CHAPTER 10 Breast
Symptoms of breast disease
Patients with breast disease present with either a lump, discharge from the nipple, pain in the breast, abnormality of the nipple, or a change in size of the breast (→ Table 10.1).
| Breast lump | Carcinoma, cyst, localized area of fibroadenosis, fibroadenoma, breast abscess, fat necrosis, duct ectasia, lipoma, galactocele, phyllodes tumour, cyst of Montgomery’s glands, sebaceous cyst |
| Pain in the breast | Cyclical and non-cyclical breast pain Carcinoma (85% are painless) Duct ectasia (pain behind the nipple) Infection: Fat necrosis |
Serous (early pregnancy)
Yellowish, brown or dark green (benign nodularity)
Thick and creamy (duct ectasia)
Purulent (rarely in association with breast abscess)
Milky (late pregnancy, post-lactation, prolactinoma)
Inflammation (eczema, Paget’s disease)
Destruction (Paget’s disease)
Mamillary fistula
Examination
Investigations
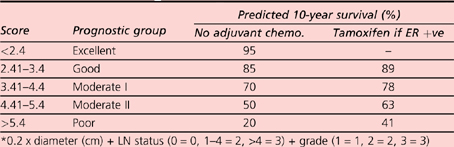
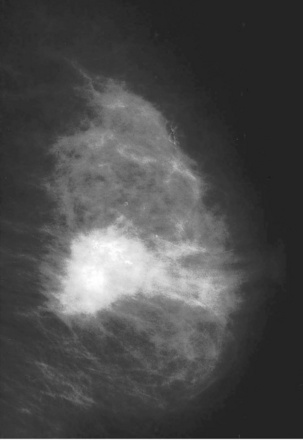
Cases are discussed with the pathological and radiological findings at a multidisciplinary team meeting. The radiological size of a tumour and lymph node status, its histological type (e.g. ductal, lobular, mucinous) and hormonal receptor status (oestrogen receptor, progesterone receptor and HER2 protein receptor positivity) are reviewed with patients clinical and social history and a plan for both surgery and adjuvant therapy is made. The Nottingham Prognostic Index combines data of both stage and grade to offer a prognostic score, which enables the benefits of adjuvant therapies to be weighed against the risks (Table 10.2).
Benign nodularity/breast pain
Treatment
Intraduct papilloma
The papilloma is usually in a solitary duct near the nipple in a young woman.
Risk factors
Investigations
Clinical staging
| Stage I | Lump <5 cm; not fixed deeply |
| Stage II | As for stage I but mobile, ipsilateral axillary nodes |
| Stage III | Lump >5 cm fixed to skin with fixed ipsilateral axillary nodes, or supraclavicular nodes, or peau d’orange, or arm oedema |
| Stage IV | Distant metastases |
| Primary (T) | Tis – carcinoma in situ T0 – no primary tumour located T1 – tumour <2 cm T2 – tumour 2–5 cm T3 – tumour >5 cm T4 – extension to chest wall |
| Nodes (N) | N0 – no nodal involvement N1 – mobile ipsilateral axillary nodes N2 – fixed ipsilateral axillary nodes N3 – ipsilateral supraclavicular nodes |
| Metastases (M) | M0 – no metastases M1 – distant metastases |