CHAPTER 5 Bony Impingement of the Ankle and Subtalar Joints
Ankle sprains are one of the most common injuries seen in sports medicine, and most heal without persistent pain or chronic disability.1,2 However, some patients with ankle sprains continue to have persistent pain and dysfunction.2,3 Two common sources of chronic pain and disability—persistent ankle instability and impingement—may occur separately or concomitantly. Impingement, which is entrapment of an anatomic structure that leads to pain and decreased range of motion of the ankle, can be classified as soft tissue or osseous.4
Osseous or bony impingement most commonly results from spur formation along the anterior margin of the distal tibia and talus or from a prominent posterolateral talar process (i.e., os trigonum). Soft tissue impingement usually results from scarring and fibrosis associated with synovial, capsular, or ligamentous injury, and it most often occurs in the anterolateral gutter, medial ankle, or region of the syndesmosis.5
Of the first few ankle impingement syndromes reported in the English literature, all involved bone. They usually have occurred in athletes whose sports necessitated sudden acceleration, jumping, and extremes of dorsiflexion or plantar flexion. The so-called athlete’s ankle was first mentioned in the orthopedic literature by Morris6 and was subsequently reported by McMurray,7 who called it footballer’s ankle. McMurray stated that the footballer’s ankle was peculiar to the professional soccer player, especially those older than 25 years who have played for many years. In later studies, this entity was described in many other athletic activities, including rugby players, football players, ballet dancers, jumpers, and runners, and it can occur in any sport.
BONY IMPINGEMENT
Etiology
Osteophytes are protrusions of bone and cartilage around the joint space. Osteophytic formations occur with weight-bearing articular cartilage damage, such as osteoarthritis of the hip and knee, and occur without weight-bearing articular cartilage damage, such as bony impingement lesions.8
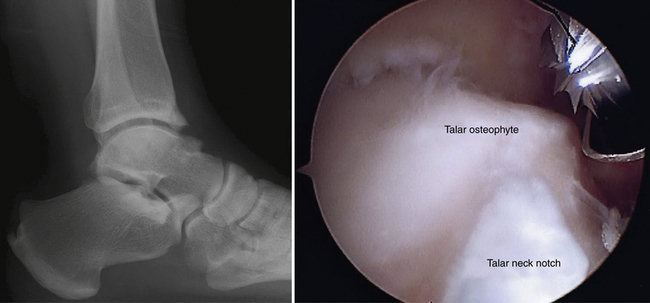
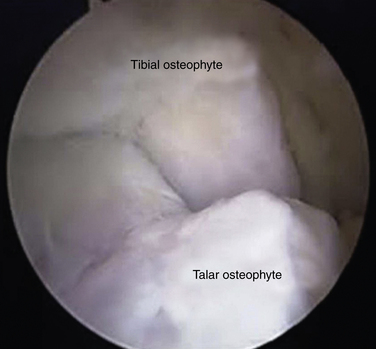
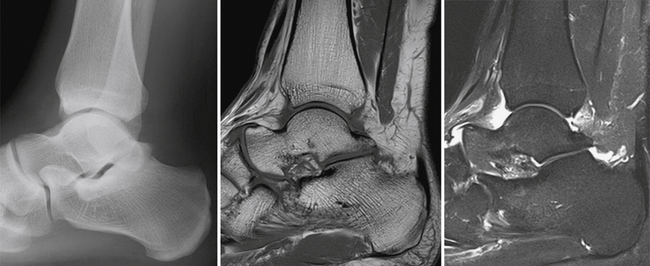
Controversy exists about the cause of bony osteophytes around the ankle with normal articular cartilage. Adjacent or articulating bones that are repetitively in contact can stimulate the cambium layer, the deep layer of periosteum that has osteogenic potential, to form osteophytes. The osteophytic prominence causes bony impingement, often increases in size, and eventually may break off, forming a loose body. After the spur is formed, it may alter normal mechanics or motion of the ankle. Morris6 and McMurray7 described osseous exostoses of the anterior rim of the tibia and the sulcus of the talus, and they believed these to result from a traction injury of the joint capsule of the anterior aspect of the ankle that occurred when the foot was in extreme plantar flexion (i.e., capsule-ligament traction). However, the capsule of the ankle attaches above the location of the tibial osteophytes and distal to the talar ones. In later studies, anatomic observations during arthroscopic surgery confirmed that tibial osteophytes were located at the joint level and talar osteophytes were found proximal to the talar neck notch, away from the capsular attachment sites (Fig. 5-1); the osteophytes were intra-articular.9,10 O’Donoghue11 attributed these exostoses to direct osseous impingement during forced dorsiflexion or to post-traumatic calcification. Van Dijk and colleagues12 attributed the osteophytes to medial impingement from inversion of the talus onto the medial tibia and thought they might be related to instability (Fig. 5-2). The osteophytes were related to direct trauma associated with the impingement of the anterior articular border of the tibia in the talar neck during forced dorsiflexion of the ankle joint.
Classification
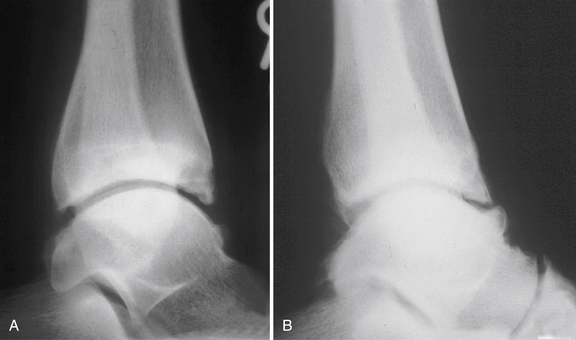
In 1992, Scranton and McDermott8 classified four types of anterior ankle impingement by the radiographic appearance of bony spurs (Table 5-1). The classification system grades the degree of spur formation and assists in predicting the length of recovery time. Van Dijk’s 1997 radiographic classification (Table 5-2) was based on osteoarthrosis of the ankle on plain radiographs (Fig. 5-3).10 The degree of osteoarthritic change is a better prognostic indicator for the outcome of arthroscopic surgery for anterior ankle impingement than size and location of spurs.
