Chapter 17 Breast Reduction
Summary
Introduction
History of development of different techniques
In the 1970s McKissock1 introduced the vertical bipedicle breast reduction technique, which was the first procedure for breast reduction surgery that was both reliable and reproducible. Before then:
When it was discovered that either of McKissock’s pedicles could be severed, the inferior pedicle with an inverted T skin resection pattern became the favored method.6–8 It has a reliable blood supply to the nipple and areolar complex and the skin flaps close easily over the pedicle. The skin brassiere was tightened to control the breast shape. Although most surgeons around the world now use an inferior pedicle alone for the nipple and the Wise skin resection pattern9 for the skin, some still prefer the vertical bipedicle of McKissock, especially for larger reductions.
Meanwhile, the South Americans10–13 and the Europeans14–18 developed expertise with a vertical skin resection pattern and a vertical wedge resection of parenchyma. These techniques were used mainly for small reductions, with an inverted T skin resection pattern used for the larger reductions. Many of these surgeons used the superior pedicle19 for the nipple-areolar complex rather than the inferior pedicle, even when they chose an inverted T skin resection pattern. Many European and South American surgeons continue to use a superior pedicle, but often combine it with a Wise skin resection pattern.
Principles behind the techniques
The three main problems with breast reduction are:
Maintaining the blood supply
The breast is a superficial ectodermal structure that develops from the fourth interspace and its blood supply is superficial,20 except for the perforator through the pectoralis muscle. The perforator:
The superficial arteries comprise:
The veins do not accompany the arteries and are found separately (and seen) just beneath the dermis.
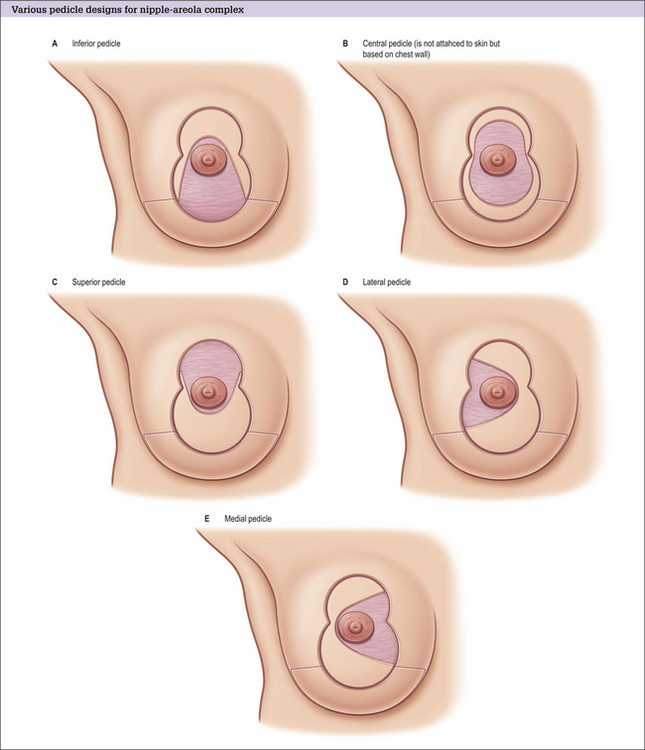
Types of pedicle
The blood supply of the different pedicles (Fig. 17.1A-E) is as follows:
Central pedicle
The central pedicle may not be quite as reliable as an inferior pedicle because there are many small but powerful blood vessels that enter the breast superficially from the level of the IMF. These are cut when a central pedicle is created. Creation of a central pedicle also severs the superficial veins, which supply most of the breast.
A central pedicle relies on the same arterial perforator and its venae comitantes as supply an inferior pedicle, and is therefore, by definition, full thickness.21,22
Free nipple grafts
Free nipple grafts are an important consideration especially if any of the other pedicles have an unpredictable blood supply,23,24 especially for the larger reductions. There is a loss of sensation, a loss of projection to the nipple, and a loss of breastfeeding potential. There is also a chance of irregular pigmentation.
