Blood, Blood-Forming Organs, and the Immune Mechanism
ICD-10-CM Examples from Tabular
D72.82 Elevated white blood cell count
Excludes1 eosinophilia (D72.1)
D72.820. Lymphocytosis (symptomatic)
D72.821. Monocytosis (symptomatic)
Excludes1 infectious mononucleosis (B27.-)
Excludes1 confirmed infection—code to infection leukemia (C91.-, C92.-, C93.-, C94.-, C95.-)
D72.828. Other elevated white blood cell count
Functions of the Blood and Immune Systems
The blood is responsible for the following:
• Transportation of gases (oxygen [O2] and carbon dioxide [CO2]), chemical substances (hormones, nutrients, salts), and cells that defend the body.
• Regulation of the body’s fluid and electrolyte balance, acid-base balance, and body temperature.
• Protection of the body from infection.
• Protection of the body from loss of blood by the action of clotting.
The lymph system is responsible for the following:
• Cleansing the cellular environment.
• Returning proteins and tissue fluids to the blood (drainage).
• Providing a pathway for the absorption of fats and fat-soluble vitamins into the bloodstream.
• Defending the body against disease.
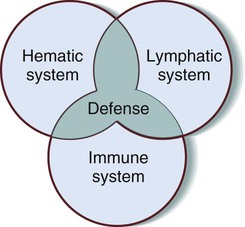
• The lymphatic system is discussed in Chapter 9 as part of the circulatory system. Explaining its role in protecting the body against disease, however, requires a discussion of how it interacts with the hematic and immune systems.
The immune system is responsible for the following:
Figure 8-1 is a Venn diagram of the interrelationship among the three systems, with the shared goals of homeostasis and protection at the intersection of the three circles.
Anatomy and Physiology
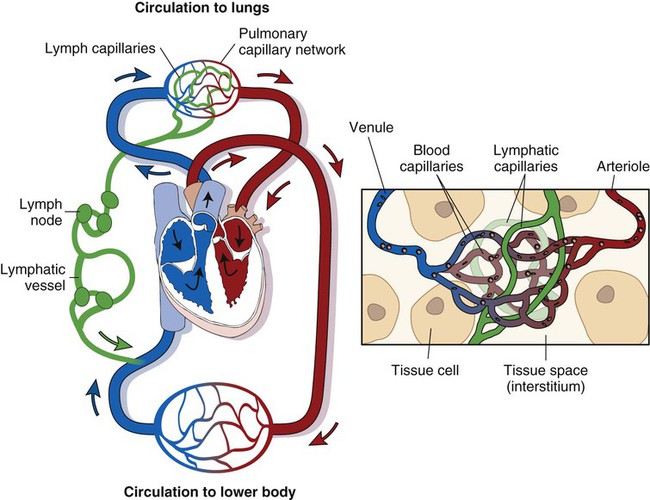
Figure 8-2 shows the relationship of the lymphatic vessels to the circulatory system. Note the close relationship between the distribution of the lymphatic vessels and the venous blood vessels. Tissue fluid is drained by the lymphatic capillaries and is transported by a series of larger lymphatic vessels toward the heart.
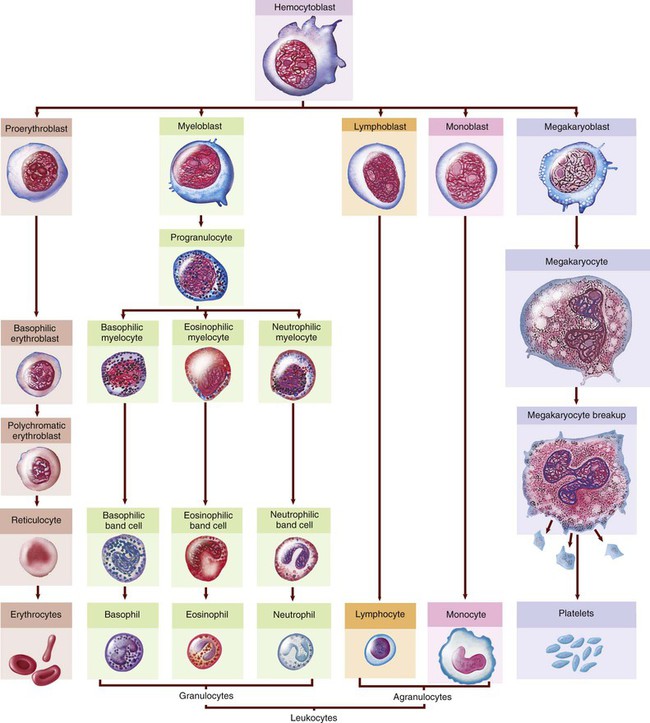
Hematic System
The hematic system is composed of blood and the vessels that carry the blood throughout the body. The formation of blood, hematopoiesis, begins in the bone marrow with a single type of cell, a multipotential (pluripotent) hematopoietic stem cell (HSC), or hemocytoblast. This cell divides into cells that mature in lymphatic tissue (band T lymphocytes) and cells that mature in the bone marrow. Refer to Figure 8-3 to follow the development from the stem cell to specialized mature blood cells.
