Chapter 20 Burns
Skin is the largest organ in the body, approximating 15% of body weight and 4.9 square metres in an adult. It has a number of functions, which correspond to the rationale of management and the potential complications of burns:
ASSESSMENT OF THE BURNS PATIENT
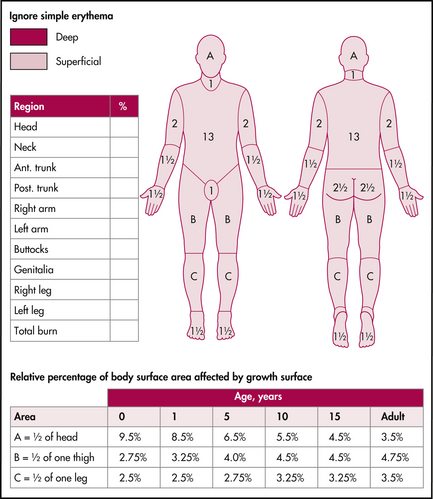
ASSESSMENT OF DEPTH AND EXTENT OF BURN
Depth of burn
The utilisation of terms such as first-, second- and third-degree has been largely replaced by:
Note: Superficial burns are not counted in assessing the extent of burn injury.
GENERAL MANAGEMENT
Analgesia
Superficial and partial thickness burns are extremely painful.
Simple oral analgesia may be required at home.
Inability to control pain is an indication for admission, particularly in children.
Other factors
Airway/lung injury/inhalation injury
This may be caused by carbon monoxide or toxic fumes such as cyanide. Supplemental oxygen is required for all but minor burns and in all patients in whom there is actual or suspected inhalation injury (include patients with no evidence of burn but where there has been a fire in an enclosed space). Intubation may be required early in patients with cyanosis, respiratory distress, stridor or hoarseness. Anticipate lung injury or swelling of the airway if facial burns are evident.
FLUID REQUIREMENTS
There are a number of formulae available. The recommended fluid replacement and maintenance from the NSW Health burns transfer document are reproduced in Box 20.1.
ADMISSION AND TRANSFER TO SPECIALISED BURNS UNIT
SPECIFIC BURNS
Chemical burns
Specific antidotes, if available, can be used after this initial treatment (see below, hydrofluoric acid).
The severity of chemical injury is related to a number of factors:
PREVENTION OF INFECTION
Dressings
In small, superficial partial thickness burns
Silver sulfadiazine (SSD) cream is generally not recommended for outpatient care as it may become a potential source of infection after 24–48 hours. Acticoat® is another silver-based product that has replaced SSD in many Australian burns units, but requires specialist application.
In deep partial thickness and full thickness burns
SPECIFIC OTHER FACTORS
Note: Eschar is a result of full thickness burn and is, therefore, insensate.
Flash burns. From arc welding are acute corneal burns that generally heal without sequelae within 24 hours. The onset of symptoms is delayed for several hours and they are extremely painful. Topical local anaesthetic may be required initially to examine the eye but should not be used as treatment. Most do not require antibiotic treatment but pilocarpine drops can reduce pain, as can reduction of eye movement by application of eye pads.
Any other concerns can always be discussed with local burns unit medical staff.
Glattner R. Highlights of the 12th Annual Scientific Assembly of the American Academy of Emergency Medicine. San Antonio, Texas, Feb 2006. Online. Available: http://www.medscape.com/viewarticle/528296_1.
NSW Severe Burn Injury Service. Burn transfer guidelines. NSW Department of Health;. August 2004. revised
Papini R. ABC of burns: management of burn injuries of various depths. BMJ. 2004;329:158-160.
Shukla P. Initial evaluation and management of the burn patient. emedicine. Feb 2008.
Singer A.J., Brebbia J., Soroff H.H. Management of local burn wounds in the ED. Am J Emerg Med. 2007;25(6):661-671.
Wood F., Stoner M. Spray on relief for burns. ATSE Focus. 137, May/June 2005.