Minimizing the risk of nipple necrosis
Although breast reduction is predictable and safe, there is a risk of complete nipple necrosis in around 1 in 300 patients. Some surgeons routinely use free nipple grafts, whereas many reserve these for the large reductions. The nipple is preserved with the Passot25 technique (or when a similar pedicle is used in a variation of the Robertson26 technique) where the complete inferior breast is used as a broad pedicle, and this is occasionally selected for extremely large reductions.
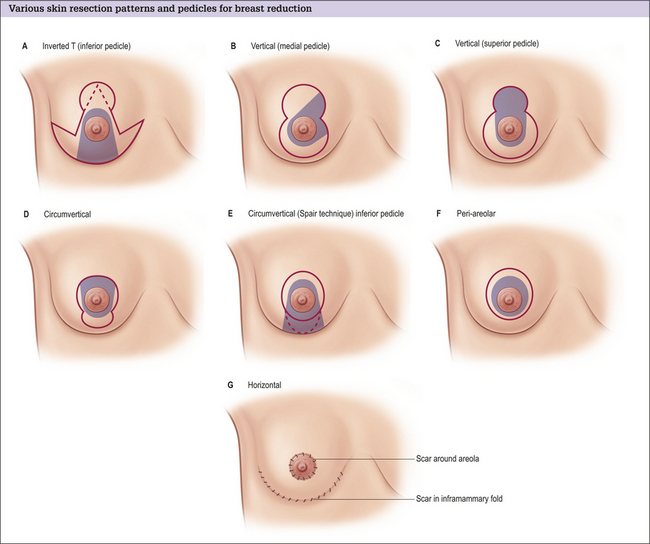
Skin resection pattern
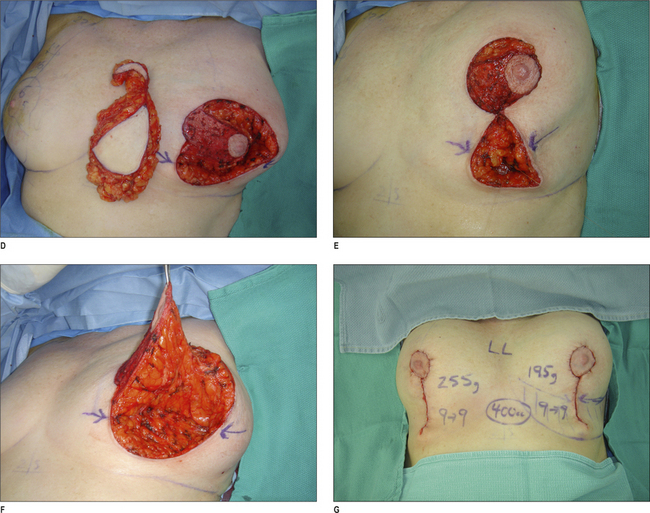
The skin resection pattern (Fig. 17.2A-G) is determined mainly by the amount and quality of the excess skin.
Approaches to minimize scarring and maximize breast shape
The aim of further reducing scars is evident in the techniques that attempt to confine the scar to the area around the areola. The periareolar method is best suited for small breast reductions and some mastopexies.35,36 These are difficult procedures with a long learning curve. Separation of the skin flaps from the parenchyma is an essential component to achieve a good outcome.
Unanswered questions
Many questions are still debated by surgeons and include:
Indications
Choice of breast reduction operation
The most common skin resection patterns are the inverted T and the vertical techniques.
Inverted T resection
The inverted T resection is used for larger reductions and for patients with a large excess of skin, especially when there is poor skin elasticity (e.g. in patients who have had a massive weight loss).40
Vertical approach
The second most common skin resection pattern is the vertical approach. The most common pedicles are the superior and the medially based pedicles. Both the lateral and the inferior (short scar peri-areolar inferior pedicle reduction [SPAIR]30) pedicles are also used. Some surgeons take up more skin into the areola and call the procedure the ‘circumvertical’ approach.41,42 This is done to shorten the vertical scar, but does require more finesse in closing the areola without puckering and stretching.