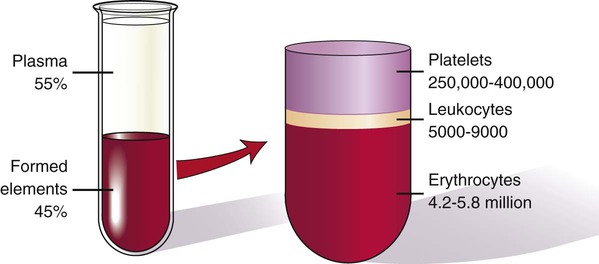
Whole blood is composed of a solid portion that consists of formed elements, or cells, and a liquid portion called plasma. Blood cells make up 45% of the total blood volume, and plasma makes up the other 55% (Fig. 8-4).
< ?xml:namespace prefix = "mml" />
The solid portion of blood is composed of three different types of cells:
1. Erythrocytes, also called red blood cells (RBCs).
2. Leukocytes, also called white blood cells (WBCs).
3. Thrombocytes, also called clotting cells, cell fragments, or platelets.
Components of Blood
Erythrocytes (Red Blood Cells)
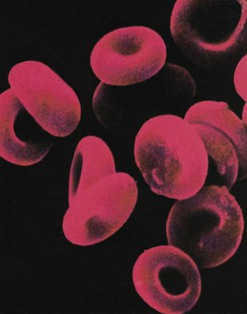
The erythrocytes (which are normally present in the millions) have the important function of transporting O2 and CO2 throughout the body (Fig. 8-5). The vehicle for this transportation is a protein-iron pigment called hemoglobin. When combined with oxygen, it is termed oxyhemoglobin.
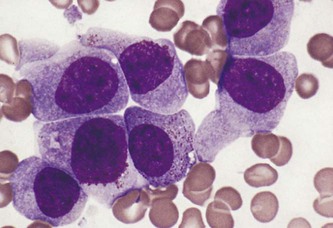
Leukocytes (White Blood Cells)
Granulocytes (Polymorphonucleocytes)
1. Eosinophils (eosins) are cells that absorb an acidic dye, which causes them to appear reddish. An increase in eosinophils is a response to a need for their function in defending the body against allergens and parasites.
2. Neutrophils (neuts), the most numerous WBCs, are cells that do not absorb either an acidic or a basic dye and consequently are a purplish color. They are also called phagocytes because they specialize in phagocytosis and generally combat bacteria in pyogenic infections. This means that these cells are drawn to the site of a pathogenic “invasion,” where they consume the enemy and remove the debris resulting from the battle. Because the nucleus in immature neutrophils has a long “bandlike” shape, these cells are often referred to as band cells. They are also called stabs; the name is from the German word for rods because of their rodlike appearance. As the cells continue to mature, the bands divide, and the adult cells are renamed segs because now the nuclei are divided into clumps (segmented).
3. Basophils (basos) are cells that absorb a basic (or alkaline) dye and stain a bluish color. Especially effective in combating parasites, they release histamine (a substance that initiates an inflammatory response) and heparin (an anticoagulant), both of which are instrumental in healing damaged tissue.
Agranulocytes (Mononuclear Leukocytes)
1. Monocytes: These cells, named for their single, large nucleus, transform into macrophages, which eat pathogens (phagocytosis) and are effective against severe infections.
2. Lymphocytes (lymphs): These cells are key in what is called the immune response, which involves the “recognition” of dangerous, foreign (viral) substances and the manufacture of their neutralizers. The foreign substances are called antigens, and the neutralizers are called antibodies.
Thrombocytes (Platelets)
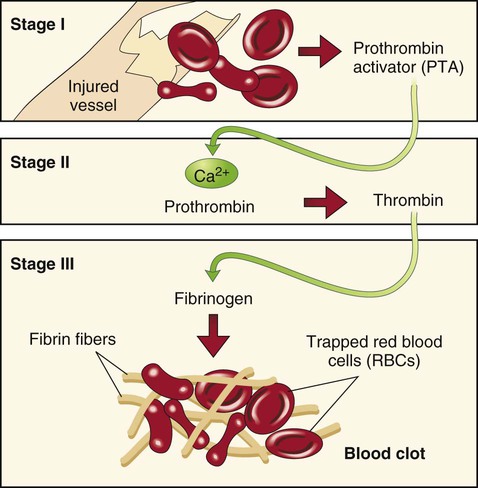
Platelets (also known as thrombocytes or plats) have a round or oval shape and are so named because they look like small plates. Platelets aid in coagulation, the process of changing a liquid to a solid. When blood cells escape their normal vessels, they agglutinate, or clump together, by the following process: First, they release factor X (formerly called thrombokinase), which, in the presence of calcium, reacts with the blood protein prothrombin to form thrombin. Thrombin then converts another blood protein, fibrinogen, to fibrin, which eventually forms a meshlike fibrin clot (blood clot), achieving hemostasis (control of blood flow; that is, stopping the bleeding). See Figure 8-6 for a visual explanation of the clotting process.
