Chapter 20 Bradycardias and Tachycardias Review and Differential Diagnosis
Bradycardias (Bradyarrhythmias)
A number of arrhythmias and conduction disturbances associated with a slow heart rate have been described. The term bradycardia (or bradyarrhythmia) refers to arrhythmias and conduction abnormalities that produce a heart rate of less than 60 beats/min. Fortunately, the differential diagnosis of a slow pulse is relatively simple in that only a few causes must be considered. Bradyarrhythmias fall into five general classes (Box 20-1).
Sinus Bradycardia and Related Rhythms
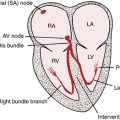
Sinus bradycardia is sinus rhythm with a rate less than 60 beats/min (Fig. 20-1). When 1:1 AV conduction is present, each QRS complex is preceded by a P wave; the P wave is negative in lead aVR and positive in lead II, indicating that the sinoatrial (SA) node is the pacemaker. Some individuals may have sinus bradycardia of 30 to 40 beats/min or less.
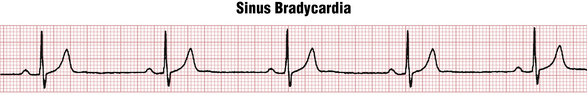
Figure 20-1 Marked sinus bradycardia at about 40/min. Sinus arrhythmia is also present. Sinus bradycardia (like sinus tachycardia) always needs to be interpreted in clinical context because it may be a normal variant (due to increased vagal tone in a resting athlete or in a healthy person during sleep) or may be due to drug effect/toxicity, sinus node dysfunction, etc., as discussed in Chapter 13. The PR interval here is also slightly prolonged (0.24 sec), also consistent with increased vagal tone or with certain drugs that depress activity in the SA and AV nodes (e.g., beta blockers).
Sinus bradycardia may be related to a decreased firing rate of the sinus node pacemaker cells or to actual SA block (see Chapter 13). The most extreme example of sinus node dysfunction is SA node arrest (see Chapters 13 and 19). Sinus bradycardia may also be associated with wandering atrial pacemaker (WAP).
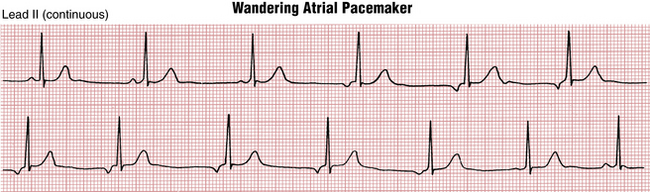
Wandering Atrial Pacemaker
Wandering atrial (supraventricular) pacemaker is an arrhythmia that is somewhat difficult to classify. As shown in Figure 20-2, this rhythm is characterized by multiple P waves of varying configuration with a relatively normal or slow heart rate. This pattern reflects shifting of the intrinsic pacemaker between the sinus node and different ectopic atrial sites, and sometimes the area around the AV junction (node).
Clinicians should be aware that WAP is quite distinct from multifocal atrial tachycardia (MAT), another arrhythmia with multiple different P waves. In WAP the rate is normal or slow. In MAT it is rapid. For rhythms that resemble MAT (see Chapter 14), but with rates between 60 to 100 beats/min, the more general term multifocal atrial rhythm can be used.
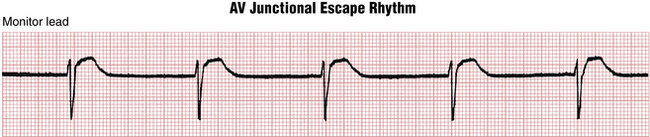
AV Junctional (Nodal) and Ectopic Atrial Rhythms
With a slow AV junctional escape rhythm (Fig. 20-3) either the P waves (seen immediately before or just after the QRS complexes) are retrograde (inverted in lead II and upright in lead aVR), or no P waves are apparent if the atria and ventricles are stimulated simultaneously. Slow heart rates may also be associated with ectopic atrial rhythms, including WAP (see previous discussion).