Other techniques
Periareolar technique
For very small breast reductions, the periareolar technique can be used. This is a commonly misunderstood technique because it does not just involve suturing the skin under tension to the areola, but also involves separation of the skin from the breast tissue. The breast tissue is reduced and reformed35 with sutures or it is wrapped in various forms of mesh.36
For very large breast reductions, variations of the Passot25 technique can be used. In these cases, the pedicle is a complete inferior pedicle from medial to lateral. The upper skin flap is brought down over the inferior tissue and a cutout is then created for the areola. The upper skin flap is much longer than the incision along the IMF and a considerable amount of gathering is needed. This procedure is some-times called the ‘no vertical scar technique’ because the scar is confined to the IMF and the periareolar areas. Pribaz43 has modified the Robertson technique as a variation for the extremely large reductions. Rubin40 has developed a variation that can restore some shape for patients who have had massive weight loss.
Liposuction-only breast reduction
Liposuction-only breast reduction44,45 is useful in women with fatty breasts, fairly high nipples and good upper pole fullness. Breasts tend to contain more fatty tissue than glandular tissue around meno-pause and these patients may be good candidates for liposuction only. Volume can be reduced, but a good shape can be best achieved in patients with high nipples and good upper pole fullness. Unfortunately many older women have developed ptosis and loss of upper pole volume. Large breasts in teenagers tend to be very glandular if they are normal body weight, and liposuction-only is not likely to be effective.
Medial pedicle vertical breast reduction vs inferior pedicle, inverted T reduction
Dog-ears
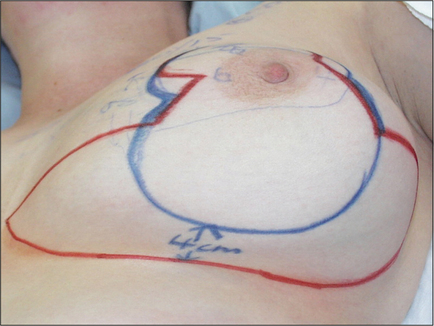
I prefer the medial pedicle vertical approach for most breast reductions. The resection pattern is a vertical ellipse or wedge resection (Fig. 17.3), which results in two dog-ears – one superiorly and one inferiorly:
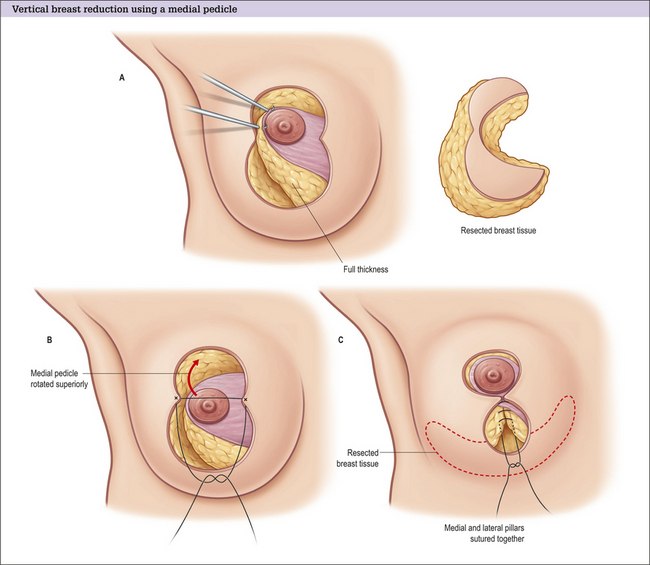
Medial Pedicle Vertical Breast Reduction
Operative Approach
Preoperative markings
1 Inframammary fold level
The first marking is the level of IMF. Some patients have high folds and some have very low folds.