Plasma
Plasma, the liquid portion of blood, is composed of the following:
2. Inorganic substances (calcium, potassium, sodium)
3. Organic substances (glucose, amino acids, fats, cholesterol, hormones)
4. Waste products (urea, uric acid, ammonia, creatinine)
5. Plasma proteins (serum albumin, serum globulin, and two clotting proteins: fibrinogen and prothrombin)
Serum (pl. sera) is plasma minus the clotting proteins. Serology is the branch of laboratory medicine that studies blood serum for evidence of infection by evaluating antigen-antibody reactions in vitro.
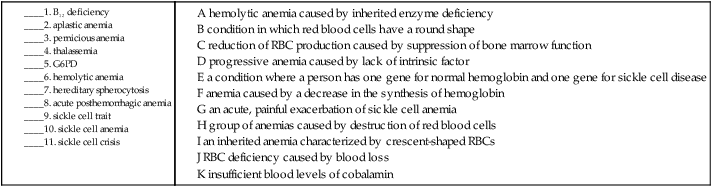
B. Match the following suffixes with their meanings.
11. polynuclear _____________________________________________________________________________________
12. agranulocytic ___________________________________________________________________________________
13. lymphatic ______________________________________________________________________________________
14. anuclear ________________________________________________________________________________________
15. polymorphic ____________________________________________________________________________________
Blood Groups
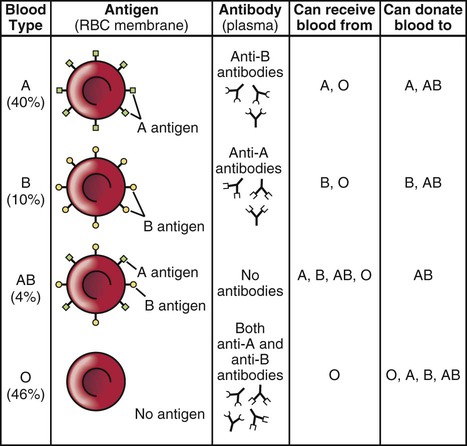
Human blood is divided into four major different types: A, B, AB, and O. See Figure 8-7 for a table of blood types, agglutinogens, and agglutinins. The differences are due to antigens present on the surface of the red blood cells. Antigens are substances that produce an immune reaction by their nature of being perceived as foreign to the body. In response, the body produces substances called antibodies that nullify or neutralize the antigens. In blood, these antigens are called agglutinogens because their presence can cause the blood to clump. The antibody is termed an agglutinin. For example, type A blood has A antigen, type B has B antigen, type AB has both A and B antigens, and type O has neither A nor B antigens. If an individual with type A blood is transfused with type B blood, the A antigens will form anti-B antibodies because they perceive B blood as being foreign. Following the logic of each of these antigen-antibody reactions, an individual with type AB blood is a universal recipient, and an individual with type O blood is a universal donor.
Another antigen, the Rh factor, is important in pregnancy because a mismatch between the fetus and the mother can cause erythroblastosis fetalis, or hemolytic disease of the newborn (HDN) (see Fig. 7-10). In this disorder, a mother with a negative Rh factor will develop antibodies to an Rh+ fetus during the first pregnancy. If another pregnancy occurs with an Rh+ fetus, the antibodies will destroy the fetal blood cells.
Immune System
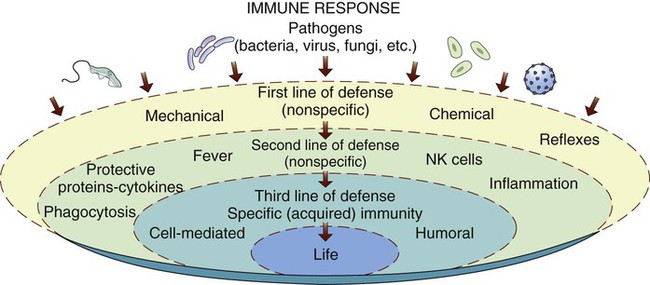
Figure 8-8 illustrates the levels of defense. The two outside circles represent nonspecific immunity and its two levels of defense. The inner circle represents the various mechanisms of specific immunity, which can be natural (genetic) or acquired in four different ways. Most pathogens can be contained by the first two lines of nonspecific defense. However, some pathogens deserve a “special” means of protection, which is discussed in the section titled “Specific Immunity.”
Nonspecific Immunity
• Mechanical: Examples include the skin, which acts as a barrier, and the sticky mucus on mucous membranes, which serves to trap pathogens.
• Physical: Examples include coughing, sneezing, vomiting, and diarrhea. Although not pleasant, these serve to expel pathogens that have gotten past the initial barriers.
• Chemical: Examples include tears, saliva, and perspiration. These have a slightly acidic nature that deters pathogens from entering the body while also washing them away. In addition, stomach acids and enzymes kill germs.
Defensive processes include the following:
• Phagocytosis: Phagocytosis is the process of cells “eating” and destroying microorganisms. Pathogens that make it past the first line of defense and enter into the bloodstream may be consumed by neutrophils and monocytes.
• Inflammation: Acquiring its name from its properties, inflammation is a protective response to irritation or injury. The characteristics (heat, swelling, redness, and pain) arise in response to an immediate vasoconstriction, followed by an increase in vascular permeability. These provide a good environment for healing. If caused by a pathogen, the inflammation is called an infection.
• Pyrexia: Pyrexia is the medical term for fever. When infection is present, fever may serve a protective function by increasing the action of phagocytes and decreasing the viability of certain pathogens.
