101 Bronchiectasis
Salient features
Examination
• Comment on kyphoscoliosis if any
• Tell the examiner that you would like to know whether the bronchiectasis is long standing; if so, you would like to examine the abdomen for splenomegaly (amyloidosis).
In addition there may be signs of collapse, fibrosis or pneumonia.
Questions
Mention the causes of bronchiectasis
• Postpneumonic, measles, pertussis, TB
• Mechanical bronchial obstruction, as in TB, carcinoma, nodal compression
• Allergic bronchopulmonary aspergillosis
• Gammaglobulin deficiency, congenital, acquired
• Immotile cilia syndrome (Kartagener syndrome)
• Neuropathic disorders (namely Riley–Day syndrome, Chagas’ disease)
Advanced-level questions
How can CT assess bronchiectasis?
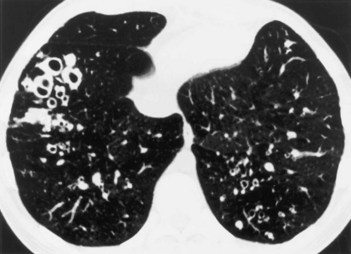
Specific abnormalities found on high-resolution CT (Fig. 101.1) include:
• dilatation of an airway lumen (rendering it >1.5 times as wide as a nearby vessel)
• lack of tapering of an airway toward the periphery
• varicose constrictions along airways
• ballooned cysts at the end of a bronchus (the bullae found in patients with emphysema have thinner walls and are away from an airway).
What are the major respiratory pathogens in bronchiectasis?
Staphylococcus aureus, Haemophilus influenzae, Pseudomonas aeruginosa.
How would you treat such patients?
• Identification of acute exacerbations and administration of antibiotics
• Suppression of the microbial load
• Treatment of underlying conditions
• Reduction of the excessive inflammatory response
• Promotion of bronchial hygiene:
• Control of bronchial haemorrhage
• Surgery in selected cases: surgical removal of extremely damaged segments or lobes that may be a nidus for infection or bleeding.
What abnormalities may be associated with bronchiectasis?
• Congenital absence of bronchial cartilage (Williams–Campbell syndrome)
• Tracheobronchomegaly (Mounier–Kuhn syndrome)
• Obstructive azoospermia and chronic sinopulmonary infection (Young syndrome), said to be caused by mercury intoxication. It was first described in the north of England by Young in 1970
• Situs inversus and paranasal sinusitis (Kartagener syndrome) (p. 117)
What do you know about Reid’s classification of bronchiectasis?
• Cylindrical bronchiectasis: bronchi that are uniformly dilated (to >2 mm but can be so large as to admit a finger) and do not taper but rather end abruptly; caused by plugging of smaller bronchi by thick mucus and casts
• Varicose bronchiectasis: dilated bronchi with irregular bulging contours similar to a varicose vein and no tapering; terminations are bulbous and bronchial subdivisions are reduced
• Cystic or saccular bronchiectasis is the most severe form and is characterized by sharply reduced bronchial subdivisions and dilated bronchi ending in cystic pus-filled cavities.
What are the modes of presentation of the bronchiectasis?
• Luminal blockage by a foreign body, broncholith or slowly growing beinign tumour
• Extrinsic narrowing caused by enlarged lymph nodes (e.g. in middle lobe syndrome, which involves a small angulated orifice surrounded by a collar of lymph nodes that may enlarge and encroach on the main airway after granulomatous disease caused by infection with mycobacteria or fungi
• Twisting or displacement of the airways after a lobar resection (e.g. the occasional cephalad displacement of a lower lobe after surgery for the resection of the upper lobe).