TABLE 5-1 Classification of Anterior Ankle Impingement
From Scranton PE Jr, McDermott JE. Anterior tibiotalar spurs: a comparison of open versus arthroscopic débridement. Foot Ankle. 1992;13:125-139.
TABLE 5-2 Classification of Osteoarthritic Changes of the Ankle Joint
| Grade | Characteristics |
|---|---|
| 0 | Normal joint or subchondral sclerosis |
| I | Osteophytes without joint space narrowing |
| II | Joint space narrowing with or without osteophytes |
| III | Total disappearance or deformation of the joint space |
From van Dijk CN, Tol JL, Verheyen CC. A prospective study of prognostic factors concerning the outcome of arthroscopic surgery for anterior ankle impingement. Am J Sports Med. 1997;25:737-745.
THE ANKLE JOINT
The Anterior Ankle
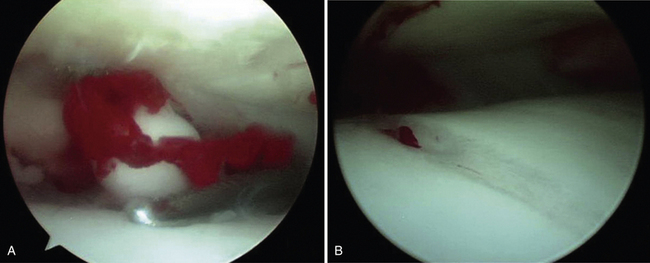
Anterior impingement syndrome of the ankle is the most common cause of anterior ankle pain in many sports participants. Repetitive forced dorsiflexion also can result in impaction-related microtrauma of the anterior chondral margin of the tibiotalar joint. Over time, attempted repair with resultant fibrosis and fibrocartilage proliferation leads to the formation of osteophytes.7 When osteophytes form, they limit dorsiflexion, facilitate further impingement, and result in more periosteal stimulation, creating a repetitive cycle. Careful inspection of the pathologic anatomy shows that osteophytes do not form in the capsular insertion but instead where bones come together.11 Osteophytes can break off and become loose bodies (Fig. 5-4).
In supination injury, damage to the anterior non–weight-bearing cartilage rim occurs.12 The cartilage proliferation, scar tissue formation, and calcification that may result from attempted repair depend on the degree of initial damage and on chondral and bone cell stimulation. Recurrent forced dorsiflexion of the ankle is the main factor in the development of spurs.13,14 Another factor is recurrent microtrauma, and it has been demonstrated that spur formation is related to recurrent ball impacts in soccer players.15 The entire process of spur formation and hypertrophied synovium or fibrosis is exacerbated by recurrent ankle sprains and persistent ankle instability. Synovial changes may result from chronic inflammation of the soft tissue (e.g., synovial fold, subsynovial fat, collagen tissue) that was crushed during forced dorsiflexion movements between spurs.16
The common history of patients with anterior ankle impingement is recurrent inversion sprain. The typical patient is a young athlete presenting with chronic anterior ankle pain.17 Pain likely results from entrapment of hypertrophied synovial tissue between the talus and the anterior tibia, which is exacerbated by the presence of anterior spurs. Patient usually present with swelling after activity and with limited ankle dorsiflexion movement.
Standard lateral radiographs of the ankle usually show spurs. The weight-bearing lateral view with the ankle in maximal dorsiflexion (i.e., plié view) demonstrates anterior impingement, and this view commonly is used in evaluating dancers. Conventional magnetic resonance imaging (MRI) accurately detects and localizes anterior tibiotalar spurs, adjacent reactive synovitis and fibrosis, subchondral bone edema, and other coexisting lesions, such as collateral ligament complex injury, osteochondral lesions of the talus, or intra-articular bodies. There is little or no additional information gained through indirect magnetic resonance (MR) arthrography for evaluating anteromedial impingement compared with conventional MRI.18
Several conditions can mimic the anterior impingement syndrome, including osteochondritis dissecans of the talus, a “high” ankle sprain involving the anterior tibiofibular ligament,19 impingement by Bassett’s ligament,1 an aberrant distal insertion of the anterior tibiofibular ligament that can cause persistent symptoms, Ferkel’s disease,16 an accumulation of debris and synovitis in the anterolateral gutter, degenerative joint disease of the tibiotalar or talonavicular joints (especially in the early phases when the radiographic findings are subtle), and a stress fracture or an osteoid osteoma in the tarsal navicular.