Specific Immunity
Types of Acquired Immunity
Active acquired immunity can take either of the following two forms:
1. Natural: Development of memory cells to protect the individual from a second exposure.
2. Artificial: Vaccination (immunization) that uses a greatly weakened form of the antigen, thus enabling the body to develop antibodies in response to this intentional exposure. Examples are the DTP and MMR vaccines.
Passive acquired immunity can take either of the following two forms:
1. Natural: Passage of antibodies through the placenta or breast milk.
2. Artificial: Use of immunoglobulins harvested from a donor who developed resistance against specific antigens.
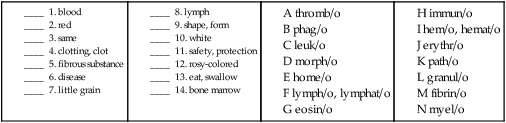
Combining Forms for the Anatomy and Physiology of Blood and the Immune System
| Meaning | Combining Form |
| appendix | append/o, appendic/o |
| base | bas/o |
| blood | hem/o, hemat/o |
| bone marrow | myel/o |
| cell | cyt/o |
| clotting, clot | thromb/o |
| clumping | agglutin/o |
| disease | path/o |
| eat, swallow | phag/o |
| fever, fire | pyr/o |
| fiber | fibr/o |
| fibrous substance | fibrin/o |
| liquid | humor/o |
| little grain | granul/o |
| lymph | lymph/o, lymphat/o |
| nucleus | nucle/o |
| oxygen | ox/i, ox/o |
| plasma | plasm/a, plasm/o |
| red | erythr/o |
| rosy-colored | eosin/o |
| safety, protection | immun/o |
| same | home/o |
| serum | ser/o |
| shape | morph/o |
| spleen | splen/o |
| thymus | thym/o |
| tonsil | tonsill/o |
| white | leuk/o |
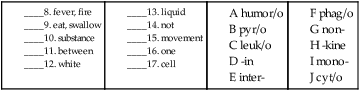
Prefixes for the Anatomy and Physiology of the Blood and Immune Systems
| Prefix | Meaning |
| a- | without |
| anti- | against |
| inter- | between |
| mono- | one |
| oxy- | oxygen |
| poly- | many |
| pro- | before |
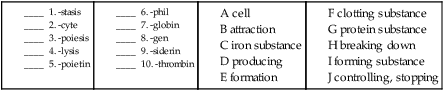
Suffixes for the Anatomy and Physiology of the Blood and Immune Systems
| Suffix | Meaning |
| -cyte | cell |
| -exia | condition |
| -gen | producing |
| -globin | protein substance |
| -in | substance |
| -kine | movement |
| -leukin | white substance |
| -lysis | breaking down |
| -osis | abnormal condition |
| -phil | attraction |
| -poiesis | formation |
| -poietin | forming substance |
| -siderin | iron substance |
| -stasis | controlling, stopping |
| -thrombin | clotting substance |
Pathology
Terms Related to Nutritional Anemias (D5Ø-D53)
| Term | Word Origin | Definition |
| B12 deficiency anemia | Insufficient blood levels of cobalamin, also called vitamin B12, which is essential for red blood cell maturation. Condition may be caused by inadequate dietary intake, as in some extreme vegetarian diets, or it may result from absence of intrinsic factor, a substance in the GI system essential to vitamin B12 absorption. | |
| folate deficiency anemia | Anemia as a result of a lack of folate from dietary, drug-induced, congenital, or other causes. | |
| pernicious anemia | an- no, not, without -emia blood condition |
Progressive anemia that results from a lack of intrinsic factor essential for the absorption of vitamin B12. |
| sideropenia | sider/o iron -penia condition of deficiency |
Condition of having reduced numbers of RBCs because of chronic blood loss, inadequate iron intake, or unspecified causes. A type of iron deficiency anemia. |
Terms Related to Hemolytic Anemias (D55-D59)
| Term | Word Origin | Definition |
| autoimmune acquired hemolytic anemia | auto- self immune safety, protection hem/o blood -lytic pertaining to destruction an- no, not -emia blood condition |
Anemia caused by the body’s destruction of its own RBCs by serum antibodies. |
| glucose-6-phosphate-dehydrogenase (G6PD) | An inherited enzyme deficiency that causes hemolytic anemia. | |
