Chapter 27. Bone and joint injuries
Bone and joint injuries range from the relatively trivial to the life-threatening. The <C>ABC system must be followed. Only when life-threatening injuries have been excluded or treated should limb injuries be assessed.
Mechanism of injury
Fractures
Fractures may be classified in several ways. Injuries may be:
• Closed (simple), if the skin and soft tissues overlying the injury are intact, or
• Open (compound) if bacteria could have entered the wound through damaged skin.
When fractures are treated, wherever possible the normal anatomical alignment should be re-established. This reduces pain and bleeding and helps to prevent damage to adjacent structures. It is perfectly acceptable to reduce a bony fragment back into a wound in order to achieve this.
Fracture anatomy
After a bone has been fractured, the fragments may remain in their normal anatomical relationship to one another (undisplaced) or their relative positions may change (displaced).
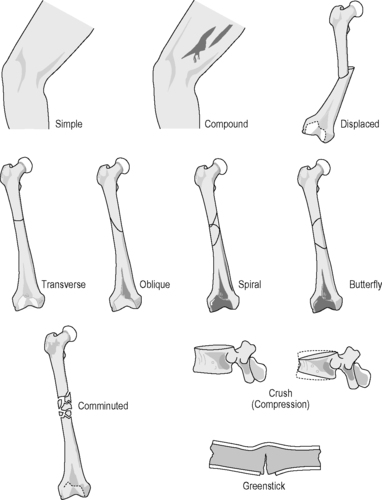 |
| Figure 27.1. |
| A classification of fractures. |
Fractures in children
Even although fracture patterns may differ in children, potential injuries should be assessed and managed in the same way as adults.
Dislocations
Dislocations may occur when similar forces are placed on joints, but the soft tissue structures fail before the surrounding bone fractures.
There are some injuries where fracture and dislocation occur at the same time; e.g. posterior dislocation of the hip with a fracture of the posterior lip of the acetabulum (hip socket). In this case, the acetabulum is fractured by the femur as it passes posteriorly, striking the lip.
General examination
The majority of fractures and dislocations are not immediately life-threatening, but exceptions include fractures of the pelvis, multiple closed fractures or compound fractures of long bones, where serious haemorrhage may occur.
Fractures of the skull and face may lead to airway obstruction or be associated with life-threatening neurological injuries. Fractures may co-exist with injuries to the vital thoracic or abdominal organs.
Limb-threatening injuries are much more likely. Many fractures and dislocations can lead to lifelong disability and thus are very important for the individual patient.
The multiply injured patient may require immediate transfer to hospital without full assessment or treatment of such injuries.
Examination of bones and joint must be systematic if injuries are to be identified (see box below).
Look – The part should be inspected for swelling, deformity and overlying wounds. Are there any pre-existing scars? The joint should be compared with the normal side
Feel – Is the injured part painful and if so, where? Is there any protective muscle spasm? Are the pulses distal to the injury intact?
Move – Can the patient move the injured part?
If there is a fracture then the sensation of grating of the bone ends may be experienced (‘crepitus’). This is extremely painful for the patient and deliberate attempts to elicit crepitus should be avoided.
Assess the limb for vascular injury. The palpation of a distal pulse alone is not sufficient. It is important to assess capillary refill in order to assess tissue perfusion.
The nail bed is compressed for 5 seconds. The pressure is released and the time taken for the return of the normal pink colour is measured. If this is greater than 2 seconds, then tissue perfusion is abnormal. The capillary refill test is best performed in good light and a warm environment.
A neurological assessment of sensation and muscle power should be made in order to determine whether there is a possibility of any nerve damage.
General treatment considerations
All patients who have sustained a long-bone injury should be given oxygen via a Hudson mask with a non-rebreathe valve and a reservoir bag at a rate of 15 L/min.
Analgesia
Entonox is excellent for fractures and dislocations sustained as sports injuries. Intravenous opiate analgesia will be required for significant fractures.
Compound fractures and serious wounds
Infection of a fracture is a disaster for the patient. Osteomyelitis can be controlled, but rarely cured. Good wound care starting at the scene of an accident will help reduce the incidence of this complication.
The fracture must be stabilised to avoid further damage to the soft tissues. Some form of immobilisation or splinting is required. Traction splinting will reduce blood loss, but must not be applied excessively if traction injuries to the nerves are to be avoided.
The wound should be covered in a sterile dressing, soaked in 0.9% saline or aqueous iodine solution. Life-threatening bleeding should be controlled by direct pressure.
Splinting a fracture or dislocation to prevent movement of the injured part is one of the best and simplest forms of pain relief
Simple splintage
Simple splintage of the lower limb may be achieved by securely fastening the injured part to the opposite uninjured leg using triangular bandages or a purpose-built splint.
The limb may be placed in a box splint which should be well padded and should be of the appropriate size for the injured limb.
Vacuum splints are even more effective.
Immobilise the joints above and below the fracture
Traction splintage
Traction splintage is generally employed for femoral shaft fractures. Modern traction splints work on the principle of traction at the ankle and countertraction via a ring at the ischial tuberosity, except for the Sager® splint (a padded T-bar that fits between the legs) which exerts countertraction on the symphysis pubis.
The principle is to reduce the fracture and overcome the deforming force of the surrounding muscles which are in spasm. The restoration of the normal length and shape of the limb also has the advantage of reducing blood loss by up to 20–30%.
Splints that apply traction to one (e.g. the Hare®, Donway® or Trac-Ill® splints) or both lower limbs (e.g. the Sager® splint) are effective.
Adequate splintage of a fractured limb will result in:
• Pain relief
• Reduction of blood loss
• Prevention of further soft tissue damage
• A reduced incidence of fat embolism.