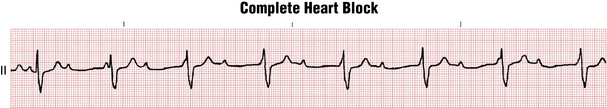
AV Heart Block (Second or Third Degree) or AV Dissociation
A slow ventricular rate of 60 beats/min or less (even as low as 20 beats/min) is the rule with complete heart block because of the slow intrinsic rate of the nodal (junctional) or idioventricular pacemaker (Fig. 20-4). In addition, patients with second-degree block (nodal or infranodal) often have a bradycardia because of the dropped (nonconducted) beats (see Chapter 17).
Isorhythmic AV dissociation and related arrhythmias, which may be confused with complete AV heart block, is also frequently associated with a heart rate of less than 60 beats/min (see Chapter 17).
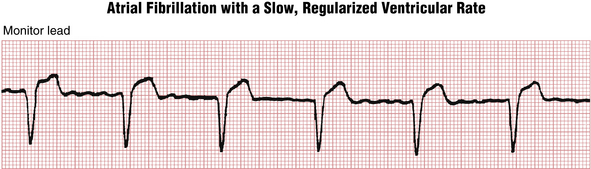
Atrial Fibrillation or Flutter with a Slow Ventricular Rate
Paroxysmal atrial fibrillation (AF), prior to treatment, is generally associated with a rapid ventricular rate. However, the rate may become excessively slow (less than 50 to 60 beats/min) because of drug effects or toxicity (e.g., beta blockers, calcium channel blockers, digoxin) or because of underlying disease of the AV junction (Fig. 20-5). In such cases the ECG shows the characteristic atrial fibrillatory (f) waves with a slow, sometimes regularized ventricular (QRS) rate. The f waves may be very fine and easily overlooked. A very slow, regularized ventricular response in AF suggests the presence of underlying complete AV heart block (see Chapters 15 and 17).
Idioventricular Escape Rhythm
When the SA nodal and AV junctional escape pacemakers fail to function, a very slow pacemaker in the ventricular conduction (His-Purkinje) system may take over. This rhythm is referred to as an idioventricular escape rhythm (see Fig. 13-10). The rate is usually very slow (often less than 45 beats/min), and the QRS complexes are wide without any preceding P waves. In such cases of “pure” idioventricular rhythm, hyperkalemia should always be excluded. In some cases of complete heart block, you may see sinus rhythm with an idioventricular escape rhythm, as described here. Idioventricular rhythm may be a terminal finding in irreversible cardiac arrest (also see Chapter 19).
Tachycardias (Tachyarrhythmias)
From a clinician’s perspective, the tachyarrhythmias can be most usefully divided into two general groups: those with a “narrow” (normal) QRS duration and those with a “wide” QRS duration (Table 20-1).
TABLE 20-1 Major Tachyarrhythmias: Simplified Classification
| Narrow QRS Complexes | Wide QRS Complexes |
|---|---|
| Sinus tachycardia | Ventricular tachycardia |
| Paroxysmal supraventricular tachycardias (PSVTs)∗ | Supraventricular tachycardia with aberration caused by a bundle branch block or Wolff-Parkinson-White preexcitation with (antegrade) conduction down the bypass tract |
| Atrial flutter | |
| Atrial fibrillation |
∗ The three most common types of PSVTs are AV nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia (AVRT) involving a bypass tract, and atrial tachycardia (AT) including unifocal and multifocal atrial tachycardia, as discussed in Chapter 14. Other nonparoxysmal supraventricular tachycardias also may occur, including types of so-called incessant atrial, junctional, and bypass tract tachycardias. (For further details of this advanced topic, see selected references cited in the Bibliography.)
Narrow complex tachycardias are almost invariably supraventricular (i.e., the focus of stimulation is within or above the AV junction). Wide complex tachycardias, by contrast, are either ventricular or supraventricular with aberrant ventricular conduction (i.e., supraventricular tachycardia [SVT] with aberrancy).