| hemoglobinopathy | hem/o blood globin/o protein -pathy disease process |
A general term for genetic defects of hemoglobin. |
| hemolytic anemia | hem/o blood -lytic pertaining to destruction |
A group of anemias caused by destruction of red blood cells. |
| hereditary spherocytosis | spher/o sphere, globe -cytosis condition of abnormal increase in cells |
Condition in which red blood cells have a round shape (instead of biconcave disc-shape) because of a fragile membrane. |
| nonautoimmune acquired hemolytic anemia | non- not hem/o blood -lytic pertaining to destruction an- no, not -emia blood condition |
Anemia that may be drug induced or may be caused by an infectious disease, in which the RBCs are destroyed. |
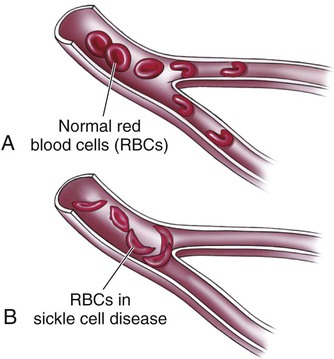
| sickle-cell disorders | Sickle cell trait is a condition where an individual has one gene that is for normal hemoglobin and one for sickle hemoglobin. Those who have the trait do not exhibit symptoms of sickle cell disease. Sickle cell anemia is an inherited anemia characterized by crescent-shaped RBCs. This abnormality in morphology causes RBCs to block small-diameter capillaries, thereby decreasing the oxygen supply to the cells (Fig. 8-9). A sickle cell crisis is an acute, painful exacerbation of sickle cell anemia. |
|
| thalassemia | thalass/o sea -emia blood condition |
Group of inherited disorders of people of Mediterranean, African, and Southeast Asian descent, in which the anemia is the result of a decrease in the synthesis of hemoglobin, resulting in decreased production and increased destruction of RBCs. |
Terms Related to Aplastic and Other Anemias and Other Bone Marrow Failure Syndromes (D6Ø-D64)
| Term | Word Origin | Definition |
| acute posthemorrhagic anemia | post- after hem/o blood -rrhagic pertaining to bursting forth an- no, not -emia blood condition |
RBC deficiency caused by blood loss. |
| aplastic anemia | a- no, not, without plast/o formation -ic pertaining to an- no, not, without -emia blood condition |
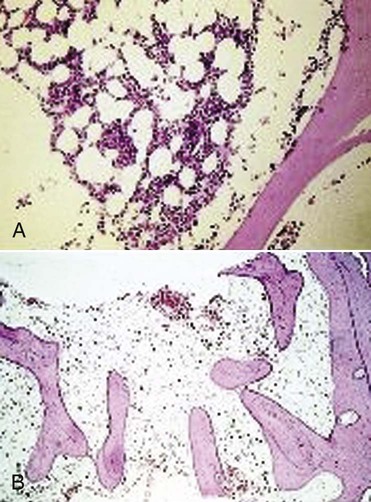
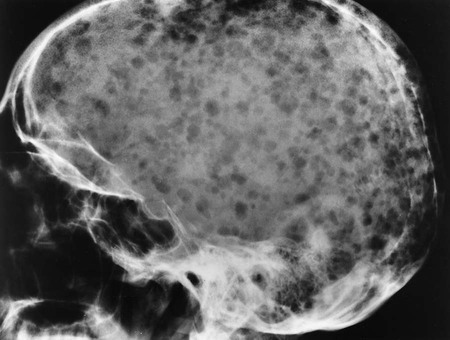
Suppression of bone marrow function leading to a reduction in RBC production. Although causes of this often fatal type of anemia may be hepatitis, radiation, or cytotoxic agents, most causes are idiopathic. Also called hypoplastic anemia (Fig. 8-10). |
| erythroblastopenia | erythr/o red blast/o embryonic, immature -penia condition of deficiency |
Deficiency of immature red blood cells. Significant in that they indicate a future lack of mature blood cells. |
| myelophthisis | myel/o bone marrow -phthisis wasting |
Wasting of bone marrow, usually with replacement by cancer cells. |
| pancytopenia | pan- all cyt/o cell -penia condition of deficiency |
Deficiency of all blood cells caused by dysfunctional stem cells (Fig. 8-11). |
12. condition of iron deficiency _____________________________________________________________________
13. disease process of blood protein __________________________________________________________________
14. condition of red embryonic, immature deficiency _________________________________________________
15. wasting of bone marrow _________________________________________________________________________
16. condition of all cell deficiency ___________________________________________________________________
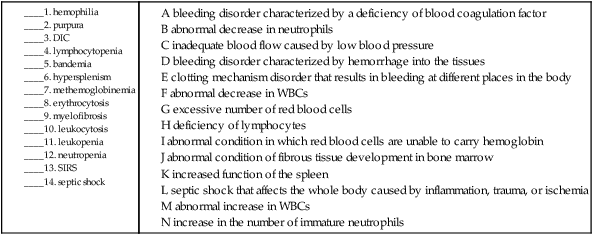
Terms Related to Coagulation Defects, Purpura, and Other Hemorrhagic Conditions (D65-D69)
| Term | Word Origin | Definition |
| disseminated intravascular coagulopathy (DIC) | intra- within vascul/o vessel -ar pertaining to coagul/o clotting -pathy disease process |