Bone and joint injuries in specific regions
Skull, facial skeleton and cervical spine
Patients who have sustained a fracture to the skull or facial bones have sustained a serious head injury. The airway may be compromised, either directly owing to instability of the facial skeleton (e.g. an unstable fracture of the mandible) or owing to secondary factors such as swelling, bleeding or loss of consciousness. All patients with a head injury should be assessed for injury to the cervical spine.
There is a 5% chance of significant cervical spine injury in the unconscious patient
The airway must take priority, but all reasonable precautions to prevent cervical spine movement must be taken. Neck collars which are combined with immobilisation on a spinal board effect the most secure immobilisation when properly applied.
Pressure necrosis of the skin and soft tissues can be caused by even short periods on a spinal board.
Scoop stretchers can be used when transferring patients from the floor to a stretcher or bed.
The patient’s clothing must be checked for sharp or lumpy objects such as coins or wallets as these will quickly lead to the development of pressure sores in the immobilised patient. This is particularly important in the unconscious patient.
The upper limb
Fractured clavicle
Cause
Fall on the outstretched hand (FOOSH), when the forces transmitted up the upper limb may indirectly result in a fracture, or from a direct blow.
Signs and symptoms
Pain occurs at the site of the fracture whenever the upper limb is moved. The patient often supports the injured arm at the elbow in an attempt to reduce movement of the limb. There is usually swelling at the site of the fracture, which typically occurs at the junction of the outer (lateral) third and inner (medial) two-thirds of the bone.
Treatment
The upper limb should be immobilised in a broad arm sling. A collar and cuff should not be used, as this will act to separate the bony ends of the fracture due to the weight of the arm.
Potential problems
This is usually a straightforward injury to treat. The sling will often control the pain as it prevents movement at the fracture site. As with all limb injuries, there is a chance of damage to important vascular and neurological structures close to the fracture site. The subclavian artery and vein are in close proximity to the clavicle and although injury to them is rare, it can be serious. Similarly, the nerves that supply the upper limb may be injured, particularly when the fracture has been caused by direct rather than indirect force. Direct injury to this region may also result in chest injury and the assessment must not be confined to the clavicle.
Always check distal neurovascular function
Fractured scapula
Cause
Usually due to a direct blow, most commonly after a fall from a motorcycle, from a blunt weapon during an assault or accidentally during a sporting event with a stick or bat (e.g., a hockey stick). The scapula is surrounded by muscle and this is an unusual injury, considerable force being required.
Signs and symptoms
Pain occurs over the site of the fracture and may be made worse with movement of the upper limb.
Treatment
Immobilisation of the upper limb in a broad arm sling will reduce the discomfort.
Potential problems
There may be associated injuries to the thoracic cage and ribs and these need careful examination.
Dislocation of the sternoclavicular joint
Cause
Fall on the outstretched hand (FOOSH) or by direct injury to the anterior aspect of the shoulder, levering the medial end of the clavicle away from its usual articulation with the manubrium of the sternum.
Signs and symptoms
There is pain localised at the medial end of the clavicle, made worse by movement of the upper limb. There may be swelling and deformity over the sternoclavicular joint.
Treatment
The vast majority of these injuries are subluxations or partial dislocations. They are best treated in a broad arm sling.
Potential problems
Occasionally there is severe displacement. If the medial end of the clavicle has been dislocated posteriorly, then the major vessels are in danger of injury. The patient should be examined for signs of chest injury and shock. If there is evidence of shock, they should be considered to have a severe, potentially life-threatening injury and evacuated to hospital immediately. Intravenous access can be achieved in transit and any delay in reaching hospital should be avoided. Occasionally posterior dislocation of the sternoclavicular joint may produce airway obstruction: the clavicle should be pulled forwards, as a matter of urgency.
Dislocation of the acromioclavicular joint
Cause
Usually a fall onto the point of the shoulder. It is a common injury in rugby football. This injury results from partial or complete disruption of ligaments between the clavicle and the acromion and in severe cases also the ligaments between the clavicle and the underlying coracoid process of the scapula.
Signs and symptoms
Pain at the lateral end of the clavicle, made worse by attempting to carry any weight with the affected arm. There will be a variable amount of local swelling and usually a step is visible between the lateral end of the clavicle and the acromion (this is the expanded anterolateral process of the scapula which forms a bony roof over the shoulder joint and muscles and normally articulates with the clavicle).
Treatment
The upper limb should be immobilised in a broad arm sling.
Potential problems
The mechanism of injury should lead to a high level of suspicion of associated injuries to the cervical spine and nerves in the brachial plexus.
Anterior dislocation of the shoulder
Cause
Usually caused by forced external rotation of the glenohumeral joint (the joint between the humerus and the glenoid process of the scapula). Typically, this results from a fall or a mistimed rugby tackle. If the shoulder has previously been dislocated, then less force is required to produce a recurrent injury.
Symptoms and signs
The patient will be supporting the forearm with the elbow flexed. The shoulder will look abnormal (square contour) compared with the other side, with a loss of the usual rounded contour of the upper arm. The lateral edge of the scapula may well appear prominent. It is important to assess the sensory portion of the axillary nerve which provides sensation to the ‘regimental badge’ area of skin on the lateral aspect of the proximal arm.
Treatment
Treatment should be directed at immobilising the upper limb during transfer to hospital for relocation of the joint. An acceptable method is to allow the patient to sit upright and support the arm, perhaps resting it on a pillow. The sooner the joint is relocated the better.