4 Areolar opening
The areolar opening should end up as a circle when closed. A 16 cm circumference matches a 5 cm diameter and 14 cm matches a diameter of 4.5 cm.
6 Pedicle design
The medial pedicle is best designed keeping one half of the base in the areolar opening and one half of the base below the areolar opening (Fig. 17.4A). This design allows the pedicle to rotate easily into position and allows the inferior border of the medial pedicle to become the medial pillar. Too much tissue left below the areolar opening may contribute to the appearance of pseudoptosis. The base is usually 68 cm in length.
The blood supply comes from the medial branches of the internal mammary system.
Operative technique
Pedicle creation
Tissue resection
Pillar closure
Skin closure
Procedure completion
Postoperative Care
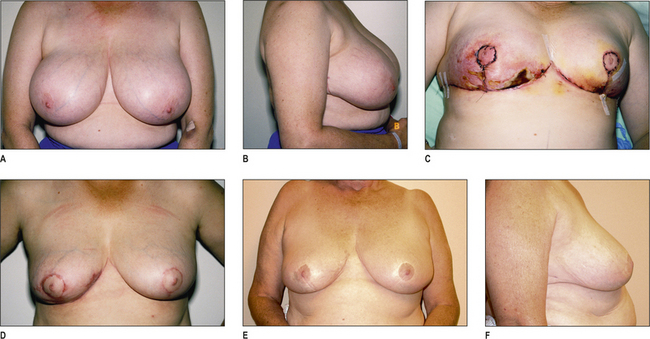
Pre and postoperative views for one patient are shown in Fig. 17.5A-L.
I have found that recovery time from a medial pedicle verticle breast reduction is about 2–4 weeks, which is about half that required for inverted T inferior pedicle reductions. Operating time is only about 2 hours and intraoperative blood loss is minimal.
Inverted T, Inferior Pedicle Breast Reduction
Operative Approach
Preoperative markings
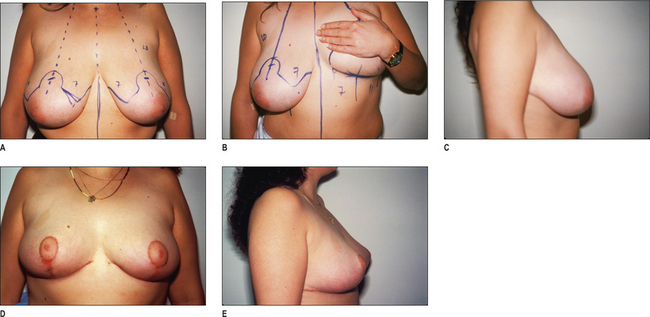
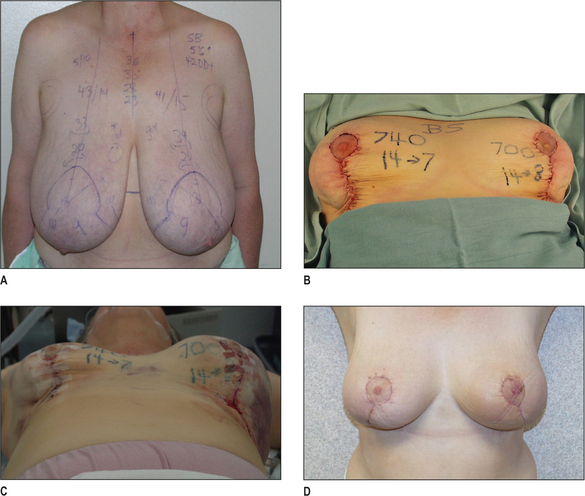
The markings (Fig. 17.6A-E) are all made preoperatively with the patient in the standing position. Some surgeons prefer to decide where to place the nipple during surgery, but I believe that a more accurate determination can be achieved preoperatively to avoid placing the nipple too high or on the concave upper surface of the breast. It is important to make sure that the markings are symmetrical for what is left behind, not for what is removed and to make them in the following sequence.