A disorder of clotting mechanisms that results in bleeding at scattered sites in the body. |
| hemophilia | hem/o blood -philia condition of attraction |
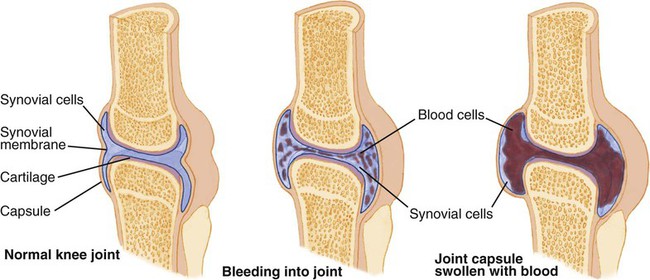
Group of inherited bleeding disorders characterized by a deficiency of one of the factors (factor VIII) necessary for the coagulation of blood (Fig. 8-12). |
| purpura | purpur/o purple -a noun ending |
Bleeding disorder characterized by hemorrhage into the tissues (Fig. 8-13). |
| thrombocytopenia | thromb/o clot, clotting cyt/o cell -penia condition of deficiency |
Deficiency of platelets that causes an inability of the blood to clot. The most common cause of bleeding disorders. |
| thrombophilia | thromb/o clot –philia condition of attraction |
An increase in the body’s tendency to form clots. |
Terms Related to Other Disorders of Blood and Blood-Forming Organs (D7Ø-D77)
| Term | Word Origin | Meaning |
| asplenia | a- without splen/o spleen -ia condition |
Absence of the spleen, either congenital or acquired due to surgical removal. |
| bandemia | band/o bands -emia blood condition |
An increase in the number of immature neutrophils (band cells) in the blood. Increases of band cells may indicate infection. |
| basophilia | bas/o base -philia condition of attraction |
Excessive basophils in the blood. |
| eosinophilia | eosin/o rosy-colored -philia condition of attraction |
An increase in the number of eosinophils in the blood. |
| erythrocytosis | erythr/o red -cytosis condition of abnormal increase of cells |
An excessive number of red blood cells in the blood. |
| hypersplenism | hyper- excessive splen/o spleen -ism condition |
Increased function of the spleen, resulting in hemolysis (Fig. 8-14). |
| leukocytosis | leuk/o white -cytosis condition of abnormal increase in cells |
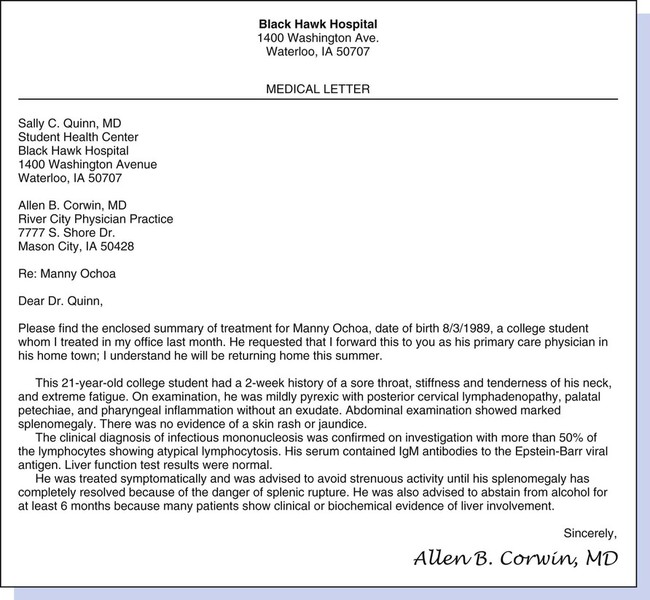
Abnormal increase in WBCs. Abnormal increases in each type of granulocyte are termed eosinophilia, basophilia, and neutrophilia, where the suffix -philia denotes a slight increase. Abnormal increases in the number of each type of agranulocyte are termed lymphocytosis and monocytosis. |
| leukopenia | leuk/o white -penia condition of deficiency |
Abnormal decrease in WBCs. Specific deficiencies are termed neutropenia, eosinopenia, monocytopenia, and lymphocytopenia. Also called leukocytopenia. |
| lymphocytopenia | lymph/o lymph cyt/o cell -penia condition of deficiency |
Deficiency of lymphocytes caused by infectious mononucleosis, malignancy, nutritional deficiency, or a hematological disorder. |
| methemoglobinemia | met(a)- change hem/o blood globin/o protein -emia blood condition |
Abnormal condition in which red blood cells are unable to carry hemoglobin. May be hereditary or acquired. |
| monocytosis | mono- one –cytosis abnormal increase of cells |
Excessive monocytes in the blood. |
| myelofibrosis | myel/o bone marrow fibr/o fiber -osis abnormal condition |
Abnormal condition of fibrous tissue development in the bone marrow due to a chromosomal abnormality (Fig. 8-15). |
| neutropenia | neutr/o neutral -penia condition of deficiency |
Abnormal decrease in neutrophils due to disease process. Formerly called agranulocytosis. |
| plasmacytosis | plasm/a plasma -cytosis abnormal increase of cells |
Excessive plasma cells in the blood. |
| splenitis | splen/o spleen -itis inflammation |
Inflammation of the spleen. |
Terms Related to Systemic Infections of the Blood
| Term | Word Origin | Definition |
| septicemia | septic/o infection -emia blood condition |
Systemic infection with pathological microbes in the blood as the result of an infection that is spread from elsewhere in the body. The term sepsis means infection. |