Potential problems
The longer the joint is dislocated, the more permanent damage is done to the articular surface of the bone and to the soft tissues. All the nerves of the upper limb can be at risk. Damage to the major blood vessels may occur and proper examination and reexamination of the distal limb circulation is essential. Severe fractures and fracture-dislocations of the surgical neck of the humerus may mimic simple anterior dislocation.
Posterior dislocation of the shoulder
Cause
Often a fall on the outstretched hand with the arm internally rotated or a direct blow to the anterior aspect of the shoulder. An electric shock, epileptic fit or chronic muscle spasticity such as is seen in cerebral palsy can also cause posterior dislocation.
Symptoms and signs
These are similar to those of anterior dislocation, with pain, swelling and local deformity.
Treatment
The arm should be immobilised and the patient transported to hospital.
Potential problems
The nerves in the brachial plexus are particularly susceptible to damage due to pressure from the humeral head. Recognition and early relocation are essential. The X-ray changes are very subtle and this injury can be easily missed in hospital.
Inferior dislocation of the shoulder
Cause
Inferior dislocation is extremely rare but can follow a violent convulsion or an electric shock.
Symptoms and signs
The arm is held extended above the head and the injury is extremely painful. The condition is often bilateral.
Treatment
Analgesia and support during the transfer to the hospital are all that is required.
Potential problems
Fitting the patient onto the stretcher may be difficult.
Fracture of the proximal humerus
Cause
Usually either a fall onto the outstretched hand (FOOSH) or a direct fall onto the upper arm, particularly in elderly patients and those with osteoporosis. The fracture can occur in younger patients following direct violence.
Symptoms and signs
There is pain at the upper end of the arm. The patient will usually be supporting the arm at the elbow with the other hand. There may be obvious deformity. Swelling is almost immediate, but the severe bruising which accompanies this injury may not be apparent for several days and can track distally down the lateral aspect of the arm.
Treatment
The arm is supported in a broad arm sling initially. Once the diagnosis has been confirmed in the accident and emergency department, the sling should be changed to a ‘collar and cuff.’ This allows the weight of the arm to apply traction to the fracture and tends to reduce the fractured bone into its normal anatomical position.
Potential problems
As with all fractures, the surrounding nerves and blood vessels can be injured directly at the time of the fracture.
Fracture of the shaft of the humerus
Cause
The shaft of the humerus may be fractured through direct injury such as a fall onto the arm or a blow from a blunt weapon. Indirect force can cause these fractures, although the fracture pattern may be different.
Symptoms and signs
The arm is painful and may be supported at the elbow by the other hand. There may be obvious angular deformity, but rotational malalignment is not always obvious. There may be significant swelling and bruising. It is essential to examine the distal portions of the limb to exclude vascular and neurological injury.
Treatment
The arm should be supported in a broad arm sling.
Potential problems
The radial nerve runs in a groove, closely applied to the humeral shaft posteriorly. It may be damaged directly or secondarily due to swelling (compartment syndrome). Loss of radial nerve function may lead to weakness of the muscles that extend the wrist and as a result the patient will demonstrate ‘wrist drop’ (inability to extend the wrist). The arterial blood supply to the upper limb is via just one vessel at this point, the brachial artery. This artery may suffer direct injury or may be constricted owing to a compartment syndrome.
Supracondylar fracture of the humerus
Cause
Supracondylar fractures of the distal portion of the humerus just proximal to the elbow joint are common in childhood. They are typically caused by a fall onto the outstretched hand. The fractures can range from an undisplaced crack to a completely displaced injury with vascular and neurological damage.
Symptoms and signs
There is pain at the elbow after a fall. The child will support the elbow with the other hand. There may be obvious swelling and deformity and serious interference with the blood supply to the distal part of the limb.
Treatment
The arm should be immobilised in a broad arm sling in slight extension. Constant evaluation of the distal circulation is essential. If the circulation is compromised the elbow should be extended (straightened).
Potential problems
The brachial artery can be kinked over the bone ends, trapped between the bone ends or directly damaged by the fracture. If the circulation to the distal forearm is not restored then there is real danger of Volkmann’s ischaemic contracture (the death of all the muscle in the forearm), leaving a contracted, painful, useless arm. This can also be the result of compartment syndrome caused by swelling after this injury. Volkmann’s contracture is a serious injury which often leads to long-term disability.
Fracture of the radial head
Cause
Fall on the outstretched hand (FOOSH).
Symptoms and signs
There is pain over the lateral aspect of the forearm just distal to the elbow joint. There is often pain on rotation of the forearm (pronation and supination) and the elbow cannot be fully extended.
Treatment
The arm should be placed in a broad arm sling. Once the diagnosis has been confirmed at the accident and emergency department this may be replaced by a collar and cuff.
Potential problems
The distal circulation should be assessed, but this injury rarely leads to complications.
Fracture of the olecranon
Cause
Fall directly onto the elbow or from violent contraction of the triceps muscle in an attempt to extend the elbow against resistance.
Symptoms and signs
The elbow is very painful and there is considerable swelling. If the triceps tendon is still attached to the distal part of the ulna then it will still be possible to actively extend the elbow, although this will be very painful. If the attachment has been pulled off or is solely to the proximal fragment, then there can be no active extension of the elbow.
Treatment
The arm is immobilised in a broad arm sling. The distal neurological and vascular status is monitored.
Potential problems
The swelling may cause vascular insufficiency and compartment syndrome. There is a potential for damage to the nerves that cross the elbow joint. This is particularly true for the ulnar nerve which is closely applied to the medial side of the joint in the ulnar groove. Damage may lead to altered or lost sensation of the palmar surface of the small and ring fingers of the hand. It may also lead to loss of function of the small muscles of the hand with the exception of those that move the thumb.
