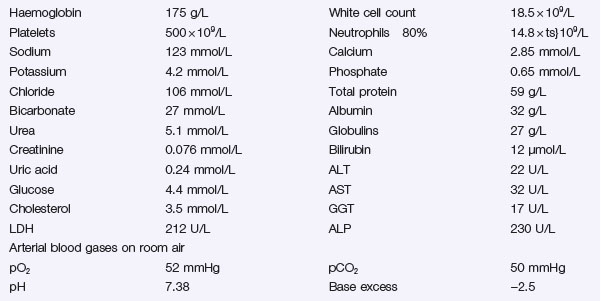
Problem 34 Breathlessness and weight loss in a 58-year-old man
Q.2
What are the possible diagnoses?
The man looks unwell and dyspnoeic and you decide to admit him to hospital for further management.
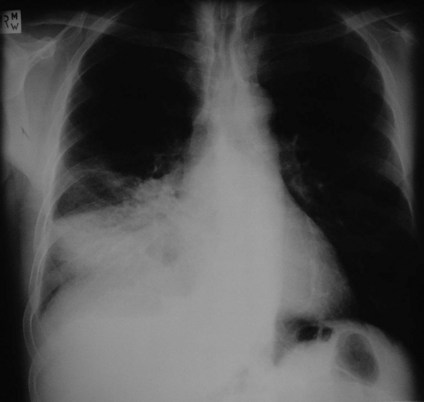
A further radiological investigation is performed. Two representative films are shown (Figures 34.2 and 34.3).
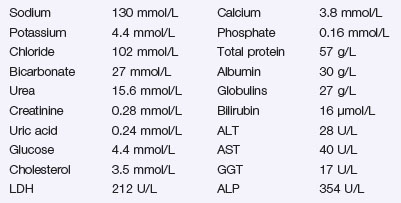
Some serum biochemistry had been performed earlier that day. The results are shown in Investigation 34.2.
Answers
On examination you should look for signs or evidence of the following:
In addition you should measure oxygen saturation via pulse oximetry and perform spirometry.
Anaemia may explain his shortness of breath, lethargy and, depending on the cause, his weight loss.
A.3 Perform these investigations:
A.5 The “chest X-ray” is reported as follows:
A.6 Once he is stabilized he will need:
A.7 The “CT scans” are reported as follows:
A.9 There are several possible causes for confusion in this man:
Revision Points
Lung Cancer
Epidemiology
Presentation
Treatment
Issues to Consider
, http://en.wikipedia.org/wiki/Non-small_cell_lung_carcinoma_staging. Summarizes the latest revision to the NSCLC staging system (January 2009)
, www.cancerresearchuk.org. Website of the Cancer Research Campaign in the UK with lots of information and links for lung and other tumours
, www.lungcancer.org. Excellent website with links and information for patients and healthcare professionals alike