| septic shock | sept/o infection -ic pertaining to |
Inadequate blood flow to the body caused by an overwhelming infection and resultant low blood pressure. Organs fail and death may occur. |
| systemic inflammatory response syndrome (SIRS) | Type of septic shock, SIRS is an inflammatory state affecting the whole body. SIRS can be caused by trauma, ischemia, or inflammation. |
15. thrombocytopenia ______________________________________________________________________________
16. eosinophilia ____________________________________________________________________________________
17. plasmacytosis ___________________________________________________________________________________
18. asplenia ________________________________________________________________________________________
19. septicemia ______________________________________________________________________________________
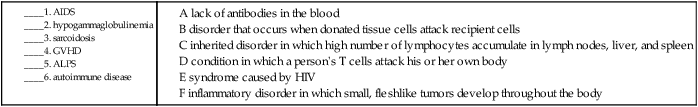
Terms Related to Certain Disorders Involving the Immune Mechanism (D8Ø-D89)
| Term | Word Origin | Definition |
| autoimmune lymphoproliferative syndrome (ALPS) | auto- self immun/o safety, protection syn- together –drome run |
Inherited disorder of the immune system with unusually high numbers of lymphocytes that accumulate in the lymph nodes, liver, and spleen. |
| graft-versus-host disease (GVHD) | Disorder occurring when donated tissue cells attack the cells of the recipient. | |
| hypogammaglobulinemia | hypo- deficiency gamma globulin/o protein -emia blood condition |
A lack of antibodies (immunoglobulin G) in the blood. |
| sarcoidosis | sarc/o flesh -oid like -osis abnormal condition |
An inflammatory disorder in which small, fleshlike tumors develop throughout the body. |
Terms Related to Other Immune Disorders
| Term | Word Origin | Definition |
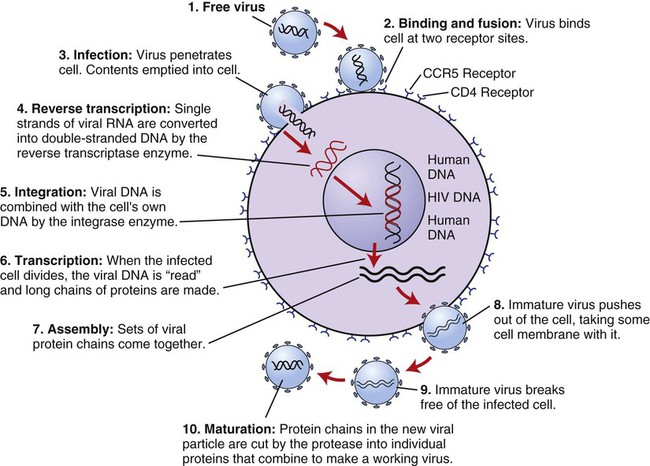
| acquired immunodeficiency syndrome (AIDS) | immun/o safety, protection | Syndrome caused by the human immunodeficiency virus (HIV) and transmitted through body fluids. Figure 8-16 demonstrates the life cycle of HIV. |
| autoimmune disease | auto- self immun/o safety, protection |
Condition in which a person’s T cells attack his/her own cells, causing extensive tissue damage and organ dysfunction. Examples of resultant autoimmune diseases include myasthenia gravis, rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis. |
Terms Related to Benign Neoplasms
| Term | Word Origin | Definition |
| myelodysplastic syndrome | myel/o bone marrow dys- abnormal -plastic pertaining to forming |
Group of disorders that result from a defect in the bone marrow. Also referred to as preleukemia. |
| polycythemia vera | poly- many, much cyt/o cell -(h)emia blood condition vera true |
Condition in which the bone marrow produces an excessive number of blood cells. |
| thymoma | thym/o thymus gland -oma tumor, mass |
Noncancerous tumor of epithelial origin that is often associated with myasthenia gravis. |
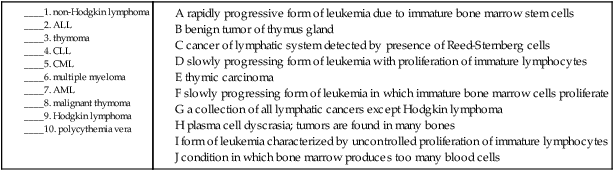
Terms Related to Malignant Neoplasms
| Term | Word Origin | Definition |
| acute lymphocytic leukemia (ALL) | lymph/o lymph cyt/o cell -ic pertaining to leuk/o white -emia blood condition |
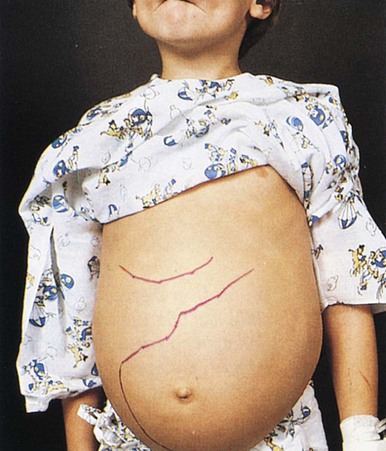
Also termed acute lymphoblastic leukemia, this cancer is characterized by the uncontrolled proliferation of immature lymphocytes. It is the most common type of leukemia for individuals under the age of 19 (Fig. 8-17). |
| acute myelogenous leukemia (AML) | myel/o bone marrow -genous pertaining to originating from leuk/o white -emia blood condition |
This rapidly progressive form of leukemia develops from immature bone marrow stem cells. |