Dislocation of the elbow
Cause
Fall on the outstretched hand. This injury may be associated with fractures of the distal humerus and/or the proximal radius and ulna.
Symptoms and signs
There is obvious deformity and gross swelling and the injury is usually very painful. Little movement is possible and attempts to do so are exquisitely painful. There is significant risk of vascular compromise due to swelling and neurological damage due to the stretching of the nerves at the elbow.
Treatment
The elbow should be immobilised in a well-padded splint. The distal circulation and neurological status require constant assessment.
Potential problems
The potential for vascular and neurological complications is high and the patient is best served by rapid transfer to hospital to enable early reduction of the dislocation.
Fractures of the shafts of radius and ulna
Cause
Falling on an outstretched hand may cause a fracture of both forearm bones, the radius and ulna. Direct injury such as a fall onto the forearm or a direct blow may also fracture both bones, but it is possible to fracture one or other in isolation. If one bone is fractured there is often an associated dislocation of the proximal or distal joint between the radius and ulna. Children may fracture the radius and ulna in the midshaft region or they may sustain a fracture involving the growth plate of the bones (epiphyseal injuries, see below).
Signs and symptoms
The forearm is painful and is supported by the other hand. There may be an obvious angular deformity.
Treatment
The arm requires immobilisation, which is best achieved using some form of splintage. However, if this is difficult to apply because of angulation or discomfort, then a broad arm sling may be appropriate. It is important that the sling prevents movement at the fracture site but that it does not compromise the circulation because it is too tight. It is almost impossible to apply a splint single-handed and attempts to do so may cause the patient unnecessary discomfort and even increase the soft tissue damage at the fracture site.
Potential problems
There is the ever-present possibility of circulatory compromise with these fractures and the distal portion of the limb must be regularly assessed. The skin and soft tissues directly overlying the fracture may be placed under tension if there is significant angulation. This may cause local skin ischaemia and necrosis. There is a real danger that closed fractures may become open if the forearm is not immobilised.
Fractures of the distal radius
Cause
Fracture of the distal radius is caused by a fall on the outstretched hand. This is particularly common in the elderly with osteoporotic bone resulting in Colles’ fracture with displacement of the distal fragment away from the palm (dorsally). Younger age groups can also sustain fractures of the distal radius. With children the injury is usually through the soft cartilage of the growth plate of the bone or epiphysis.
If the patient falls onto the back of the wrist with the forearm supinated then the distal fragment of the fracture may be displaced towards the palmar (volar or ventral) surface. This is known as a Smith’s fracture.
Symptoms and signs
There is pain and swelling at the wrist. If the distal fragment has been displaced dorsally there is said to be a ‘dinner fork’ deformity. If there is volar displacement of the fragment, there is said to be a ‘garden spade’ deformity. There may be symptoms of nerve injury in the palm of the hand. The median nerve is situated in the midline of the wrist and enters the hand via the carpal tunnel. It supplies sensation to the palmar surfaces of the thumb, index and middle fingers and supplies the motor branches to the small muscles of the thumb. It may sustain direct damage at the time of fracture or it may be compressed within the carpal tunnel owing to swelling or displacement of the fragments of the bone. The ulnar nerve may also be affected in fractures of the distal radius, but less frequently than the median nerve. The ulnar nerve supplies sensation to the little and ring fingers and motor branches to the remainder of the small muscles of the hand.
Treatment
The distal radius must be immobilised. A broad arm sling may be sufficient in some cases, a short box splint or vacuum splint may be used as alternatives. The sensation and circulation to the hand and fingers must be monitored.
Potential problems
The nerve injuries outlined above may cause symptoms. The hand must be examined to exclude vascular damage. If there is massive swelling then the hand and wrist should be elevated after the fracture has been immobilised.
Fractures of the carpal bones
Cause
Fractures of the carpal bones are caused by a fall on the outstretched hand. Scaphoid fractures (the most common) are caused when the wrist is forced into hyperextension.
Symptoms and signs
The wrist is painful with reduced movements. There may be no significant swelling.
Treatment
The arm should be placed in a broad arm sling.
Potential problems
If fractures of these bones are missed and not immobilised in plaster, the fracture may fail to unite and the patient will be left with a stiff wrist.
Fractures of the metacarpals and fingers
Cause
Injuries to the metacarpals and fingers are usually caused by direct falls or blows.
Symptoms and signs
The injured bone will be painful. There may be considerable swelling on the dorsum (back) of the hand. The palmar skin is firmly attached to the bony skeleton of the hand to allow good grip but the dorsal skin is loose and thus bruising and swelling track dorsally. There may be obvious bony deformity. The fifth metacarpal is most commonly broken, often as a result of a punch.
Treatment
The hand should be elevated in a high arm sling.
Potential problems
The blood supply to the digits may be compromised, either directly as a result of the injury or secondary to swelling. Rings should always be removed from an injured hand. If it is not possible to remove them prehospital then their presence must be communicated to the staff in the accident and emergency department so that arrangements can be made to cut the rings off. Failure to remove rings may lead to swelling, circulatory compromise and even loss of the digit. This applies to rings on uninjured digits because they will subsequently swell in any hand injury.
Dislocation of the fingers
Cause
Finger dislocation is usually caused by direct injury, for instance by a blow from a cricket ball.
Symptoms and signs
There is obvious deformity of the joint, which is painful.
Treatment
It is often said that these dislocations should be reduced quickly, without anaesthesia. This is not appropriate. Relocation of these joints is not always straightforward and there may be a fracture associated with the dislocation. It is better to transport the patient to the accident and emergency department where a fracture can be excluded by X-ray and reduction can performed painlessly under a ring block or other regional anaesthesia.
