Blood groups and blood testing
The blood groups
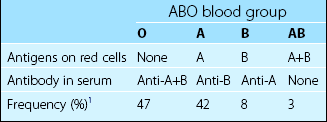
The most important blood group is the ABO system. The genes encoding the ABO antigens are located on chromosome 9 and are inherited in an autosomal dominant fashion. Each antigen is a sugar residue made by a specific glycosyl transferase. The ABO system is crucial in clinical blood transfusion as there are naturally occurring IgM antibodies in the serum targeted against the non-present ABO antigens (Table 41.1). These antibodies necessitate the use of ABO ‘compatible’ blood for transfusion. For example, the administration of incompatible group A blood to a group B patient would engender a potentially fatal haemolytic transfusion reaction due to the destruction of the donor’s group A red cells by the recipient’s anti-A antibody.
The testing of blood
The objective of routine testing of donated blood is to provide blood which can be selected for likely compatibility with a patient and which contains no identifiable infectious agent (Table 41.2). Antibody testing (e.g. for HIV and hepatitis C) is now supplemented by molecular techniques sensitive enough to trace the virus in the blood before the development of antibodies (i.e. during the ‘window period’).
Testing before transfusion
Blood grouping
The recipient’s red cells are tested for ABO and Rhesus antigens and the serum tested for naturally occurring antibodies to confirm the ABO group. Blood grouping tests traditionally rely on the visual identification of agglutination of red cells induced by the presence of antibodies against antigens present on the cell surface (Fig 41.1). Gel technology (see Fig 41.2) is widely used and increasingly automated. DNA-based tests may be employed as an adjunct to haemagglutination but they are not currently indicated for routine ABO and Rh group testing.
Antibody screening
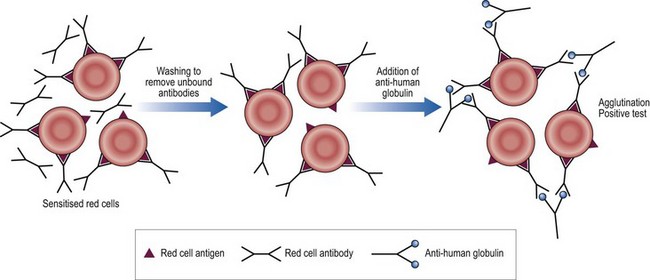
The patient’s serum is tested against three standard sets of screening red cells of known antigenic type. This is to detect immune or ‘atypical’ antibodies (i.e. non-ABO) which might destroy donor red cells. Clinically relevant antibodies are generally reactive at 37°C. A sensitive indirect antiglobulin test technique is used (see Fig 41.3). If an antibody is detected by this screen then a larger panel of red cells is tested to indentify it. The blood selected for the patient must be negative for the relevant antigen.
Practicalities of blood ordering
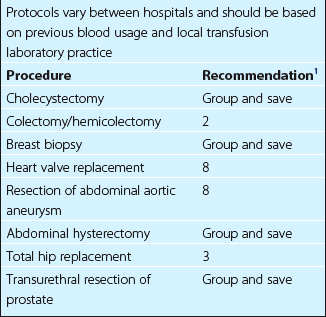
The bulk of blood is crossmatched for use in elective surgical procedures. Where there is only a small chance (less than 10%) that transfusion will be required it is reasonable to limit wastage by adopting a ‘group and save’ policy. The patient’s blood group is determined and the serum screened for atypical antibodies. Provided the screen is negative, blood is not routinely crossmatched. Most hospitals have implemented a formal surgical blood order schedule with guidelines for common operations (Table 43.3). Such guidelines are generalisations and special provision is made for unusually difficult procedures or patients who are judged to be at a higher than average risk of haemorrhage. Electronic crossmatching is very rapid and its introduction potentially reduces the number of operations for which blood is issued in advance.