6 Pedicle design
Several surgeons believe that it may be important to try to cant the pedicle base laterally to some degree to include the deep branch of the lateral fourth intercostal nerve to preserve nipple sensation. It is probably more important, however, to leave tissue over the pectoralis muscle to preserve this nerve around the level of the fourth interspace.
Operative technique
Pedicle creation
Tissue resection
Flap closure
Postoperative Care
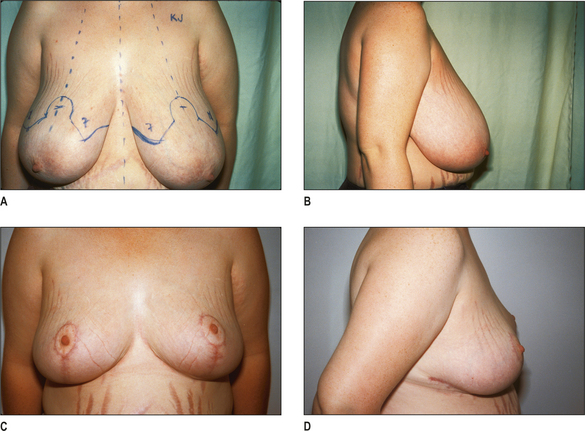
Pre and postoperative views for one patient are shown in Figs 17.7A-D.
Optimizing outcomes
Complications and Side Effects
Scarring, loss of sensation and potential inability to breastfeed are expected side effects:
Wound healing and infection
Wound healing problems (Figs 17.8A&B, 17.9A-F and 17.10A-D) are more likely in obese patients. Smoking also appears to have an adverse effect on wound healing. Perioperative antibiotics not only reduce the infection rate (which is more common in the larger patients), but also reduce wound healing problems. The breast ducts are contaminated with Staphylococcus epidermidis and proprionibacteria. It makes sense that some form of antibacterial pro-phylaxis may be indicated in breast surgery. It is not completely ‘clean’ surgery.
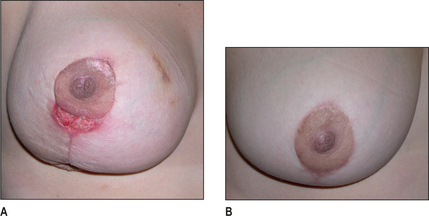
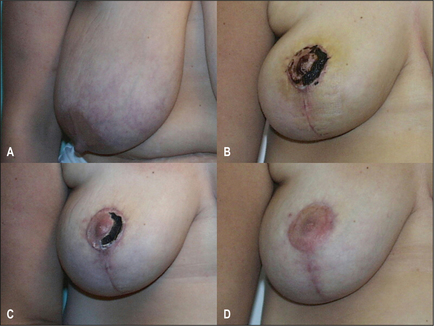
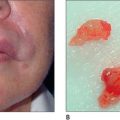
Nipple-areolar necrosis
Creation of a pedicle also involves a reduction of blood supply. The four main arterial inputs to the breast may not all be equally dominant. Nipple necrosis (Fig. 17.11A-D and see Fig. 17.10) can occur when one of these vessels is weak or there is constriction, kinking or compression of the pedicle obstructing venous return. External compression is unlikely to be strong enough to cause necrosis, but a hematoma could be a problem.
If a nipple and areola look congested, removal of sutures and release of compression are indicated.
Hematomas and seromas
Meticulous hemostasis can prevent the development of a hematoma (Fig. 17.12A-D), but drains cannot. If infiltration is used, the vessels may be constricted and the surgeon may not notice them. A careful search for known vessels is important before closure.
Asymmetry
Asymmetry can occur with any breast procedure. If it persists postoperatively it can often be treated with liposuction to the larger side. It is interesting that patients will tolerate asymmetry on the same side better than if the asymmetry is reversed postoperatively.