The thoracic skeleton
Fractures of the ribs and flail chest
Cause
Rib fractures are usually a result of direct trauma. They may be multiple.
Symptoms and signs
The fractured rib is painful. Clearly it is not possible to stop moving the injured rib without stopping breathing. Thus, pain is experienced with each inspiratory and expiratory movement. If there have been fractures of more than one rib in more than one place, then a segment of the thoracic cage may move independently of the main chest wall. This is referred to as a flail segment (flail chest). A flail segment will exhibit paradoxical movement; that is, it will move in the opposite direction to the rest of the chest wall. This has significant consequences for the ventilation of the underlying lung. Patients with significant chest injuries will have an abnormal respiratory rate (usually high).
A fractured rib may result in blood loss of up to 150 mL. Multiple rib fractures may therefore be a significant contributory factor in hypovolaemic shock.
Treatment
The patient must be given high-flow oxygen (15 L/min) through a mask with reservoir bag. Large flail segments may be treated by lying the patient on the injured side (remembering the cervical spine precautions) or by strapping the chest. If the patient is shocked then an intravenous infusion should be started, but this must not delay transfer to hospital.
Record the respiratory rate and monitor changes
Fractures of the sternum
Cause
Fractures of the sternum are characteristically caused when the chest strikes the steering wheel in a decelerating vehicle. The correct use of seatbelts, and more recently, the deployment of air bags during an accident, has prevented many of these injuries.
Symptoms and signs
There is pain in the anterior aspect of the chest. There may also be symptoms and signs of other significant chest injury.
Treatment
It should be assumed that there is also myocardial contusion. The patient should receive oxygen by face mask (15 L/min through mask with reservoir bag). Monitoring of the pulse, blood pressure, respiratory rate, ECG and oxygen saturation are mandatory. Intravenous access should be obtained following normal protocols. Urgent transfer to hospital is essential.
Potential problems
The main problem with these fractures is not the bony injury but contusion or bruising of the heart which lies just posterior to the sternum. This injury requires careful cardiac monitoring and observation in hospital. If cardiac arrhythmias occur they require urgent treatment.
The pelvis
Minor pelvic fractures
Fractures of the pubic ramus
Cause
The cause of a fracture of the pubic ramus is usually a fall, particularly in an elderly patient.
Symptoms and signs
The patient will complain of pain in the hip. Careful elucidation of the site of the pain will reveal that it is in fact groin pain. There is no external rotation or shortening of the leg. The patient is usually unable to walk. The injury is frequently confused with fracture of the femoral neck and correct differentiation of the two may only be possible on X-ray.
Treatment
The patient requires supportive treatment and transfer to hospital.
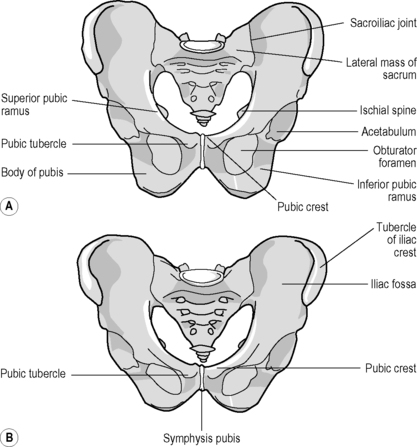 |
| Figure 27.2. |
| Anatomy of the bony pelvis. (A) male; (B) female. |
Avulsion fracture of the pelvis
Cause
Many powerful muscles have attachment to the pelvis (for example, the hamstring muscles). Strong contraction of these, perhaps during sporting activity, may lead to an avulsion fracture (where the muscle inserts onto bone, a small fragment of bone is pulled off).
Symptoms and signs
The patient experiences acute pain after a muscular effort and may be unable to stand or walk. The symptoms are similar to those of a severe pulled muscle.
Treatment
The patient will need analgesia and should be transferred to hospital for assessment.
Major pelvic fractures
Cause
Major pelvic fractures are usually caused by severe violence. Falls directly onto the pelvis or force transmitted down the femoral shaft are common causes; direct injury by a heavy weight falling on the pelvis can also be responsible. The pelvis can be considered as a ring and usually fails in at least two places. The fracture pattern is dependent on the mechanism of injury.
Symptoms and signs
The patient will be in pain. There may be a leg length discrepancy in pelvic fractures with a vertical shear fracture. Major blood vessels lie on the inner pelvic surface anterior to the sacroiliac joint and pelvic fractures can be complicated by life-threatening haemorrhage. The patient must be examined and assessed for signs of hypovolaemia. The pelvic organs are also at risk of severe injury. The male patient may have blood at the tip of his penis and swelling of the scrotum as a result of rupture of the urethra. The pregnant woman will be susceptible to uterine rupture or detachment of the placenta (abruptio placentae). She will also mask the signs of hypovolaemia because she has a proportionately greater blood volume in pregnancy.
Treatment
The diagnosis of a major pelvic fracture may be made when instability is found on pelvic assessment during ‘C’ of the primary survey. The absence of obvious instability does not exclude the diagnosis which may be suspected from the mechanism of injury or in a shocked patient where no other obvious source of bleeding is identified. Avoid attempts to ‘spring’ the pelvis, as this may precipitate or exacerbate haemorrhage. The patient should receive high-flow oxygen (15 L/min through a mask with reservoir). Haemorrhage can be fatal and an external fixator may need to be applied as an emergency at hospital. Any delay will be detrimental to the patient, who must be transported to hospital quickly. Intravenous access should therefore be obtained during transit or, for short transit times, after arrival in hospital. If it is possible the pelvis should be stabilised during transfer. Pelvic ‘wrap-around’ splints (e.g. the SAM splint) have been proven to improve alignment and reduce bleeding in complex pelvic fractures.