Conservative treatment with rest, physical therapy, shoe modification, or local injection constitutes first-line therapy for most cases of anterior ankle impingement. If all modalities of conservative treatment are unsuccessful, operative treatment may be indicated. The goal of surgery is removal the osteophytes to restore the anterior space and to reduce the chance of symptoms recurring. Numerous investigators have reported good results with open arthrotomy, but it can be complicated by cutaneous nerve entrapment, wound dehiscence, damage of the long extensor tendons, and formation of hypertrophic scar tissue.7,11,17 In recent years, the arthroscopic treatment of anterior ankle impingement has had a high success rate. The first series reported by Biedert3 had a success rate of approximately 67%. Ferkel and colleagues16 reported a success rate of approximately 84% for 31 patients with soft tissue impingement of the ankle. Ogilvie-Harris and colleagues20 described an average of 39 months’ follow-up for patients who were treated for anterior ankle impingement by arthroscopic removal of bony spurs. The good and excellent results were obtained for 88% of 17 patients.20 In a prospective study, Amendola and coworkers21 treated 79 cases of ankle impingement by arthroscopic débridement. Fifteen cases of soft tissue impingement and 14 cases of anterior bony impingement were included in the study. There were statistically significant decreases in subjective analog scores. Eighty percent of the soft tissue impingement lesions and 86% of the bony impingement lesions benefited from the procedure. Eighteen percent of patients had neurologic complications, including partial deep peroneal nerve neurapraxia and superficial peroneal nerve irritation.21
Scranton and colleagues8 reported the comparative open and arthroscopic treatment of ankle impingement. The recovery time of the arthroscopic treatment patients was approximately one half of the time of open treatment patients. The patients treated arthroscopically returned to full athletic training 1 month faster than the other group.8
Tol and associates9 described the results for 5 to 8 years of follow-up for the arthroscopic treatment of anterior impingement in the ankle. Excellent or good results were obtained for 100% of patients without osteoarthritis, 77% of patients with grade I disease, and 53% of patients with grade II diseases according to the classification for osteoarthritis of the ankle (see Table 5-2).22 Osteophytes recurred in two thirds of the ankles with grade I osteoarthritis, but the recurrence of osteophytes did not correlate statistically with the return of symptoms. Narrowing of the joint space increased in 47% of patients with grade II osteoarthritis.9
Anteromedial Ankle Impingement
Anteromedial ankle pain is caused by impingement of the anterior portion of the medial malleolus on a spur on the medial shoulder of the talus. Spurs often occur on both sides of the joint. They result from injury to the deltoid ligament complex, leading to scar formation and synovitis along the anteromedial joint line. Patients complain of pain along the anteromedial joint line that is aggravated by walking or sporting activities. Patients often report a clicking sensation and painful limited dorsiflexion of the ankle. On physical examination, the anteromedial aspect of the ankle appears swollen and is tender to palpation over the anterior tibiotalar fascicle of the deltoid ligament. The anteromedial spur often can be palpated on physical examination but usually cannot be visualized on standard anteroposterior and lateral radiographs of the ankle. In a cadaver study, Tol and colleagues15 described medially located talar osteophytes and anteromedial tibial osteophytes that were up to 7.3 mm in diameter, originated from the anteromedial border, and could remain undetected due to overprojection or superposition of the lateral part of the talar neck and body and the prominent anterolateral border of the distal tibia, respectively.15
These osteophytes are easy to miss (i.e., “hidden spurs”). A special oblique anteromedial impingement view (Fig. 5-5) has been developed to aid in the detection of anteromedial spurs, and it is obtained with the beam tilted in a 45-degree craniocaudal direction with the leg in 30 degrees of external rotation and the foot in plantar flexion in relation to the standard lateral radiograph position.23 The sensitivity of lateral radiographs for detecting anterior tibial and talar osteophytes is 40% and 32%, and their specificity is 70% and 82%, respectively. The combination of lateral and oblique anteromedial impingement radiographs of the ankle increase the sensitivity to 85% for tibial osteophytes and 73% for talar osteophytes.24
Conventional MRI has not been useful in detecting anteromedial impingement syndrome. Robinson and associates25 demonstrated that the cross-sectional MR arthrography could confirm anteromedial ankle impingement. Their findings included capsular and synovial soft tissue thickening anterior to the tibiotalar ligaments and associated osseous abnormalities such as anteromedial osteophytes.25 The impingement is thought to be soft tissue entrapment associated with previous injury to the anterior tibiotalar fascicle of the deltoid ligament complex. A thickened anterior tibiotalar ligament can impinge on the anteromedial corner of the talus, often resulting in adjacent fibrosis or a meniscoid lesion and synovitis that may lead to adjacent spur formation.
Anterocentral Ankle Impingement
Anterolateral Ankle Impingement
Bassett’s Ligament.
Bassett’s ligament impingement is caused the distal fascicle of the anteroinferior tibiofibular ligament.1 It is a thickened distal fascicle of the anteroinferior tibiofibular ligament (AITFL) that extends far distally on the lateral malleolus. Nikolopoulos and coworkers26 considered this fascicle to be an independent accessory ligament. This anatomic structure represents a separate ligament rather than a distal component of the AITFL. A fibrofatty septum separated the AITFL from the accessory fascicle, similar to the one that covered the intermediate space between the interosseous and the anterior tibiofibular ligament.26 The lateral shoulder of the talus impinges against the distal fascicle of the AITFL when the ankle is plantar flexed. Patients had a history an inversion sprain of the ankle followed by chronic pain in the anterior aspect of the ankle, but they had no gross ligamentous instability. The post-traumatic anterolateral hyperlaxity due to an injured ATFL resulted in anterior extrusion of the talar dome with dorsiflexion, which contacted the distal fascicle of the AITFL with more pressure and friction.1
Temporarily relieving distraction is advised when resecting the AITFL because the AITFL lesion may be missed during distraction.26 Numerous surgeons have reported good to excellent results (89% to 100%)with arthroscopic resection.
Synovial Impingement.
Synovial impingement is a chronic, painful condition in which an accumulation of scar tissue and synovitis are trapped in the anterolateral gutter of the ankle, usually after inversion injuries.16 Wolin and associates27 were the first to describe synovial hypertrophy in the anterolateral aspect of the ankle. They called this, perhaps misleadingly, a meniscoid lesion, and histologic examination demonstrated that it was hyalinized connective tissue. Ankle arthroscopists have since recognized that there is a spectrum of sites where impingement can occur and that the condition is characterized by a range of histologic findings. The meniscoid appearance is unusual and is a pathologic rather than an anatomic variant.
Imaging may be of value, but the condition is usually a diagnosis based on clinical findings. Radiographs demonstrate no specific abnormality associated with anterolateral soft tissue impingement but are useful in excluding coexisting osseous abnormalities, such as fracture, osteochondral lesion of the talus, or anterior tibial spur formation. Computed tomography (CT) arthrography may provide evidence of anterolateral impingement, including intra-articular oblique linear formation, nodular thickening of the capsule, or irregularity of the edges of the anterolateral groove of the ankle.28 Conventional MRI of the ankle has a wide range of sensitivities (39% to 100%) and specificities (50% to 100%) with regard to establishing the diagnosis of anterolateral impingement.29–31 Factors associated with increased sensitivity and specificity of conventional MRI for confirming anterolateral impingement include the presence of a joint effusion and the experience level of the radiologist.31,32 The diagnosis can be suggested by MRI when fluid in the lateral gutter outlines an abnormal soft tissue structure separate from the anterior talofibular ligament.31 MR arthrography is highly accurate in the assessment of anterolateral impingement, with a sensitivity of 96%, specificity of 100%, and accuracy of 100% when clinical signs of anterolateral impingement are present.33
DeBerardino and coworkers34 reported a 96% rate of good or excellent results for arthroscopic treatment of soft tissue impingement of the ankle in athletes after an average follow-up of 27 months. Kim SH and colleagues35 reported good or excellent results (94% to 96%) with arthroscopic débridement for impingement of the anterolateral soft tissues of the ankle.