The four major classes of supraventricular tachyarrhythmia∗ are sinus tachycardia, paroxysmal supraventricular tachycardia (PSVT), atrial flutter, and AF. With each class, cardiac activation occurs at one or more sites in the atria or AV junction (node), above the ventricles (hence supraventricular). This activation sequence is in contrast to ventricular tachycardia (VT) in which the depolarization impulses originate in the ventricles. VT is simply a run of three or more consecutive premature ventricular depolarizations (see Chapter 16). The QRS complexes are always wide because the ventricles are not being stimulated simultaneously. The rate of VT is usually between 100 and 200 beats/min. By contrast, with supraventricular arrhythmias the ventricles are stimulated normally (simultaneously), and the QRS complexes are therefore narrow (unless a bundle branch block is also present).
Differential Diagnosis of Narrow Complex Tachyarrhythmias
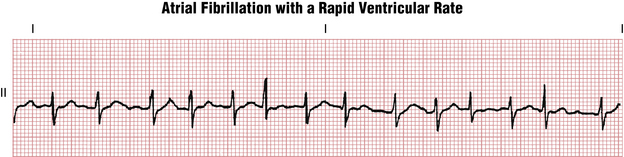
PSVT and AF can generally be distinguished on the basis of their regularity. PSVT resulting from AV nodal reentry or a concealed bypass tract is usually an almost perfectly regular tachycardia with a ventricular rate between 140 and 250 beats/min (see Chapter 14). AF, on the other hand, is distinguished by its irregularity. Remember that with rapid AF (Fig. 20-6) the f waves may not be clearly visible, but the diagnosis can be made in almost every case by noting the absence of true P waves and the haphazardly irregular QRS complexes.
Atrial flutter is characterized by “sawtooth” flutter (F) waves between QRS complexes (Fig. 20-7). However, when atrial flutter is present with 2:1 AV block (e.g., the atrial rate is 300 beats/min and the ventricular response is 150 beats/min), the F waves are often hidden or obscured in one or more leads. Therefore, atrial flutter with a regular ventricular rate of 150 beats/min can be confused with sinus tachycardia, PSVT, or AF (Fig. 20-8). AF can be most readily excluded because atrial flutter with 2:1 conduction is generally very regular.

Figure 20-7 Atrial flutter with 2:1 atrioventricular (AV) conduction (block). The flutter waves are subtle.
Nevertheless, the differential diagnosis of sinus tachycardia, PSVT, AF, and atrial flutter can be challenging (see Fig. 20-8). One measure often used to help separate these arrhythmias is carotid sinus massage (CSM).∗ Pressure on the carotid sinus produces a reflex increase in vagal tone. The effects of CSM on sinus tachycardia, reentrant types of PSVT, and atrial flutter are briefly reviewed next (see also Chapter 14).
Paroxysmal Supraventricular Tachycardias
PSVT resulting from AV nodal reentry tachycardia (AVNRT) or AV reentry tachycardia (AVRT) involving a concealed or manifest bypass tract usually has an all-or-none response to CSM. In successful cases the tachycardia breaks suddenly, and sinus rhythm resumes (see Chapter 14). At other times CSM has no effect, and the tachycardia continues at the same rate. In cases of PSVT caused by atrial tachycardia (AT), CSM may have no effect or may increase the degree of block, resulting in a rapid sequence of one or more nonconducted P waves.
Atrial Flutter
CSM often increases the degree of AV block in atrial flutter, converting flutter with a 2:1 response to 3:1 or 4:1 flutter with a ventricular rate of 100 or 75 beats/min, respectively, or to flutter with variable block. Slowing of the ventricular rate unmasks the characteristic F waves but does not convert the arrhythmia to sinus (see Chapter 15). Therefore, if you know your patient has atrial flutter or fibrillation, there is no justification for using CSM.
Differential Diagnosis of Wide Complex Tachycardias
Tachycardias, as noted, are subdivided by cardiologists into SVTs and VT. A tachycardia with widened (broad) QRS complexes (i.e., 120 msec or more in duration) indicates two possible diagnostic considerations:
1. The first and more important is VT, a potentially life-threatening arrhythmia. As noted, VT is a consecutive run of three or more ventricular premature beats (VPBs) at a rate generally between 100 and 200 beats/min or more. It is usually, but not always, very regular, especially monomorphic VT at higher rates.