Potential problems
Severe hypovolaemic shock may lead to pulseless electrical activity dissociation and death. The patient may also have sustained other life-threatening injuries which must be identified and treated.
Types of major pelvic fracture
Femoral acetabular fractures
Cause
Fractures usually occur when force is transmitted indirectly from the femoral shaft. This is a high-violence injury and usually follows a road traffic accident or a fall from a height. The exact injury will depend on the position of the femur. If the hip is flexed or extended then it will usually dislocate, perhaps fracturing the rim of the acetabulum. However, if the hip is in neutral then the force is transmitted directly to the acetabulum which will fracture.
Symptoms and signs
The patient will be in pain which is made worse by any attempt to move the leg. The leg may be short, adducted and internally rotated (see Dislocated hip, below). There may be extensive haemorrhage and thus the patient may show signs of shock.
Treatment
The patient should be given high-flow oxygen. An intravenous infusion should be started if this does not delay transporting the patient to hospital. The injured leg should be supported by splinting it to the other leg.
Potential problems
The patient may have sustained other life-threatening injuries which must be identified and treated. If there has been displacement of the femoral head into the pelvis then there may be severe haemorrhage and damage to other pelvic organs.
The lower limb
Fractured neck of the femur
Cause
Fracture of the neck of the femur occurs in the elderly population. A fall or twisting injury may result in this injury. Some children (often overweight adolescents) have a condition where the upper femoral growth plate slips. Minor trauma in these children may precipitate a complete slipped epiphysis which has similar signs and symptoms to fractured neck of femur.
Symptoms and signs
The hip is painful. There may also be referred pain to the knee of the same side. The leg may be shorter than the normal side and may lie in external rotation. All movements of the hip joint cause pain. It is often the case with the elderly person who lives alone that the patient has been lying on the floor for some time since the injury. This increases the possibility of chest infection, pressure necrosis to the skin and hypothermia. The elderly patient may have had some medical event to cause the fall in the first instance (e.g. a myocardial infarction).
Treatment
The leg should be immobilised during transfer to hospital. This is best achieved by using some form of strap or bandage to tie the injured leg to the normal one.
Potential problems
The patient may have been on the floor for some time. Underlying medical problems may require urgent treatment. Egress from the patient’s home may be difficult. Analgesia will be required but must be used judiciously in the frail, elderly patient. Fluids can usually wait until hospital.
Dislocation of the hip
Cause
Hip dislocation is caused by a high-energy injury. Typically, the knee is struck when the hip is flexed, for example on the dashboard of a car in a high-speed road traffic collision. Posterior dislocation is most common and there is often an associated fracture of the lip of the acetabulum (see above). If the hip is in the extended position at the time of injury anterior dislocation may occur. Hip prostheses are particularly vulnerable to dislocation.
Symptoms and signs
The hip is painful. There may be referred pain down the thigh and in the knee joint. The hip is held flexed and adducted and the leg is internally rotated. There may be associated sciatica. Other life-threatening injuries are extremely likely and examination should identify these urgently.
Treatment
The patient should be given oxygen. It is not possible to place the femur in the normal position until reduction is performed under anaesthesia. Attempts to reduce the dislocation without anaesthesia will be fruitless, extremely painful and delay the patient at the scene. The injured leg should be immobilised by securing it to the uninjured side and the patient transported to hospital as soon as possible. The distal circulation should be monitored. Analgesia will certainly be required. If the patient is trapped then medical assistance should be requested. If the patient is responsive intravenous opiates will probably be required in addition to Entonox.
Potential problems
The mechanism of injury is such that the patient may have multiple injuries. There is considerable disruption to the muscles and soft tissues around the hip joint, leading to haemorrhage. The patient must be monitored and treated for hypovolaemic shock where appropriate but this should not delay transfer to hospital. Good analgesia is essential. The head of the femur will compress the sciatic nerve as it leaves the pelvis which may lead to temporary or permanent damage. If the displacement of the joint is significant then the femoral vessels may become kinked and the distal circulation threatened. It can be difficult to extricate a patient with this injury, even if the vehicle damage is minimal, and good liaison with the fire and rescue services will be essential.
Fracture of the shaft of femur
Fracture of the shaft of the femur is always a major injury.
Cause
Fractures of the femoral shaft are usually the result of high-energy injury, such as a road traffic collision or a fall from a height.
Symptoms and signs
The exact symptoms and signs will depend on the level of the fracture. There will be pain and usually swelling at the site of the injury. There is often some degree of deformity, which may be rotational or angular. The leg may be short. The distal circulation may be compromised. Other coexistent life-threatening injuries should be identified and treated.
Treatment
The patient should receive high-flow oxygen (15 L/min through a mask with reservoir). An intravenous infusion should be started particularly if there is a delay before the patient can be transferred to hospital; otherwise it may be commenced en route. Intravenous opiate analgesia will be required. A regional nerve block (femoral nerve block) may be administered by an immediate-care doctor. Some form of splintage is required: the best splintage will be afforded by a traction splint, but if this is not easily applied or unavailable then a long leg splint (box splint, lollipop splint) or splinting to the other leg will suffice.
Potential problems
Hypoxia must be avoided. Other major injuries must be identified and treated. A femoral fracture may lose up to 1500 mL blood. This may be doubled in a compound injury. The patient should be monitored for the signs of shock and treated with fluids or urgent evacuation. It should be remembered that the infusion volumes achievable in hospital are far greater than those at the roadside. Minimal delay is essential. It may not be possible to immobilise a badly displaced fracture without manipulation.
