CHAPTER 14 Brachial plexus anatomy
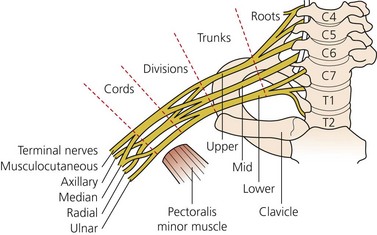
Before selection of technique, it is important to have a thorough understanding of brachial plexus anatomy. The plexus is composed of roots, trunks, divisions, cords, and branches (Fig. 14.1). The brachial plexus stems from the ventral rami of the C5 to T1 nerve roots in the majority of individuals. Approximately 15% of patients may have contributions to the brachial plexus from the C4 or T2 nerve roots, creating a ‘prefixed’ or ‘postfixed’ plexus (see Fig. 15.9). The cervical roots emerge from the intervertebral foramina and lie on a sulcus on the vertebral transverse processes between the anterior and posterior tubercles to which the scalene muscles are attached. Immediately lateral to the transverse processes of the cervical vertebrae, the nerve roots are sheathed in the prevertebral fascia. The nerve roots then travel between the scalene muscles and form three trunks (upper, middle, and lower). The interscalene groove is a palpable surface anatomy depression between the anterior and middle scalene muscles; it allows clinicians easy and reliable access to the roots and trunks of the plexus. The roots are posterior to the vertebral artery – an important anatomic relation for the interscalene block.
Branches of the brachial plexus
Infraclavicular branches
The infraclavicular branches are derived from the three cords of the brachial plexus.
The radial nerve
The deep branch of the radial nerve
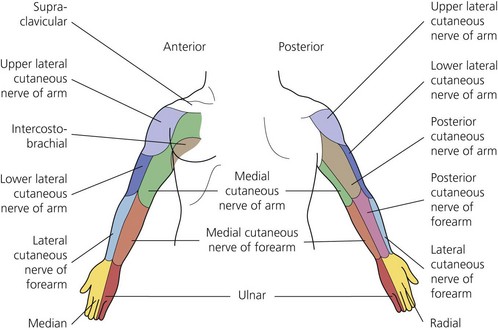
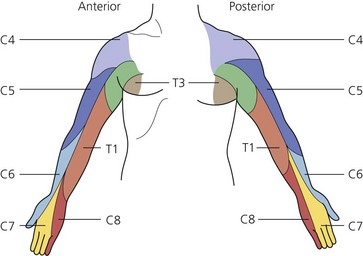
The sensory (Figs 14.2 and 14.3) and motor innervation of the upper limb is clinically important. Knowledge of sensory innervation helps determine which cutaneous nerve distributions within a surgical field require blockade. Motor innervation is clinically relevant as a means of matching a peripheral nerve stimulation response to a particular nerve being stimulated. As the arm has multiple innervation, assessment of block efficacy is best achieved by assessing function unique to each nerve. It is important to remember that significant variation in the structure of the brachial plexus occurs, with seven major configurations described.