2. The second possible cause of a tachycardia with widened QRS complexes is so-called SVT with aberration or aberrancy. The term aberration simply means that some abnormality in ventricular activation is present, causing widened QRS complexes due to asynchronous activation.
Differentiation of SVT with Aberrancy from Ventricular Tachycardia
Ventricular aberrancy with an SVT, in turn, has two major, general mechanisms: a bundle branch block (intraventricular) conduction delay and, much more rarely, conduction down a bypass tract in conjunction with the Wolff-Parkinson-White (WPW) preexcitation syndrome (Chapters 12 and 14).
SVT with Aberrancy
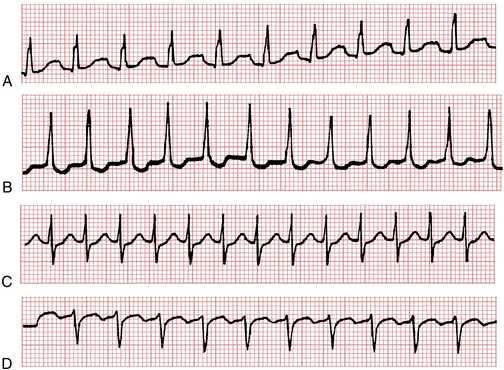
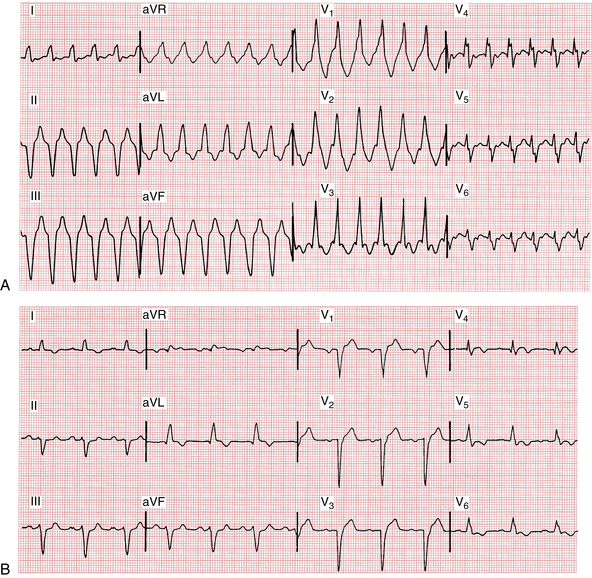
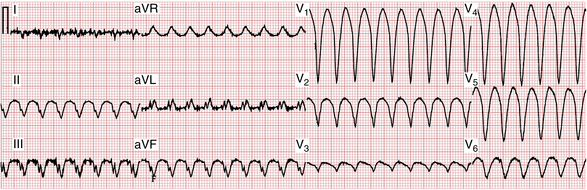
Figure 20-9A shows AF with a rapid ventricular response occurring in conjunction with LBBB. Figure 20-9B shows an example of VT. Because the arrhythmias look so similar, it can be difficult to tell them apart. The major distinguishing feature is the irregularity of the AF as opposed to the regularity of the VT. However, VT sometimes may be irregular. Another example of AF with aberrancy (due to LBBB) is shown in Figure 20-10.