Fractures of the patella
Cause
Fracture of the patella (kneecap) may be sustained in a number of ways. The knee may strike the dashboard in a road traffic accident or it may strike the floor in a fall. Alternatively, a heavy object falling on the knee may cause a patella fracture, as may violent contraction of the quadriceps tendon.
Signs and symptoms
The knee is painful and swollen. There may be a laceration or abrasion over the patella. If the fracture is displaced, it may be possible to feel the gap between the ends of the patella. The extensor mechanism of the knee consists of the quadriceps tendon superiorly, the patella and the patella tendon inferiorly. The latter attaches to the tibia at the tibial tubercle which can be felt 4–5 cm below the patella. If any of these soft tissue or bony structures are disrupted then the knee cannot be extended.
Treatment
The leg should be placed in a well-padded, long leg splint.
Potential problems
A careful history will ensure that potentially serious associated injuries can be identified and treated.
Dislocation of the patella
Cause
The patella may dislocate with minor trauma. The patient will often have experienced this injury previously. The patient typically complains of a dislocated knee secondary to relatively minor trauma.
Symptoms and signs
The patella almost always dislocates laterally. The acute injury is usually painful. The knee appears abnormal with the patella located over the lateral femoral condyle. There may be swelling (effusion) inside the joint. The patient will not be able to move the joint.
Treatment
Analgesia with Entonox may be sufficient to allow relocation of the patella. The important manoeuvre is to extend (straighten) the knee while pressing the kneecap medially. It will be very difficult to reduce while the knee is flexed (bent). If one attempt fails then the leg is placed in a long leg splint and the patient transported to hospital. If the patella is successfully relocated, hospital consultation is still required as the patient will need orthopaedic follow-up.
Potential problems
This condition can be extremely painful and the patient may not tolerate a splint.
Dislocation of the knee
Cause
Dislocation of the knee is a rare and serious injury which inevitably means that the majority of the ligaments of the knee have been disrupted. The vessels and nerves to the distal portion of the limb are frequently compromised. A great degree of force is required.
Symptoms and signs
The knee will be painful and swollen. There may be significant angular deformity of the joint, although elastic recoil may have returned it to an anatomical position. The disruption of the ligaments and capsule renders the joint unstable. There is a serious possibility of vascular and neurological deficit to all structures below the knee.
Treatment
The vascular status must be assessed and monitored. The leg should be placed in a long leg splint.
Potential problems
The joint is unstable and may have few ligamentous and capsular attachments remaining. Redislocation of the joint may further damage the vascular and neurological structures. When placing the leg in the splint, the limb must be supported above and below the knee.
Soft tissue and ligament injuries to the knee joint
Cause
Injuries to the ligaments of the knee joint are common and are frequently sustained during sporting activities such as football, rugby and skiing. Damage to the menisci of the knee (commonly known as ‘cartilages’) can occur in isolation or in concert with such ligament injuries. A common mechanism of injury is a twisting injury to the knee when the foot is fixed.
Symptoms and signs
The knee will be painful. It may swell immediately (if there is bleeding into the joint, a haemarthrosis), or over the next 12–24 hours (an effusion). It is important to ascertain the exact mechanism of injury as this will help the medical staff make the diagnosis.
Treatment
The leg should be immobilised in a long leg splint until a fracture has been excluded in hospital. The distal circulation should be assessed and monitored.
Potential problems
The joint may be potentially unstable when severe ligament disruption has occurred.
Fractures of the tibial plateau
Cause
Fracture of the tibial plateau is caused by a large valgus force (the lower tibia is forced away from the midline) or varus force (the lower tibia is forced towards the midline).
Symptoms and signs
There is pain at the knee and often a haemarthrosis (bleeding into the joint). The patient is unable to walk.
Treatment
The limb is immobilised in a well-padded splint.
Potential problems
The patient should be examined for other major injuries and the distal circulation monitored.
Fractures of the tibial shaft and fibula
Cause
Fractures of the tibial shaft and fibula may be caused by direct injury, such as in road traffic accidents and sporting injuries. In some cases of direct injury either the tibia or fibula may be fractured in isolation. Longitudinal compression as a result of a fall may lead to these fractures and they may also result from indirect torsional forces caused by rotation transmitted from the foot or from the upper body if the foot is fixed. Finally, the tibia may fracture as a result of completion of a preexisting stress fracture.
Symptoms and signs
There is localised pain and swelling. There may be angular or rotational deformity. The distal circulation may be compromised.
Treatment
Oxygen should be given (15 L/min). Hypoxia is common after tibial fractures and must be avoided. Similarly, there may be considerable haemorrhage. The patient must be examined for circulatory shock and monitored. An intravenous infusion should be started without causing undue delay in transferring the patient to hospital. The injured limb should be immobilised in a long leg splint.
It may be necessary to reduce the fracture before immobilisation is possible and therefore opiate analgesia is required. Only then should the limb be subjected to gentle longitudinal traction to reverse any shortening caused by muscle spasm and overlap of bone. Once limb length, rotation and angular deformity are corrected, the fracture will be in a near reduced position. Excessive traction must be avoided as this may lead to secondary injury to the vessels and nerves. Accurate fracture reduction will reduce the amount of haemorrhage at the fracture site and from the soft tissues.
Potential problems
The tibia is a subcutaneous bone. It is easy to convert a simple fracture to a compound fracture by careless handling of the limb. The vascular supply of the lower parts of the limb may become compromised.
