ice) may be used to initially cover the burn wound. These often provide greater pain relief than do dry dressings. If the surface area involved is large, however, dry, nonadherent dressings should be used, to avoid overcooling the victim and introducing hypothermia (see page 305). Because the skin is the major thermoregulatory organ of the body, it is difficult for an extensively burned victim to control his body temperature, so great care must be taken when wetting down such a person. If the victim begins to shiver, the cooling is too extreme.
Fluid Replacement
A person who has suffered an extensive burn will rapidly become dehydrated. Because water quickly shifts from the blood volume into the tissues of the body, the injured skin cannot retain moisture, and associated immune suppression leads to overwhelming infection and shock. Oral rehydration with balanced salt solutions is little help, but in the wilderness, it is usually the only option. Try to get the victim to drink—in sips, if necessary—enough liquid to keep the urine copious and clear (see page 208). If a burned victim cannot drink because his airway is injured, consciousness is altered, weakness prevails, or vomiting is persistent, immediately call for an evacuation.
BURN PREVENTION
1. Obey all posted warnings regarding campfires.
2. Use flame-resistant tents and sleeping bags.
3. Keep all campfires a sufficient distance (minimum 20 feet) from tents and other flammable materials. Create a clear, fuel-free perimeter of at least 3 feet around any campfire or grill. Do not sit too close to a campfire, particularly in windy conditions. Do not allow children to play near a campfire.
4. Do not add lighter fluid, gasoline, kerosene, or any other flammable liquid to a flaming fire or hot coals/embers.
5. Store flammable liquids in approved metal containers that are tightly sealed. Do not fill lamps and stoves with fuel anywhere near intense heat or open flames. Use a funnel to pour flammable liquids, and clean up any spills immediately.
6. Keep a bucket of water within easy reach of a campfire.
7. Thoroughly extinguish the campfire before going to sleep or leaving the campsite.
8. Do not handle camp sauna hot rocks or cook pots without wearing proper hand protection.
9. Do not allow children to handle containers with hot water.
10. Do not set containers of hot water or food on unstable or uneven surfaces.
11. Use battery-operated lights in or near tents or campers.