Puckers
Puckers (see Fig. 17.5G-L) occur with both the vertical and the inverted T procedures. The horizontal excision of skin and breast tissue with the inverted T results in a lateral dog-ear and a medial dog-ear. The lateral dog-ear is often difficult to correct without chasing it around the back. The medial dog-ear presents a particular problem because it is important not to let the scar cross the midline of the chest. It is often better to accept a small dog-ear medially rather than a hypertrophic scar across the midline.
Conclusion
There reasons for choosing different skin resection patterns and different pedicles differ. Some of these decisions are based on an estimated volume of reduction, previous surgery or biopsy scars, quality of the skin, or surgeon or patient preference. The best technique is the technique with which a surgeon is most comfortable with under the circumstances.
1. McKissock P.K. Reduction mammaplasty with a vertical dermal flap. Plast Reconstr Surg. 1972;49:245-252.
2. Biesenberger H. Eine neue methode der mammaplastik. Zentralbl Chir. 1928;2382:55.
3. Strombeck J.O. Mammaplasty: report of a new technique based on the two-pedicle procedure. Br J Plast Surg. 1960;13:79-90.
4. Dufourmentel C., Mouly R. Plastie mammaire par la methode oblique. Ann Chir Plast. 1961;6:45.
5. Skoog T. A technique of breast reduction – transposition of the nipple on a cutaneous vascular pedicle. Acta Chir Scand. 1963;126:453-465.
6. Robbins T.H. A reduction mammaplasty with the areola-nipple based on an inferior pedicle. Plast Reconstr Surg. 1977;59:64-67.
7. Courtiss E.H., Goldwyn R.M. Reduction mammaplasty by the inferior pedicle technique. An alternative to free nipple and areola grafting for severe macromastia or extreme ptosis. Plast Reconstr Surg. 1977;59:500.
8. Georgiade N.G., Serafin D., Morris R., et al. Reduction mammaplasty utilizing an inferior pedicle nipple-areolar flap. Ann Plast Surg. 1979;3:211.
9. Wise R.J. A preliminary report on a method of planning the mammaplasty. Plast Reconstr Surg. 1956;17:367.
10. Arie G. Una nueva tecnica de mastoplastia. Rev Iber Latino Am Cir Plast. 1957;3:28.
11. Pitanguay I. Surgical correction of breast hypertrophy. Br J Plast Surg. 1967;20:78.
12. Ribeiro L. A new technique for reduction mammaplasty. Plast Reconstr Surg. 1975;55:330.
13. Peixoto G. Reduction mammaplasty: a personal technique. Plast Reconstr Surg. 1980;65:217.
14. Lassus C. A technique for breast reduction. Int Surg. 1970;53:69.
15. Lassus C. A 30-year experience with vertical mammaplasty. Plast Reconstr Surg. 1996;97:373-380.
16. Marchac D., de Olarte G. Reduction mammaplasty and correction of ptosis with a short inframammary scar. Plast Reconstr Surg. 1982;69:45-55.
17. Lejour M., Abboud M., Declety A., et al. Reduction des cicatrices de plastie mammaire: de l’ancre courte a la verticale. Ann Chir Plast Esthet. 1990;35:369.
18. Lejour M., Abboud M. Vertical mammaplasty without inframammary scar and with breast liposuction. Perspect Plast Surg. 1996;4:67-90.
19. Wiener D.L., Aiache A.E., Silver L., et al. A single dermal pedicle for nipple transposition in subcutaneous mastectomy, reduction mammaplasty or mastopexy. Plast Reconstr Surg. 1973;51:115.
20. Palmer J.H., Taylor G.I. The vascular territories of the anterior chest wall. Br J Plast Surg. 1986;39:287-299.
21. Balch C.R. The central mound technique for reduction mammaplasty. Plast Reconstr Surg. 1981;67:305.
22. Hester T.R., Bostwick J., Miller L., Cunningham S.J. Breast reduction utilizing the maximally vascularized central breast pedicle. Plast Reconstr Surg. 1985;76:890.