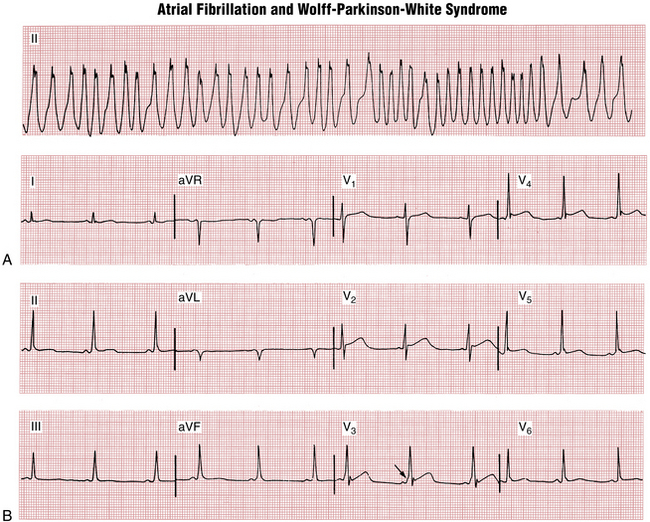
SVT with the Wolff-Parkinson-White Preexcitation Syndrome
The second general mechanism responsible for a wide complex tachycardia is SVT with the WPW syndrome. As noted elsewhere (see Chapters 12 and 14) patients with WPW preexcitation have an accessory pathway connecting the atria and ventricles, thus bypassing the AV junction. Such patients are especially prone to a reentrant type of PSVT with narrow (normal) QRS complexes. This distinct type of PSVT is called (orthodromic) AV reentrant tachycardia (AVRT).
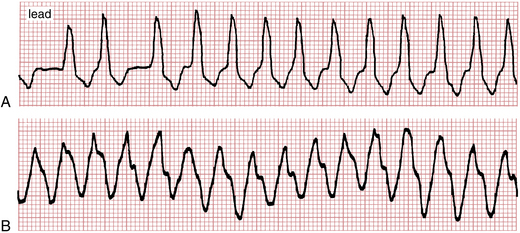
Sometimes, however, particularly if AF or atrial flutter develops, a wide complex tachycardia may result from conduction down the bypass tract at very high rates. This kind of wide complex tachycardia obviously mimics VT. An example of WPW syndrome with AF is shown in Figure 20-11.
WPW syndrome with AF should be strongly suspected if you encounter a wide complex tachycardia that (1) is irregular and (2) has a very high rate (i.e., very short RR intervals). In particular, RR intervals of 200 msec or less are rarely seen with conventional AF and very rapid VT is usually quite regular. These very short RR intervals are related to the ability of the bypass tract (in contrast to the AV node) to conduct impulses in extremely rapid succession (see Fig. 20-11A).
WPW syndrome with a wide QRS complex may also occur in two other pathophysiologic contexts: (1) PSVT with a reentrant circuit that goes down the bypass tract and reenters the atria through the ventricular conductions system and AV node is a very rare variant is called antidromic AV reentrant tachycardia (AVRT). (2) The more common variant, namely, conduction down the AV node-His-Purkinje system and up the bypass tract, occurs in association with a bundle branch block. For more information on these advanced topics, please see the Bibliography and the online supplement.
VT vs. SVT with Aberration: Important Diagnostic Clues in Wide Complex Tachycardia
Clinical Clues
• Over 80% of WCTs presenting to medical attention are VTs. In patients with known structural heart disease (e.g., prior infarcts, cardiomyopathies) this percentage increases to over 90%.
• Treating SVT as VT will most likely cure the arrhythmia, but treating VT as SVT can precipitate hemodynamic collapse (see next bullet). When in doubt about managing a WCT, therefore, assume the diagnosis of VT until proved otherwise.
• Remember that intravenously administered verapamil should not be used in undiagnosed WCTs. This vasodilating drug with negative inotropic effects can cause hemodynamic collapse in patients with VT or AF with WPW preexcitation syndrome that may simulate VT.
