Chapter 4 Blood-pressure generation
Together with heart rate, pulsatile blood pressure is the most readily accessible measure of cardiovascular performance in humans. Blood pressure rises with sympathetic activation and this pressor response plays a vital role in optimizing blood flow to muscle and other vital organs during exercise. It is, therefore, important to spend a little time considering the factors that determine the limits of pressure pulsation and how these will be affected by increased sympathetic drive. The changes in blood pressure that occur during exercise will be examined in more detail in Chapter 7.
FACTORS AFFECTING BLOOD PRESSURE
Limits to blood pressure
Systolic pressure
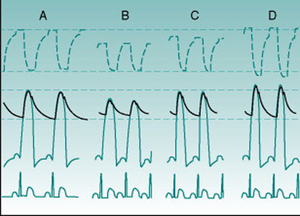
The extent to which blood pressure rises during systolic ejection reflects how much the energy of ejection is able to compress the arterial contents downstream of the left ventricle. The size of the stroke volume is, therefore, one obvious factor that will influence the level of systolic blood pressure (SBP). Anything that reduces stroke volume will reduce SBP (Fig. 4.1A,B). In normal individuals, the most usual situations in which this occurs is when cardiac filling falls because of an increase in heart rate or reduced venous return, typically during postural change.
Generalised sympathetic nervous system activation elevates SBP, due to a variety of factors. First, increased cardiac muscle contractility reduces end-systolic ventricular volume and increases stroke volume. Second, an increased action potential conduction velocity through the ventricular myocardium leads to faster compression of the contents and, therefore, to a higher velocity of ejection. In addition, the smooth muscle in the proximal aorta receives a sympathetic innervation and contraction of these muscle cells reduces aortic compliance. This stiffening allows all of the energy of ejection to be used in pressure generation. Finally, sympathetic vasoconstrictor drive to veins stiffens these and mobilizes blood normally stored in the venous reservoir back into active circulation, aiding cardiac filling and further increasing stroke volume. The additive effects of these factors are illustrated in Figures 4.1C and D.
Diastolic pressure
As diastolic blood pressure (DBP) represents the lowest value to which pressure falls in the arteries before the next systolic ejection, it must be influenced by the period over which the pressure can fall, so heart rate itself is also a major determinant of DBP, with tachycardia predictably causing a pressure rise (Fig. 4.1). Heart rate changes will also affect SBP if pulse pressure remains constant but, in practice, the consequences of heart rate alteration for ventricular filling time and, therefore, for stroke volume tends to minimize SBP changes.
The second main influence on DBP is the rate at which intra-arterial pressure falls after systolic ejection ceases; that is, how fast the pressurized blood flows out through the resistance of the peripheral blood vessels. Thus, the total peripheral resistance is a major determinant of DBP and changes in DBP can in many situations be used as an index of peripheral resistance changes. While all vascular beds and all segments of the vasculature contribute to the overall resistance of the system, most of the peripheral resistance occurs in the largest regional vascular beds, those supplying the digestive tract and associated tissues (the splanchnic circulation), the skeletal muscles, the skin and the kidneys, and almost all is localized to the arteriolar segment of the vasculature. In Chapter 5 (p. 50) we will see why the arterioles produce so much more resistance to flow than do other parts of the vascular tree.
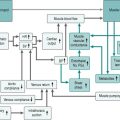
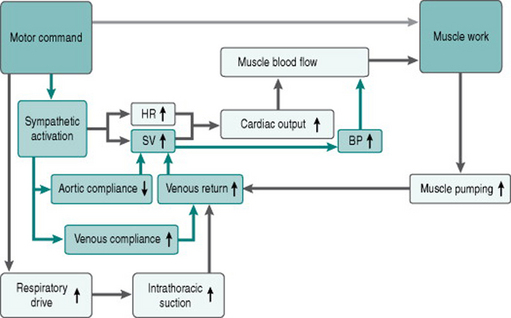
Figure 4.2 adds the effects of sympathetic activation on cardiac generation of blood pressure to our flow chart of the exercise response.
Mean versus phasic arterial pressure
As indicated above, the phasic limits of blood pressure can provide valuable information on the behaviour of specific components of the circulatory system. The pulsatile nature of pressure in large arteries is, however, irrelevant to perfusion of the peripheral tissues, since virtually all pulsatility is damped out by the time blood enters the capillaries. Also, calculation of parameters such as peripheral resistance requires an averaged value for pressure. The concept of mean arterial pressure is, therefore, essential to quantitative evaluation of circulatory function.
