Bone marrow aspiration and trephine biopsy
Bone marrow aspiration
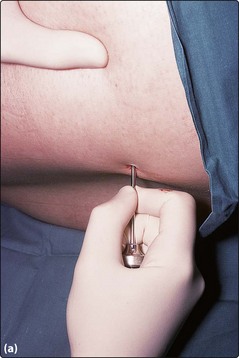
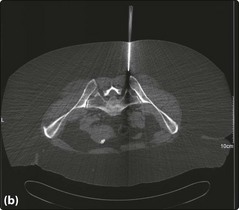
The patient lies in the left or right lateral position and the skin over the posterior iliac crest is cleaned with antiseptic prior to screening with sterile drapes. The crucial next stage is to properly identify the bony landmarks (Fig 53.1). This is straightforward in most patients but can be problematic in obese subjects. If there are real difficulties in locating the posterior iliac crest then the anterior crest or the sternum may be considered or the procedure may be performed under CT guidance. A local anaesthetic is infiltrated into the skin and then down to the periosteum. Before use it should be checked that the marrow aspirate needle stylet is easily withdrawn and the guard is removed (this is only required for sternal aspirates). The needle (Fig 53.2) is inserted through the skin and subcutaneous tissues at the site of local anaesthetic infiltration until the periosteum is encountered. It is pushed through the periosteum with a deliberate screwing motion (alternating clockwise and anti-clockwise) – a ‘give’ is felt as the marrow cavity is entered. The stylet is withdrawn and a syringe attached to the needle (Fig 53.3). Approximately 0.5 mL of marrow is aspirated into the syringe. The patient should be warned that this stage often causes pain but that it is momentary.
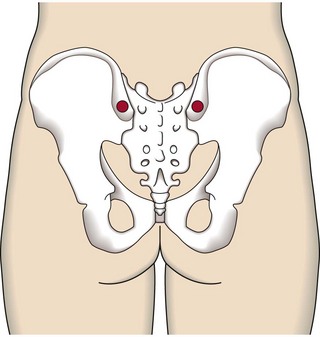
Fig 53.1 Anatomy of the posterior iliac crest.
Possible sites for marrow sampling are indicated in red.
Patients often ask how quickly the ‘results’ will be available. Aspirate slides can be processed for microscopy (see p. 19) within a few hours but most ancillary tests (Table 53.1) take longer.
Bone marrow trephine biopsy
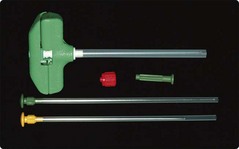
In practice the trephine procedure is usually performed immediately following the aspirate at the same site. It is helpful to enlarge the aspiration puncture site slightly with a scalpel blade. There is sometimes more prolonged discomfort than in the aspirate procedure and sedation is indicated in anxious adults, and a general anaesthetic is necessary in children. A number of different disposable needles are available – the Jamshidi type is illustrated in Figure 53.4. Smaller needles are available for paediatric use.
It is important to ensure that the device is complete and that the stylet can be easily withdrawn. The trephine needle is inserted in a similar fashion to the aspirate needle through the periosteum and approximately 0.5 cm into the cortex (Fig 53.5a) – when properly inserted the needle should easily support its own weight. The stylet is removed prior to advancing the needle 2–3 cm using the same oscillatory movement. The needle is aimed towards the anterior iliac crest. The method for breaking off the biopsy varies with the needle used. Some have devices designed to grip the biopsy and ensure its retention. The needle is then withdrawn taking care not to catch the skin and lose the biopsy in subcutaneous tissue. A special blunt probe is provided to push the biopsy out of the needle. The probe is inserted (with great care to avoid injury to the operator) at the sharp end of the needle so as not to traumatise the sample.