ECG Clues
Five classes of ECG clues may be especially helpful in favoring VT over SVT with aberrancy:
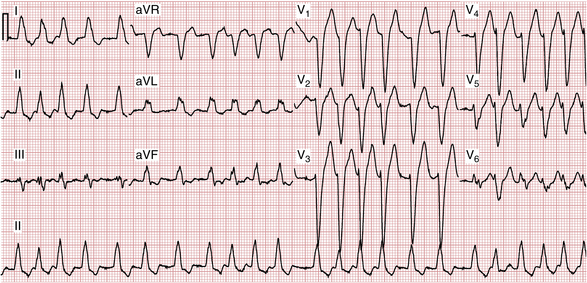
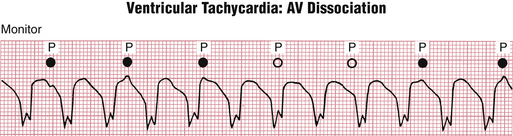
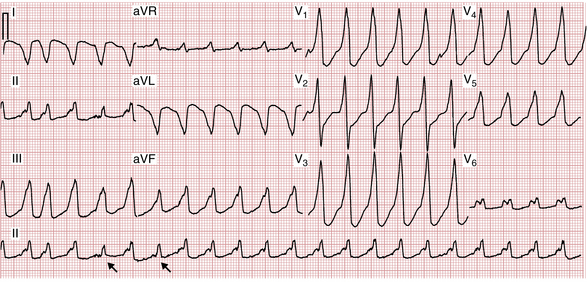
1. AV dissociation is a key clue that may be especially helpful in differentiating SVT with aberrancy from VT. Recall from Chapter 15 that with AV dissociation the atria and ventricles are paced from separate sites, with the ventricular rate equal to or faster than the atrial rate. Some patients with VT also have AV dissociation; in other words, the ventricles are paced from an ectopic ventricular site at a rapid rate, while the atria continue to be paced independently by the SA node. In such cases, you may be able to see P waves occurring at a slower rate than the rapid wide QRS complexes (Fig. 20-12). Some of the P waves may be buried in the QRS complexes and, therefore, difficult or impossible to discern.
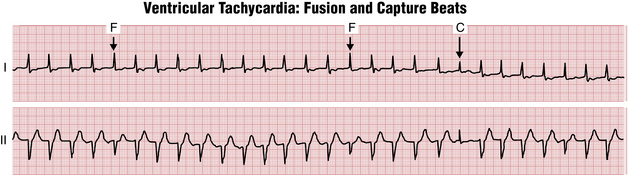
Furthermore, in some cases of VT with AV dissociation the SA node may transiently “capture” the ventricles, producing a capture beat, which has a normal QRS duration, or this mechanism may produce a fusion beat, in which the sinus and ventricular beats coincide to produce a hybrid complex. Figure 20-13 illustrates capture and fusion beats due to AV dissociation occurring with VT.
2. Morphology refers to the shape of the QRS complex in leads V1/V2, and V6. The morphology of the QRS in selected leads may help provide important clues about whether the wide complex tachycardia is (monomorphic) VT or not. When the QRS shape during a tachycardia resembles an RBBB pattern, a typical rSR′ shape in lead V1 suggests SVT while a single broad R wave or a qR, QR, or RS complex in that lead strongly suggests VT (Fig. 20-14). When the QRS shape during a tachycardia resembles an LBBB pattern, a broad (≥0.04 sec) initial R wave in lead V1 or V2 or a QR complex in lead V6 strongly suggests VT (Box 20-2).
BOX 20-2 Wide Complex Tachycardia: Selected Criteria Favoring Ventricular Tachycardia
∗ QRS duration may also be increased in supraventricular tachycardias in the presence of drugs that prolong QRS interval or with hyperkalemia.
Adapted from Josephson ME, Zimetbaum P: The tachyarrhythmias. In Kasper DL, Braunwald E, Fauci A, et al (eds): Harrison’s Principles of Internal Medicine, 16th ed. New York, McGraw-Hill, 2004.
3. The QRS duration. A QRS width of greater than 0.14 sec with an RBBB morphology or greater than 0.16 sec with an LBBB morphology suggests VT. However, this criterion is not as reliable if the patient is on a drug that widens the QRS complex, such as flecainide, or in the presence of hyperkalemia. Remember to look at all 12 leads and measure this duration in the lead with the widest QRS. (You should also be aware that even though most cases of VT are associated with a very wide QRS complex, VT may occur with a QRS complex that is only mildly prolonged, particularly if the arrhythmia originates in the upper part of the ventricular septum or in the proximal part of the fascicles.)
