Chapter 29 Breast Disease: A Gynecologic Perspective
 Screening of the Breast in Asymptomatic Women
Screening of the Breast in Asymptomatic Women
 Diagnosis of Breast Lesions
Diagnosis of Breast Lesions
OPEN BREAST BIOPSY
Small masses may undergo excisional biopsy, whereas large masses should undergo incisional biopsy, or occasionally core-cutting needle biopsy. Absolute indications for open breast biopsy are listed in Box 29-1. Relative indications for breast biopsy include those women with a clinically benign mass but a positive family or personal history of breast cancer, a history of atypical hyperplasia, or an equivocal finding on mammography or cytology.
BOX 29-1 Absolute Indications for Open Breast Biopsy
 Common Benign Breast Disorders
Common Benign Breast Disorders
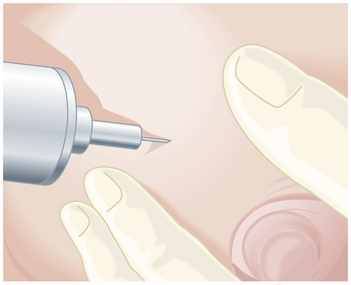
HYPERPLASIA
Treatment depends on the age of the patient, the severity of the symptoms, and the relative risk for the development of breast cancer. Women older than 25 years should undergo baseline mammography to exclude carcinoma. Cysts may be aspirated to relieve pain (Figure 29-1). If the fluid is clear and the lump disappears, careful follow-up only is indicated. Open biopsy is required if the fluid is bloody or if there is any residual mass following aspiration.
 Breast Cancer
Breast Cancer
ETIOLOGY
Established risk factors for breast cancer are shown in Table 29-1, but 75% of women develop the disease despite having no apparently increased susceptibility.
| Risk Factor | Relative Risk |
|---|---|
| Age (≥50 vs <50 yr) | 6.5 |
| Family history of breast cancer | |
| First-degree relative | 1.4-13.6 |
| Second-degree relative | 1.5-1.8 |
| Age at menarche (<12 vs ≥14 yr) | 1.2-1.5 |
| Age at menopause (≥55 vs <55 yr) | 1.5-2.0 |
| Age at first live birth (>30 vs <20 yr) | 1.3-2.2 |
| Benign breast disease | |
| Breast biopsy (any histologic finding) | 1.8-10.5 |
| Atypical hyperplasia | 4.0-4.4 |
| Hormone replacement therapy | 1.0-1.5 |
Data from Armstrong K, Eisen A, Weber B: Assessing the risk of breast cancer. N Engl J Med 342:564-571, 2000.
STAGING
Several systems of staging for cancer of the breast have been recommended. The one recommended by the American Joint Committee on Cancer is available at http://www.cancerstaging.org.
CLINICAL FEATURES
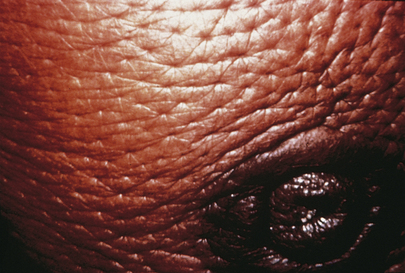
Carcinoma of the breast is usually painless and may be freely mobile. A serous or bloody nipple discharge may be present. With progressive growth, the tumor may become fixed to the deep fascia. Extension to the skin may cause retraction and dimpling, whereas ductal involvement may cause nipple retraction. Blockage of skin lymphatics may cause lymphedema and thickening of the skin, a change referred to as peau d’orange (Figure 29-2) due to its “orange peel” appearance.
ADJUVANT THERAPY
Current recommendations for adjuvant chemotherapy and hormonal therapy are as follows:
An added bonus of tamoxifen is a 70% reduction in the risk for cancer in the contralateral breast.
Bonadonna G., Valagussa P., Veronesi U. Lessons from the initial adjuvant cyclophosphamide, methotrexate, and fluorouracil studies in operable breast cancer. J Clin Oncol. 2008;26:342-344.
Clarke M., Coates A.S., Darby S.C. for the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG): Adjuvant chemotherapy in oestrogen-receptor-poor breast cancer: Patient-level meta-analysis of randomised trials. Lancet. 2008;371:29-40.
Del Mastro L., Dozin B., Aitini E., et al. Timing of adjuvant chemotherapy and tamoxifen in women with breast cancer: Findings from two consecutive trials of Gruppo Oncologico-Ovest-Mammel; a Intergruppo (GONO-MIG) Group. Ann Oncol. 2008;19:299-307.
Goldhirsch A., Wood W.C., Gelber R.D., et al. for the 10th St. Gailen Conference: Progress and promise: Highlights of the International Expert Consensus on the Primary Therapy of Early Breast Cancer 2007. Ann Oncol. 2007;18:1133-1144.
Mansel R., Locker G., Fallowfield L., et al. Cost-effectiveness analysis of anastrozole vs tamoxifen in adjuvant therapy for early stage breast cancer in the United Kingdom: The 5-year completed treatment analysis of the ATAC (“Arimidex,” Tamoxifen Alone or in Combination) trial. Br J Cancer. 2007;97:152-161.