The Lateral Ankle
The “meniscoid” of the ankle is the soft tissue trapped between the lateral shoulder of the talus and the lateral malleolus. McCarroll and associates36 described this lesion in four soccer players who had a history of frequent ankle sprains, and after failing conservative treatment, they underwent arthroscopic débridement of the lesion. After appropriate rehabilitation, all four returned to competition with cessation of the symptoms; only one player rarely had pain.
Fracture of the lateral process of the talus37 causes impingement beneath the lateral malleolus. Snow-boarder’s fracture is a synonym for this fracture because of the increased incidence in this patient population. The fracture is often misdiagnosed as an ankle sprain, and routine plain radiographs often are read as normal. CT is the investigation of choice. Treatment is surgical excision or open reduction and internal fixation.38
The Medial Ankle
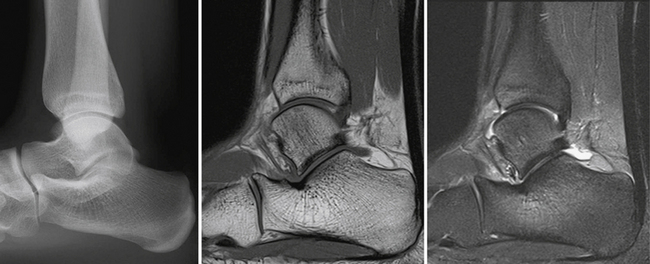
Medial ankle pain usually is not caused by bony impingement. Medial ankle sprains are rare because the medial structures are strong and rigid compared with lateral sprains, but after medial ankle instability occurs, medial osteophytes may cause bony medial impingement (Fig. 5-6). The medial ankle pain common in athletes typically is caused by posterior tibial tendonitis. Flexor hallucis longus (FHL) tendonitis often is found in dancers (i.e., dancer’s tendonitis), and it causes posteromedial pain. In dancers, the most common cause of pain around the medial malleolus comes from “rolling in” (i.e., pronating) to obtain proper turnout. This is one of many overuse syndromes causing chronic strain on the deltoid ligament. The lesion results from the chronic strain on the deep posterior fibers of the deltoid ligament complex between the medial talus and the medial malleolus. Injury leads to the formation of scar tissue and fibrosis located along the posteromedial joint line that becomes entrapped between the posterior talus and medial malleolus, resulting in persistent medial ankle pain. This lesion may be isolated, but it most often coexists with symptoms of anterolateral ankle pain and instability. If the lesion remains unrecognized and untreated, medial ankle impingement may result in persistent pain after lateral ankle reconstruction.39,40
The Posterior Ankle
Posterior ankle impingement, or talar compression syndrome,13 is natural result of full weight bearing in maximal plantar flexion of the ankle in full pointe position. It is also referred to as os trigonum syndrome, posterior triangle pain, and posterior tibiofibular impingement. Posterior ankle pain is common in athletes, dancers, gymnasts, swimmers, divers, figure skaters, and soccer players who require repetitive and extreme plantar flexion.
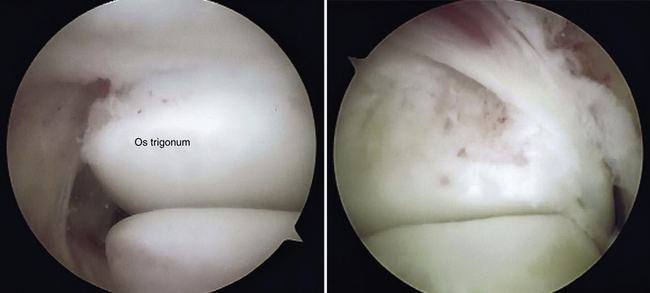
The key structures involved in posterior ankle impingement syndrome can be divided into osseous and soft tissue components. The osseous components include the posterior tibia and talus and the superior calcaneum. Posterior talar anatomy variations are the principal predisposing osseous factors in posterior ankle impingement syndrome. The posterior aspect of the talus has two tubercles: the medial tubercle and lateral tubercle. The lateral tubercle is the origin of the posterior tibiofibular ligament. If it is large, it is referred to as the posterior process of the talus, or Stieda’s process. The os trigonum is the ununited lateral tubercle on the posterior aspect of the talus. It is present in 7% to 14% of people, and it is often bilateral.41,42 The os trigonum is the second most common accessory bone in the foot; the accessory navicular is the most common.
Pain may result from osseous structures of the posterior ankle impacting one another or from compression of the soft tissue between the two opposing osseous structures. FHL tendon irritation is often caused by the adjacent impingement. Pain also can result from acute trauma to the posterolateral talar process or as a result of chronic repetitive microtrauma, causing direct injury to Stieda’s process or the os trigonum.43
Most patients with posterior ankle impingement respond to conservative treatment, such as rest, shoe modification, and physical therapy. Image-guided steroid and local anesthetic injection into areas of focal inflammation provides diagnostic confirmation and long-lasting symptomatic relief in most patients, and this approach avoids the need for surgery.44
Posterolateral Ankle Impingement
Posterolateral ankle impingement manifests as posterolateral pain in the back of the ankle when the posterior lip of the tibia closes against the superior border of the os calcis. Posterolateral ankle impingement is the natural result of full weight bearing in maximal plantar flexion of the ankle in the demi-pointe or full pointe position (Fig. 5-7).