23. Gradinger G.P. Reduction mammaplasty utilizing nipple-areola transplantation. Clin Plast Surg. 1988;15:641-654.
24. Gradinger G.P. Discussion: maximizing breast projection after free-nipple-graft reduction mammaplasty. Plast Reconstr Surg. 2001;107:961-964.
25. Passot R. La correction esthetique du prolapsus mammaire par la procede de la transposition du mamelon. Presse Med. 1925;33:317.
26. Robertson D.C. The technique of inferior flap mammaplasty. Plast Reconstr Surg. 1967;40:372.
27. Chiari A.J. The L Short Scar Mammaplasty: a new approach. Plast Reconstr Surg. 1992;90:233.
28. Lejour M. Vertical mammaplasty and liposuction of the breast. St Louis: Quality Medical Publishing, 1993.
29. Asplund O., Davies D.M. Vertical scar breast reduction with medial flap or glandular transposition of the nipple-areola. Br J Plast Surg. 1996;49:507-514.
30. Hammond D.C. Short scar periareolar inferior pedicle reduction (SPAIR) mammaplasty. Plast Reconstr Surg. 1999;103:890.
31. Hall-Findlay E.J. A simplified vertical reduction mammaplasty: shortening the learning curve. Plast Reconstr Surg. 1999;104:748.
32. Hall-Findlay E.J. Vertical breast reduction with a medially based pedicle. Operative strategies. Aesthetic Surg J. 2002;22(2):185-195.
33. Berthe J.-V., Massaut J., Greuse M., et al. The vertical mammaplasty: a reappraisal of the technique and its complications. Plast Reconstr Surg. 2003;111:2192-2199.
34. Spear S.L., Howard M.A. Evolution of the vertical reduction mammaplasty. Plast Reconstr Surg. 2003;112:855-868.
35. Benelli L. A new periareolar mammaplasty: The ‘round block’ technique. Aesthetic Plast Surg. 1990;14:93.
36. Sampaio-Goes J.C. Periareolar mammaplasty double skin technique. Breast Dis. 1991;4:111.
37. Schnur P.L., Schnur D.P., Petty P.M., et al. Reduction mammaplasty: an outcome study. Plast Reconstr Surg. 1997;100(4):875-883.
38. Blomqvist l., Eriksson A., Brandberg Y. Reduction mammaplasty provides long-term improvement in health status and quality of life. Plast Reconstr Surg. 2000;106(5):991-997.
39. Kerrigan C.L., Collins E.D., Striplin D., et al. The health burden of breast hypertrophy. Plast Reconstr Surg. 2001;108(6):1591-1599.
41. Mottura A. Circumvertical reduction mammaplasty. Aesthetic Surg J. 2000;20:199-204.
42. Graf R., Auersvald A., Bernardes A., et al. Reduction mammaplasty and mastopexy with shorter scar and better shape. Aesthetic Surg J. 2000;20:99-106.
44. Courtiss E.H. Reduction mammaplasty by suction alone. Plast Reconstr Surg. 1993;92:1276-1284.
45. Gray L.N. Liposuction breast reduction. Aesthetic Plast Surg. 1998;22:159.
46. Schwartzmann E. Beitrag zur Vermeidung von Mammillennekrose bei einzeitiger Mammaplastik schwerer Fälle. [Avoidance of nipple necrosis by preservation of corium in one-stage plastic surgery of the breast.]. Rev Chir Struct. 1937;7:206-209.
47. Schlenz I., Kuzbari R., Gruber H., et al. The sensitivity of the nipple-areola complex: an anatomic study. Plast Reconstr Surg. 2000;105:905-909.
48. Cruz-Korchin N., Korchin L. Breast-feeding after vertical mammaplasty with medial pedicle. Plast Reconstr Surg. 2004;114(4):890-894.