There is a significant risk of compartment syndrome following fracture of the tibia. The muscles of the lower legs are enclosed in tough fibrous sheaths. If bleeding occurs into these compartments or if there is significant swelling following a soft tissue injury, then the pressure within the compartment will rise. The risk is highest when there is a closed fracture or a soft tissue injury such as a muscle haematoma following a kick. As the pressure rises, perfusion of the tissues and cells decreases and they are starved of oxygen. The pressure in the arteries may be high enough to allow continued flow into the compartment, making the situation worse. The presence of a palpable distal pulse does not guarantee that the tissues are adequately perfused. The capillary refill test must be performed to allow a more complete assessment of the vascular status of the tissues.
Fractures and dislocations of the ankle
Cause
The exact pattern of fracture depends on the mechanism of injury, but the prehospital treatment is identical regardless of the fracture type. The typical history is of ‘going over’ on or ‘twisting’ the ankle, which may be combined with a fall down a kerbstone or step. These injuries are usually referred to as inversion or eversion injuries. Injuries of this kind are also common on the sports field. The ankle may be trapped by the foot pedals in a motor vehicle or a fall may lead to a fracture or dislocation of the ankle.
Symptoms and signs
The ankle is extremely tender over the fracture site and swelling occurs rapidly. In general, eversion injuries are associated with fractures of the medial malleolus and inversion injuries with fractures of the lateral malleolus. In severe injuries, both may fracture. Any attempt at walking is painful. There may be associated deformity. Distal nerve or vessel injury may occur.
Treatment
The ankle should be immobilised in a well-padded splint – this will probably require analgesia. The neurological and vascular status of the foot must be carefully monitored. Dislocation of the ankle may occur with obvious deformity. This is a limb-threatening emergency requiring rapid reduction. Urgent transfer to hospital (or reduction on scene by a doctor in remote areas) is essential. With an unstable injury, the act of splinting the joint may lead to reduction. However, reduction often requires sedation and intravenous analgesia.
Potential problems
If there is significant deformity following this fracture then the skin overlying the joint can become tightly stretched over the bony fragments. This will quickly lead to pressure necrosis and death of that skin. Penetration of the skin converting a closed to an open injury must be avoided.
At times it can be difficult to distinguish between a fracture and a sprain of the ankle. Typically the pain and swelling of a sprain to the anterior talofibular ligament are distal and anteromedial to the lateral malleolus. If there is any doubt about the diagnosis it is best to treat these injuries as fractures until they have been assessed at hospital.
Fractures of the talus and calcaneum (os calcis)
Cause
The talus is situated between the lower tibia (and forms part of the ankle joint) and the calcaneum or os calcis (heel bone). Both these bones are vulnerable to fracture as a result of falls from a height. They can also fracture when struck or trapped by foot pedals in a motor vehicle.
Symptoms and signs
There is pain on attempts to walk or on direct palpation. There may be significant deformity if these fractures are associated with dislocation of either the ankle or the midfoot joints.
Treatment
The ankle and foot should be placed in a well-padded splint and elevated. The circulation to the foot should be monitored and the neurological state assessed.
Potential problems
The mechanism of injury usually causes associated injuries. A fall from a height may produce fractures of the calcaneum, talus, femoral neck, acetabulum and vertebrae and a thorough secondary survey is mandatory, although this will usually be deferred until the patient arrives in hospital.
Dislocations of the midfoot
Cause
Midfoot dislocations result from a fall from a height, landing on the foot with the toes pointing downwards.
Symptoms and signs
The deformity is usually obvious, although it may be obscured by the footwear, and swelling will occur quickly. There may be associated vascular injury, either directly or indirectly, because of a compartment syndrome.
Treatment
The paramedic should not attempt to relocate the dislocation at the scene. The foot should be placed in a well-padded splint and elevated and the patient evacuated to hospital. The circulation to the distal part of the foot must be assessed and recorded.
Potential problems
The possibility of other associated serious injuries should not be forgotten.
Fractures of the metatarsals and toes
Cause
Fractures of the metatarsals and toes can be caused by direct blows, falls and even by overuse (e.g. the ‘march fracture’ of the second metatarsal seen in army recruits unused to marching in boots). Overuse injuries will rarely present to the ambulance service as an emergency.
Symptoms and signs
There is pain over the fracture which is made worse when attempting to walk. The foot swells dorsally (the top surface), an analogous situation with hand injuries.
Treatment
The foot should be elevated. A splint is not always required, but when used it should be well padded.
Potential problems
The main problem is swelling which may compromise the circulation, particularly of the digits.
Traumatic amputation
Traumatic amputation can range from a relatively minor fingertip injury to a life-threatening avulsion of a limb. Recent improvements in microsurgical techniques have increased the likelihood of successful reimplantation of the amputated part.
In order to minimise the damage to the amputated part and thus improve the chances of successful surgery, the following steps should be performed.
• The time of amputation should be recorded
• The amputated part should not be placed in water or directly in ice, as this can cause further cellular damage
• The amputated part should be securely wrapped up in a sealed plastic bag, which should be placed in a second bag, and the double-wrapped part kept cool. It is safe to place the part in an ice-water mixture after wrapping it in this way as direct contact is avoided
• If the patient is still trapped then the part should be clearly labelled and sent to the receiving hospital after discussion with the medical staff who will be receiving and treating the patient.
However damaged the amputated part is, it should always be transported to hospital with the patient. Even if reimplantation is not possible, use of the skin for grafting may be considered.
Complications of fractures
The complications of any injury can be divided into immediate, early and late.
Immediate complications
• Haemorrhage
• Vascular injury
• Nerve injury.
Early complications
• Compartment syndrome
• Infection
• Fat embolism.
Late complications
• Reflex sympathetic dystrophy
• Osteomyelitis
• Non-union
• Malunion
• Arthritis.
For further information, see Ch. 27 in Emergency Care: A Textbook for Paramedics.