Posterior ankle impingement is seen best on a lateral view of the ankle en pointe or in full plantar flexion. The MRI findings include bone marrow edema located within the posterior talus or within the posterolateral talar process or os trigonum, a prominent posterior calcaneal process, and the posterior tibia a with downward sloping signal. Common soft tissue abnormalities include posterior capsule thickening, a fluid-distended posterior joint space, increased T2-weighted signal, or postcontrast enhancement along the posterior margin of the ankle that indicates synovitis and FHL tenosynovitis.45–47
The combined presence of bone marrow edema and posterior ankle synovitis may suggest the diagnosis of posterolateral ankle impingement (Fig. 5-8). The diagnosis can be confirmed by injection of 0.5 mL of a local anesthetic into the posterior soft tissue behind the peroneal tendon. If the pain is relieved by this small injection, the diagnosis is almost certain. The most common cause of posterolateral ankle pain is os trigonum syndrome. The differential diagnosis includes acute ankle injury causes, such as PTFL avulsion, fracture of the trigonal process (i.e., Shepherd’s fracture), and acute disruption of the os trigonum synchondrosis, and chronic injury causes, such as posterior capsule and adjacent soft tissue thickening, peroneal tendonitis, loose avulsion fragments of the posterolateral ankle ligament, and loose bodies. The talus is relatively plantar flexed and adducted, which causes further stress on the trigonal process by means of tension in the posterior talocalcaneal ligament in the pes planus foot. In cavus foot, the talus is supinated, moving the posterior surface medially and inferiorly and causing stress on the trigonal process by means of a tense PTFL.
Best and colleagues48 reported anomalous muscles caused posterolateral impingement. The peroneus quartus, which originated on the fibula separate from the peroneal muscles, extended distal to the level of the ankle joint and inserted onto the peroneal tubercle of the calcaneus. The peroneocalcaneus internus muscles arose from the posterolateral aspect of the FHL muscle, coursing along the lateral margin of the FHL tendon within the tendon sheath and inserting onto the distal aspect of the medial margin of the sustentaculum tali.48
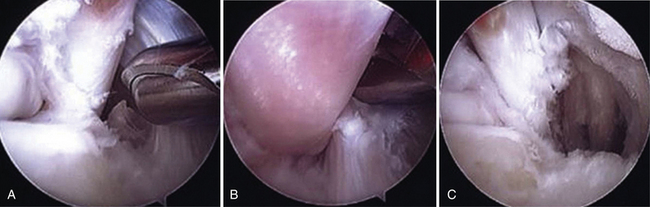
When local anesthesia does not relieve symptoms, the lesion should be treated by surgical excision. It should be stressed that the presence of an os trigonum usually is not a surgical problem; most athletes with os trigonum do not need to have them removed surgically. Surgical excision is indicated only after failure of conservative treatment. Abramowitz and colleagues49 reported the outcomes for resection of a symptomatic os trigonum with an open posterolateral approach. The postoperative American Orthopaedic Foot and Ankle Society (AOFAS) score averaged 87.6 points. Complications included a 19% rate of sural nerve sensory loss, which was temporary in four and permanent in four patients; a 2% rate of the superficial wound infection; and a 2% rate of reflex sympathetic dystrophy.49 The two posterior portal techniques provide excellent visualization of the posterior ankle structures, and the views obtained are superior to those in open procedures. The os trigonum may be separated and removed from the posterior talar process. Loose bodies and fragments of bone may be removed easily. The FHL tendon sheath may be released (Fig. 5-9).50
Posteromedial Ankle Impingement
Tendonitis of the FHL tendon behind the medial malleolus of the ankle is common in dancers (i.e., dancer’s tendonitis), but it also occurs in sports participants. It is often misdiagnosed as posterior tibial or Achilles tendonitis. The FHL passes through a fibro-osseous tunnel behind the talus between the medial and lateral tubercles to the level of the sustentaculum tali like a rope through a pulley. As it passes through this pulley, it is easily strained. The positions of en pointe and demi-pointe in ballet require the FHL tendon to function through an extreme range of motion while passing through its fibro-osseous tunnel.13
Frequent, prolonged repetitive motion of dance movements can lead to irritation and swelling of the FHL tendon. Chronic inflammation and hypertrophy of the musculotendinous unit within this tunnel can lead to painful stenosing tenosynovitis, analogous to de Quervain disease in the wrist. If a nodule or partial tear is present, triggering of the big toe may occur. This condition is known as hallux saltans. In severe case, the tendon may become completely frozen in the sheath, causing pseudohallux rigidus.
Physical examination findings include localized tenderness and swelling over the FHL sheath behind and lateral to the medial malleolus. Palpation of the sheath during active and passive motion of the hallux elicits the patient’s symptoms. Dorsiflexion of the first metatarsophalangeal joint can be reduced or absent when the ankle is in maximum dorsiflexion and the muscle fibers of the FHL are drawn into the FHL tunnel, producing a functional hallux rigidus (i.e., Thomasen’s sign) (Fig. 5-10). This finding is not always pathologic, and it may be present in asymptomatic patients. Usually, there is no pain with forced plantar flexion of the ankle. The differential diagnoses of posteromedial ankle pain are FHL tendonitis, soleus syndrome, posterior tibial tendonitis, and posteromedial fibrous tarsal coalition (Table 5-3). The muscles that adhere to the neurovascular bundles behind the medial malleolus arise from the gastrocnemius-soleus complex and insert onto the quadrates plantae muscle.48
TABLE 5-3 Differentiating Posterior Impingement Syndrome from Flexor Hallucis Longus Tendonitis
| Posterior Impingement Syndrome | Flexor Hallucis Longus Tendonitis |
|---|---|
| Posterior lateral | Posterior medial |
| Tenderness behind fibula | Tenderness over flexor hallucis longus tendon |
| Pain with plantar flexion of the ankle | Pain or triggering with motion of the hallux |
| Positive plantar flexion sign | Positive Thomasen’s sign |
| Mistaken for peroneal tendonitis | Mistaken for posterior tibial tendonitis |
From Hamilton WG, Chao W. Posterior ankle pain in athletes and dancers. Foot Ankle Clin. 1999;4:811-832.