Does mean blood pressure change with heart rate?
or
With increasing heart rate, the shape of the BP wave changes so that the flatter late diastolic portion disappears and the waveform becomes more triangular. There is some experimental evidence suggesting that under these circumstances mean BP may be better approximated by DBP + 2/5PP (Robinson et al 1988).
Central and peripheral arterial pressures
The concept of arterial pressure generation from cardiac ejection and the factors determining systolic and diastolic limits as discussed above relate specifically to pressure just outside the semilunar valves. In the systemic circulation, however, additional factors become significant in pressure determination the further one moves away from the heart down the system of distributing arteries, with the result that absolute values recorded from, for example, arteries in the arm or leg, are no longer a precise reflection of the pressures in the aortic arch.
MEASUREMENT OF ARTERIAL PRESSURE
Auscultation
The technique relies on the luminal diameter of an artery being narrowed along the section underneath an inflated occlusive cuff and that this diameter suddenly increases at the downstream edge of the cuff. Flow velocity is increased through the narrowed section of the vessel. The combination of this increased velocity and the larger diameter vessel just downstream of the cuff transforms the flow profile to a turbulent one just in this region. At occlusive pressures above SBP there is of course no forward flow and so no turbulence. At pressures below SBP, however, intra-arterial pressure exceeds the cuff pressure for a portion of each cardiac cycle, producing periods of noisy turbulent flow separated by silence. These noises are known as Korotkow sounds.
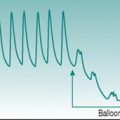
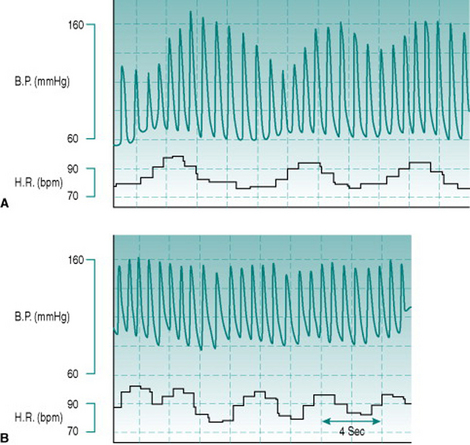
During inspiration, the increased cardiac filling and consequent increased stroke volume associated with negative intrathoracic pressure causes a rise in SBP. In younger individuals, this is reinforced by the tachycardic phase of sinus arrhythmia. Appreciable respiratory fluctuations in SBP are seen even during quiet respiration, and are more pronounced at low respiratory frequencies because the longer period of low intrathoracic pressure allows greater cardiac filling (Fig. 4.3). In order to measure SBP accurately, it is obviously important that the cuff is inflated to a pressure that is above the highest SBP value. The standard recommendation is for inflation to a value around 20 mmHg higher than that at which the palpated radial pulse disappears, but this advice does not take account of the respiratory phase at which the pulse is detected. For accurate results, it is a sensible precaution to measure several palpated SBP values over a complete respiratory cycle and then to use an inflation pressure for auscultation around 20 mmHg above the maximum recorded.
However, it is essential for the experimental scientist to remember that the association of Korotkow phase V with DBP is coincidental and based entirely on the absolute velocity of blood flow. If velocity increases because cardiac output is elevated (for example by exercise or pregnancy), or because the occluded artery is small in diameter (as occurs in children), then less compression of the artery will be sufficient to cause turbulence. Under these circumstances, Korotkow sounds may persist until cuff pressure is as much as 20–30 mmHg below DBP. By contrast, the cuff pressure at which muffling occurs has a constant and close relationship to DBP. For this reason, muffling and not disappearance of sounds must be used as the auscultatory criterion for DBP during exercise if serious errors are to be avoided. A stethoscope is essential in such circumstances: microphones are able to reliably recognize only the presence or absence of sounds.
Robinson et al (1988) proposed on the basis of comparisons of auscultatory and inter-arterial BP values that the standard formula DBP + 1/3PP does not provide accurate calculation of mean BP when auscultatory readings are used during heavy exercise; it was suggested that DBP + 1/2PP gave a closer approximation of true (that is, intra-arterial) mean pressure. However, the intra-arterial values in that study were significantly higher than those from auscultation and appeared likely to be an overestimate of the true pressure because of the cannula placement (see Intra-arterial catheters, below). If this probable error is discounted then there seems no good reason to assume that the standard formula is not accurate even at high work intensities.
In a few individuals the Korotkow sounds disappear and then reappear in the middle of the pulse pressure range. The silent range of pressures is known as the ‘auscultatory gap’ (Korotkow phases II–III). In these individuals, the pressure at which sounds reappear might be mistaken for SBP, or the pressure at which they disappear might be mistaken for DBP. It is, therefore, a sensible precaution to always check the cuff pressure at which the palpated radial pulse disappears and reappears, before starting auscultatory measurement.