4. QRS concordance means that the QRS waveform has identical or near identical polarity in all six chest leads (V1-V6). Positive concordance (Fig. 20-15) is defined by wide R waves in leads V1-V6 and negative concordance by wide QS waves (Fig. 20-16) in these leads. Either positive or negative concordance is a specific, but not very sensitive, indicator of VT—helpful when you see these signs, but they are not common findings even when VT is present.
5. Prior sinus rhythm ECGs. A comparison using available prior ECGs during sinus rhythm (or other supraventricular rhythms) may be helpful, especially if the prior ECG is relatively recent. Most important is finding that the sinus rhythm QRS configuration (morphology and axis) remains identical during the WCT; this observation strongly suggests a supraventricular mechanism. On the other hand, if the QRS configuration during the WCT is identical to any VPBs during sinus rhythm, this finding points to VT as the cause of a longer run of wide complex beats.
Box 20-2 summarizes some aspects of the differential diagnosis of VT versus SVT with aberration.
Clinical Significance: Some Important Reminders
As mentioned previously, the first question to ask in looking at any tachyarrhythmia is whether the rhythm is VT. If sustained VT is present, emergency treatment is required (see Chapter 16). The treatment of narrow complex tachycardias depends on the clinical setting. In patients with sinus tachycardia (see Chapter 13), treatment is directed at the underlying cause (e.g., fever, sepsis, congestive heart failure, alcohol withdrawal, or hyperthyroidism).
Another major question to ask about any patient with a tachyarrhythmia (or any arrhythmia for that matter) is whether digitalis or other drugs are part of the therapeutic regimen. Some arrhythmias (e.g., AT with block) may be digitalis toxic rhythms, disturbances for which electrical cardioversion is contraindicated (see Chapter 18). Drug-induced QT prolongation is an important substrate for torsades de pointes type of polymorphic VT, as discussed in Chapter 16.
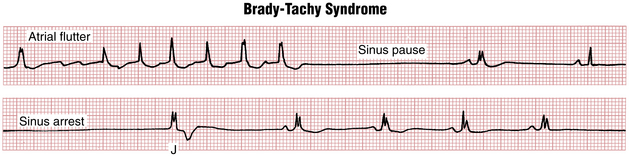
Slow and Fast: Sick Sinus Syndrome and the Brady-Tachy Syndrome
In some patients with sick sinus syndrome, bradycardia episodes are interspersed with paroxysms of tachycardia (usually AF, atrial flutter, or some type of PSVT). Sometimes the bradycardia occurs immediately after spontaneous termination of the tachycardia. An important subset includes patients with paroxysmal AF have marked sinus bradycardia and even sinus arrest after spontaneous conversion of AF (see Chapters 13 and 15). The term brady-tachy syndrome has been used to describe patients with sick sinus syndrome who have both tachyarrhythmias and bradyarrhythmias (Fig. 20-17).
∗ Remember: supraventricular tachycardia is a source of common confusion in terminology (see Chapter 14). Clinicians use the term supraventricular tachycardia (SVT) in several related, but different, ways. First, SVT is used by some to refer to any rapid rhythm originating in the SA node, atria, or AV junction, above the ventricular conduction system (hence supraventricular). Second, others use the term in the same way, but exclude sinus tachycardia. Third, SVT is used by other clinicians more specifically to be synonymous with the class of paroxysmal supraventricular tachycardias (PSVTs) that include three rhythms: atrial tachycardias, AV nodal reentrant tachycardia (AVNRT), and AV reentrant tachycardia (AVRT), which involves a concealed or manifest (WPW-type) bypass tract. These PSVTs are distinct from sinus tachycardia, AF, or atrial flutter (see Chapters 12, 14, and 15). Make sure when you hear supraventricular tachycardia you are clear about the specific meaning.
∗ Note: CSM is not without risks, particularly in elderly patients or in those with cerebrovascular disease. Interested readers should consult relevant references in the Bibliography for details on this and other vagal maneuvers, as well as on the use of adenosine in the differential diagnosis of narrow complex tachycardias.