The insidious onset of posteromedial ankle pain 4 to 6 weeks after a supination injury and tenderness in the posteromedial ankle in forced plantar flexion and inversion are diagnostic of posteromedial ankle impingement. The MRI findings include posteromedial capsular thickening, loss of striation of the PTTL, and posteromedial synovitis (Fig. 5-11).51 Injection of a steroid and long-acting anesthetic along with dry needling of the capsular abnormality allows most patients return to activity rapidly. Surgical resection of capsular thickening is successful in resistant cases.52
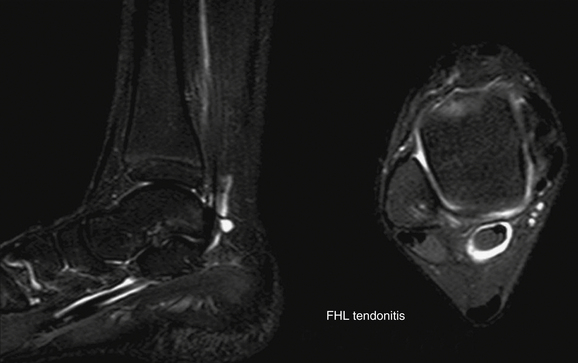
FIGURE 5-11 Magnetic resonance imaging shows posteromedial synovitis and flexor hallucis longus tendonitis.
Posterior ankle impingement can be treated by open or arthroscopic techniques. The open technique has a success rate of 73% to 90% and mean time to return to sporting activities or dancing of 3 to 6 months, but it has a complication rate of 12% to 24%.49,53 Arthroscopic treatment improves the success rate (good or excellent results for 80% of cases) and has a shortened recovery time (return to sport activities at 9 weeks) and a decreased complication rate (1% to 9%).54,55 The overall results for bony impingement appear to be better than those for soft tissue impingement.
Van Dijk and associates56 described the two-portal posterior endoscopic approach to the hindfoot with the patient in the prone position. It offered excellent access to the posterior compartment of the ankle joint, the posterior subtalar joint, the FHL tendon, and the os trigonum. It caused less morbidity and facilitated a quick recovery.56 Lijoi and coworkers57 verified the safety of a posteromedial portal in the arthroscopic treatment of the hindfoot.57 Phisitkul and colleagues58 showed the potential to increase the arthroscopic working area in the posterior subtalar joint. Horibe and associates59 described the posterolateral portal for arthroscopic visualization and the accessory posterolateral portal for insertion of instruments to excise a symptomatic os trigonum without any complications. Willits and coworkers reported the short-term clinical outcome for posterior ankle arthroscopy in the treatment of posterior ankle impingement. The excellent or good results were obtained for 93% of patients. The mean score on the AOFAS Ankle and Hindfoot Scale was 91, and the score on the AOFAS Lower Extremity Functional Scale was 75. Complications included temporary numbness in the region of the scar and temporary ankle stiffness.50
THE SUBTALAR JOINT
Sinus Tarsi Syndrome
Sinus tarsi syndrome (STS) was first described by Denis O’Connor. STS is a rare condition characterized by pain in the sinus tarsi that usually occurs after a sprain.60 STS has been associated with previous trauma, most commonly inversion ankle sprains.61 Clinically, it manifests as pain or tenderness over the sinus tarsi laterally. The diagnosis is confirmed by complete relief of pain by injection of a local anesthetic in the sinus tarsi. Subtalar pain often is present, and some investigators have confirmed a high incidence of STS on imaging studies.62
Several theories have been proposed to explain the cause of STS, including interosseous talocalcaneal ligament scarring or injury, synovial inflammation with impingement, and sensory nerve traction injury, but the true cause is not clear. Different diagnostic techniques have been proposed for the evaluation of STS, including arthrography, MRI, and local injection of anesthetic.63,64 However, the anatomy of the sinus tarsi, inconsistent inflammatory tissue and fibrosis, and chronicity of the problem make the diagnosis difficult.
Arthroscopy of the subtalar joint and sinus tarsi has provided another method of evaluation and treatment of this difficult problem. Investigators have described the results of arthroscopic débridement of the sinus tarsi for chronic pain in this area. Frey and colleagues65 reviewed subtalar arthroscopies, and of the 14 feet that had a preoperative diagnosis of STS, all the diagnoses were changed at the time of arthroscopy. The postoperative diagnoses included 10 cases of interosseous ligament tears, 2 cases of arthrofibrosis, and 2 cases of degenerative joints. The investigators thought that STS was an inaccurate term that should be replaced with a specific diagnosis.65
Lee and coworkers66 reported a rate of 88% for good or excellent results with arthroscopic treatment for STS. The mean score on the AOFAS Ankle and Hindfoot Scale improved from 43 preoperatively to 86 points postoperatively.66
Lateral Bony Impingement of the Subtalar Joint
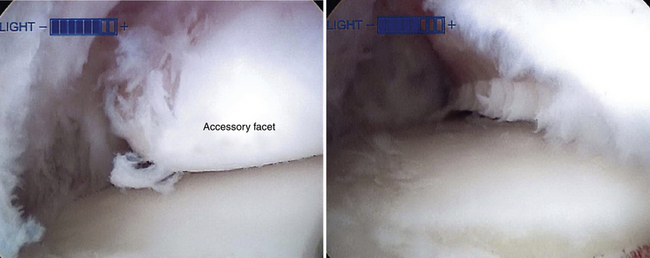
The accessory anterolateral facet was first described in a study of the astragalus by Sewell.67 The accessory anterolateral facet is associated with painful talocalcaneal impingement in cases of flatfoot deformity. The accessory anterolateral talar facet causes lateral bony impingement of the subtalar joint, as reported by Martus and colleagues.68 Sarrafian reported that a large accessory talar facet was found in 4% of 100 tali specimens. An accessory anterolateral talar facet was present in 34% of the specimens in a pediatric bone study.68 It was associated with male sex, a smaller angle of Gissane, and dorsal talar beaking. When subtalar eversion is removed, narrowing of the sinus tarsi is accentuated by the presence of a large accessory facet.68 Malicky and associates69 described CT imaging performed with the foot positioned in frames that simulated weight bearing in 19 patients with lateral talocalcaneal impingement. Impingement occurred between the lateral talar process and the calcaneal neck (Fig. 5-12).
Injection of an anesthetic to confirm the diagnosis is useful and easily performed. Arthroscopic resection is indicated when conservative treatment has failed (Fig. 5-13).