Applanation tonometry
This technique employs high-frequency application of inwardly directed pressure over an artery, so as to continually exactly balance the intravascular pressure. The pressurizing and sensing devices are located together in a housing that is strapped on the skin, overlying either the radial artery at the wrist or a digital artery on a finger. As no process of cuff inflation or deflation is needed, a continuous beat-to-beat record of BP is obtained. This makes the technique an attractive one when SBP varies from moment to moment and for situations in which rapid changes in BP must be tracked. For example, a Valsalva manoeuvre (see Chapter 10, p. 120) lasts typically for only around 12 s. Over this time there are several significant changes in BP due to different mechanisms, all of which must be measured in order to assess the physiological response. None of these pressure changes could be detected by auscultation or oscillometry because the cuff inflation–deflation cycle takes in excess of 20 s.
Intra-arterial catheters
To interpret intra-arterial BP measurements accurately, it is important to know the position of the catheter tip and the direction in which this faces. The catheter is usually inserted retrogradely into the radial artery in the forearm or the femoral artery in the groin and, because of the rise in SBP with increasing distance away from the heart (see Central and peripheral pressures, p. 35), the absolute pressures recorded will depend on how far the cannula tip is advanced towards the central aorta. In addition, most catheters are open-tipped tubes, so when they are inserted retrogradely into an artery the open tip faces upstream. Under these circumstances, the pressure recorded is greater than the true intravascular hydrostatic pressure, because of the kinetic energy of blood flow pushing on the catheter lumen. The kinetic component is determined primarily by the velocity of blood flow and can be calculated as:
When an end-opening catheter faces downstream, then the true intra-arterial pressure is underestimated by the Pkinetic value. This is not a problem with systemic BP measurement but can be important when measuring pulmonary BP, since the catheters for this purpose are inserted through a central vein and passed on through the right heart (see Chapter 8, p. 101). The only way in which the kinetic artefact can be obviated is to use a catheter that has its opening at right angles to the direction of blood flow.
Discussion
This is a nice example of technology getting in the way of biological reality! Home blood-pressure-measuring devices that rely on auscultatory detection of Korotkow sounds have to include an in-built microphone because it would be too difficult to market them with a separate stethoscope. However, anything but the most sophisticated microphone cannot distinguish between different qualities of sound and recognizes only whether the sound is present or absent. By definition, therefore, these devices are constrained to using Korotkow phase V as the index of DBP.
MEASUREMENT OF TOTAL PERIPHERAL RESISTANCE
so the advantages and limitations of techniques for determining each of these parameters have to be considered for any particular experimental situation. The unit for TPR as derived from this formula can be either (mmHg/mL)/min or (mmHg/L)/min, depending on whether cardiac output is expressed in L/min or mL/min and, rather confusingly, both are usually referred to simply as peripheral resistance units (PRUs) rather than citing the individual parameters involved. To avoid confusion, it is important to bear this in mind and be aware that PRUs derived using mL/min will give TPR values of the order of 0.02–0.05 while those derived using L/min give values around 20–50.
Robinson TR, Sue DY, Huszczuk A, Weiler-Ravell D, Hansen JE. Intra-arterial and cuff blood pressure responses during incremental cycle ergometry. Medicine and Science in Sports and Exercise. 1988;20:142-149.
Wasserman K, Hansen JE, Sue DY, Casaburi R, Whipp BJ. Principles of exercise testing and interpretation. Philadelphia: Lippincott Williams & Wilkins, 1999;125-126.

 . Some time ago, Rita had decided to monitor her blood pressure daily. She chose a home blood-pressure kit that detected Korotkow sounds with an in-built microphone rather than an oscillometric device, because she wanted to be able to use it during exercise. During her most recent bout of dizziness she recorded her blood pressure as 136/16 mHg. At rest, prior to the exercise, she had recorded values of 126/70 mmHg. Rita was understandably concerned that she could be suffering from inadequate circulation and that her baby may be in danger if she continued to exercise.
. Some time ago, Rita had decided to monitor her blood pressure daily. She chose a home blood-pressure kit that detected Korotkow sounds with an in-built microphone rather than an oscillometric device, because she wanted to be able to use it during exercise. During her most recent bout of dizziness she recorded her blood pressure as 136/16 mHg. At rest, prior to the exercise, she had recorded values of 126/70 mmHg. Rita was understandably concerned that she could be suffering from inadequate circulation and that her baby may be in danger if she continued to exercise.