PEARLS& PITFALLS
PEARLS
PITFALLS
1. Bassett FH 3rd, Gates HS 3rd, Billys JB, et al. Talar impingement by the anteroinferior tibiofibular ligament. A cause of chronic pain in the ankle after inversion sprain. J Bone Joint Surg Am. 1990;72:55-59.
2. Ogilvie-Harris DJ, Gilbart MK, Chorney K. Chronic pain following ankle sprains in athletes. the role of arthroscopic surgery, Arthroscopy. 131997 564-574.
3. Biedert R. Anterior ankle pain in sports medicine. aetiology and indications for arthroscopy, Arch Orthop Trauma Surg. 1101991 293-297.
4. van den Bekerom MP, Raven EE. The distal fascicle of the anterior inferior tibiofibular ligament as a cause of tibiotalar impingement syndrome. a current concepts review, Knee Surg Sports Traumatol Arthrosc. 152007 465-471.
5. Watson AD. Ankle instability and impingement. Foot Ankle Clin. 2007;12:177-195.
6. Morris LH. Athlete’s ankle. J Bone Joint Surg Am. 1943;25:220.
7. McMurray TP. Footballer’s ankle. J Bone Joint Surg Br. 1950;32B:68-69.
8. Scranton PEJr, McDermott JE. Anterior tibiotalar spurs. a comparison of open versus arthroscopic débridement, Foot Ankle. 131992 125-129.
9. Tol JL, Verheyen CP, van Dijk CN. Arthroscopic treatment of anterior impingement in the ankle. J Bone Joint Surg Br. 2001;83:9-13.
10. van Dijk CN, Tol JL, Verheyen CC. A prospective study of prognostic factors concerning the outcome of arthroscopic surgery for anterior ankle impingement. Am J Sports Med. 1997;25:737-745.
11. O’Donoghue DH. Impingement exostoses of the talus and tibia. J Bone Joint Surg Am. 1957;39A:835-852. discussion, 852
12. van Dijk CN, Bossuyt PM, Marti RK. Medial ankle pain after lateral ligament rupture. J Bone Joint Surg Br. 1996;78:562-567.
13. Hamilton WG. Foot and ankle injuries in dancers. Clin Sports Med. 1988;7:143-173.
14. Parkes JC 2nd, Hamilton WG, Patterson AH, Rawles JGJr. The anterior impingement syndrome of the ankle. J Trauma. 1980;20:895-898.
15. Tol JL, Slim E, van Soest AJ, van Dijk CN. The relationship of the kicking action in soccer and anterior ankle impingement syndrome. A biomechanical analysis. Am J Sports Med. 2002;30:45-50.
16. Ferkel RD, Karzel RP, Del Pizzo W, et al. Arthroscopic treatment of anterolateral impingement of the ankle. Am J Sports Med. 1991;19:440-446.
17. Cutsuries AM, Saltrick Kr, Wagner J, Catanzarti AR. Arthroscopic arthroplasty of the ankle joint. Clin Podiatr Med Surg. 1994;11:449-467.
18. Haller J, Bernt R, Seeger T, et al. MR-imaging of anterior tibiotalar impingement syndrome. agreement, sensitivity and specificity of MR-imaging and indirect MR-arthrography, Eur J Radiol. 582006 450-460.
19. Hamilton WG. Sprained ankles in ballet dancers. Foot Ankle. 1982;3:99-102.
20. Ogilvie-Harris DJ, Mahomed N, Demaziere A. Anterior impingement of the ankle treated by arthroscopic removal of bony spurs. J Bone Joint Surg Br. 1993;75:437-440.
21. Amendola A, Petrik J, Webster-Bogaert S. Ankle arthroscopy. outcome in 79 consecutive patients, Arthroscopy. 121996 565-573.
22. van Dijk CN, Verhagen RA, Tol JL. Arthroscopy for problems after ankle fracture. J Bone Joint Surg Br. 1997;79:280-284.
23. van Dijk CN, Wessel RN, Tol JL, Maas M. Oblique radiograph for the detection of bone spurs in anterior ankle impingement. Skeletal Radiol. 2002;31:214-221.
24. Tol JL, Verhagen RA, Krips R, et al. The anterior ankle impingement syndrome. diagnostic value of oblique radiographs, Foot Ankle Int. 252004 63-68.
25. Robinson P, White LM, Salonen D, Ogilvie-Harris D. Anteromedial impingement of the ankle. using MR arthrography to assess the anteromedial recess, AJR Am J Roentgenol. 1782002 601-604.
26. Nikolopoulos CE, Tsirikos AI, Sourmelis S, Papachristou G. The accessory anteroinferior tibiofibular ligament as a cause of talar impingement. a cadaveric study, Am J Sports Med. 322004 389-395.
27. Wolin I, Classman F, Sideman S, Levinthal DH. Internal derangement of the talofibular component of the ankle. Surg Gynecol Obstet. 1950;91:193-200.
28. Hauger O, Moinard M, Lasalarie JC, et al. Anterolateral compartment of the ankle in the lateral impingement syndrome. appearance on CT arthrography, AJR Am J Roentgenol. 1731999 685-690.
29. Farooki S, Yao L, Seeger LL. Anterolateral impingement of the ankle. effectiveness of MR imaging, Radiology. 2071998 357-360.
30. Liu SH, Nuccion SL, Finerman G. Diagnosis of anterolateral ankle impingement. Comparison between magnetic resonance imaging and clinical examination. Am J Sports Med. 1997;25:389-393.
31. Rubin DA, Tishkoff NW, Britton CA, et al. Anterolateral soft-tissue impingement in the ankle. diagnosis using MR imaging, AJR Am J Roentgenol. 1691997 829-835.
32. Duncan D, Mologne T, Hildebrand H, et al. The usefulness of magnetic resonance imaging in the diagnosis of anterolateral impingement of the ankle. J Foot Ankle Surg. 2006;45:304-307.
33. Robinson P, White LM, Salonen DC, et al. Anterolateral ankle impingement. MR arthrographic assessment of the anterolateral recess, Radiology. 2212001 186-190.
34. DeBerardino TM, Arciero RA, Taylor DC. Arthroscopic treatment of soft-tissue impingement of the ankle in athletes. Arthroscopy. 1997;13:492-498.
35. Kim SH, Ha KI. Arthroscopic treatment for impingement of the anterolateral soft tissues of the ankle. J Bone Joint Surg Br. 2000;82:1019-1021.
36. McCarroll JR, Schrader JW, Shelbourne KD, et al. Meniscoid lesions of the ankle in soccer players. Am J Sports Med. 1987;15:255-257.
37. Hawkins LG. Fractures of the neck of the talus. J Bone Joint Surg Am. 1970;52:991-1002.
38. Valderrabano V, Perren T, Ryc C, et al. Snowboarder’s talus fracture. treatment outcome of 20 cases after 3.5 years, Am J Sports Med. 332005 871-880.
39. Liu SH, Mirzayan R. Posteromedial ankle impingement. Arthroscopy. 1993;9:709-711.
40. Paterson RS, Brown JN. The posteromedial impingement lesion of the ankle. A series of six cases. Am J Sports Med. 2001;29:550-557.
41. Lawson JP. International Skeletal Society Lecture in honor of Howard D. Dorfman. Clinically significant radiologic anatomic variants of the skeleton. AJR Am J Roentgenol. 1994;163:249-255.
42. Karasick D, Schweitzer ME. The os trigonum syndrome. imaging features, AJR Am J Roentgenol. 1661996 125-129.
43. Maquirriain J. Posterior ankle impingement syndrome. J Am Acad Orthop Surg. 2005;13:365-371.
44. Robinson P, Bollen SR. Posterior ankle impingement in professional soccer players. effectiveness of sonographically guided therapy, AJR Am J Roentgenol. 1872006 W53-W58.
45. Bureau NJ, Cardinal E, Hobden R, Aubin B. Posterior ankle impingement syndrome. MR imaging findings in seven patients, Radiology. 2152000 497-503.
46. Peace KA, Hillier C, Hulme A, Healy JC. MRI features of posterior ankle impingement syndrome in ballet dancers. a review of 25 cases, Clin Radiol. 592004 1025-1033.
47. Wakeley CJ, Johnson DP, Watt I. The value of MR imaging in the diagnosis of the os trigonum syndrome. Skeletal Radiol. 1996;25:133-136.
48. Best A, Giza E, Linklater J, Sullivan M. Posterior impingement of the ankle caused by anomalous muscles. A report of four cases. J Bone Joint Surg Am. 2005;87:2075-2079.
49. Abramowitz Y, Wollstein R, Barzilay Y, et al. Outcome of resection of a symptomatic os trigonum. J Bone Joint Surg Am. 2003;85:1051-1057.
50. Willits K, Sonneveld H, Amendola A, et al. Outcome of posterior ankle arthroscopy for hindfoot impingement. Arthroscopy. 2008;24:196-202.
51. Messiou C, Robinson P, O’Connor PJ, Grainger A. Subacute posteromedial impingement of the ankle in athletes. MR imaging evaluation and ultrasound guided therapy, Skeletal Radiol. 352006 88-94.
52. Koulouris G, Connell D, Schneider T, Edwards W. Posterior tibiotalar ligament injury resulting in posteromedial impingement. Foot Ankle Int. 2003;24:575-583.
53. Hamilton WG, Geppert MJ, Thompson FM. Pain in the posterior aspect of the ankle in dancers. Differential diagnosis and operative treatment. J Bone Joint Surg Am. 1996;78:1491-1500.
54. van Dijk CN. Hindfoot endoscopy. Foot Ankle Clin. 2006;11:391-414. vii
55. Ferkel RD, Small HN, Gittins JE. Complications in foot and ankle arthroscopy. Clin Orthop Relat Res. 2001;391:89-104.
56. van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16:871-876.
57. Lijoi F, Lughi M, Baccarani G. Posterior arthroscopic approach to the ankle. an anatomic study, Arthroscopy. 192003 62-67.
58. Phisitkul P, Tochigi Y, Saltzman CL, Amendola A. Arthroscopic visualization of the posterior subtalar joint in the prone position. a cadaver study, Arthroscopy. 222006 511-515.
59. Horibe S, Kita K, Natsu-ume T, et al. A novel technique of arthroscopic excision of a symptomatic os trigonum 121e1-121e4. Arthroscopy. 24 2008.
60. The American Academy of Orthopaedic Surgeons, O’Connor D. A new entity. sinus tarsi syndrome, J Bone Joint Surg Am. 401958 715-731.
61. Williams MM, Ferkel RD. Subtalar arthroscopy. indications, technique, and results, Arthroscopy. 141998 373-381.
62. Meyer JM, Garcia J, Hoffmeyer P, Fritschy D. The subtalar sprain. A roentgenographic study. Clin Orthop Relat Res. 1988;226:169-173.
63. Klein MA, Spreitzer AM. MR imaging of the tarsal sinus and canal. normal anatomy, pathologic findings, and features of the sinus tarsi syndrome, Radiology. 1861993 233-240.
64. Taillard W, Meyer JM, Garcia J, Blanc Y. The sinus tarsi syndrome. Int Orthop. 1981;5:117-130.
65. Frey C, Feder KS, DiGiovanni C. Arthroscopic evaluation of the subtalar joint. does sinus tarsi syndrome exist?, Foot Ankle Int. 201999 185-191.
66. Lee KB, Bai LB, Song EK, et al. Subtalar arthroscopy for sinus Tarsi syndrome. arthroscopic findings and clinical outcomes of 33 consecutive cases, Arthroscopy. 242008 1130-1134.
67. Sewell RB. A study of the astragalus. J Anat Physiol. 1904;38(Pt 4):423-434.
68. Martus JE, Femino JE, et al. Iowa Orthop J. 2008;28:1-8.
69. Malicky ES, Crary JL, Houghton MJ, et al. Talocalcaneal and subfibular impingement in symptomatic flatfoot in adults. J Bone Joint Surg Am. 2002;84:2005-2009.