| chronic lymphocytic leukemia (CLL) | lymph/o lymph cyt/o cell -ic pertaining to leuk/o white -emia blood condition |
A slowly progressing form of leukemia in which immature lymphocytes proliferate. Occurs most frequently in middle age (or older) adults, rarely in children. |
| chronic myelogenous leukemia (CML) | myel/o bone marrow -genous pertaining to originating from leuk/o white -emia blood condition |
A slowly progressing form of leukemia in which immature bone marrow cells proliferate. Like CLL, it occurs most frequently in middle age (or older) adults, rarely in children. |
| Hodgkin lymphoma | lymph/o lymph -oma tumor, mass |
Also termed Hodgkin disease, this cancer is diagnosed by the detection of a type of cell specific only to this disorder: Reed-Sternberg cells. |
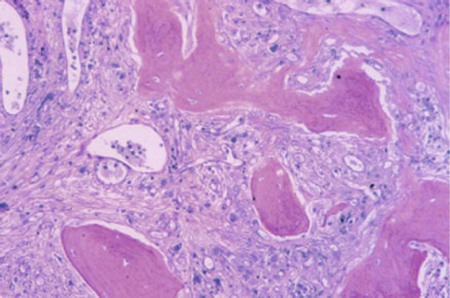
| myeloma, multiple | myel/o bone marrow -oma tumor, mass |
Also termed plasma cell dyscrasia or myelomatosis, this rare malignancy of the plasma cells is formed from B lymphocytes. It is called “multiple” myeloma because the tumors are found in many bones. If it occurs in only one bone, the tumor is referred to as a plasmacytoma (Fig. 8-18). |
| non-Hodgkin lymphoma | lymph/o lymph -oma tumor, mass |
A collection of all other lymphatic cancers but Hodgkin lymphomas. This type is the more numerous of the two lymphomas and is the sixth most common type of cancer in the United States. |
| thymoma, malignant | thym/o thymus gland -oma tumor, mass |
Also termed thymic carcinoma, this rare malignancy of the thymus gland is particularly invasive and, unlike its benign form, is not associated with autoimmune disorders. |
Procedures
Terms Related to Laboratory Tests
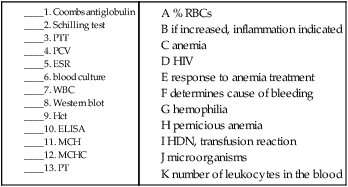
| Term | Word Origin | Definition |
| AIDS tests—ELISA, Western blot | Tests to detect the presence of HIV types 1 and 2 (Fig. 8-19). | |
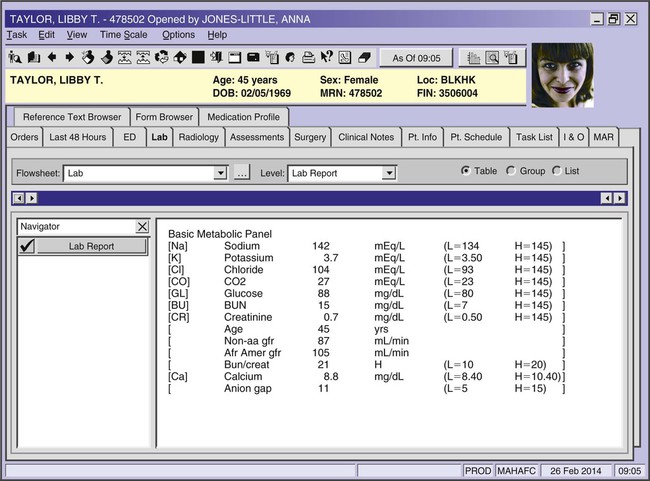
| basic metabolic panel (BMP) | Group of blood tests to measure calcium; glucose; electrolytes such as sodium (Na), potassium (K), and chloride (Cl); creatinine; and blood urea nitrogen (BUN). | |
| blood cultures | Blood samples are submitted to propagate microorganisms that may be present. Cultures may be indicated for bacteremia or septicemia, or to discover other pathogens (fungi, viruses, or parasites) (Fig. 8-20). | |
| complete blood cell count (CBC) | Twelve tests, including RBC (red blood cell count), WBC (white blood cell count), Hb (hemoglobin), Hct/PCV (hematocrit/packed-cell volume), and diff (WBC differential). | |
| comprehensive metabolic panel (CMP) | Set of 14 blood tests that add protein and liver function tests to the BMP. Glucose is also measured with a different method than in the basic panel. | |
| Coombs antiglobulin test | anti- against -globulin protein substance |
Blood test to diagnose hemolytic disease of the newborn (HDN), acquired hemolytic anemia, or a transfusion reaction. |
| diff count | Measure of the numbers of the different types of WBCs. | |
| erythrocyte sedimentation rate (ESR) | erythr/o red -cyte cell |
Measurement of time for mature RBCs to settle out of a blood sample after an anticoagulant is added. An increased ESR indicates inflammation. |
| hematocrit (Hct), packed-cell volume (PCV) | hemat/o blood -crit separate |
Measure of the percentage of RBCs in the blood. |
| hemoglobin (Hgb, Hb) | hem/o blood -globin protein substance |
Measurement of the iron-containing pigment of RBCs that carries oxygen to tissues. |
| mean corpuscular hemoglobin (MCH) | hem/o blood -globin protein substance |
Test to measure the average weight of hemoglobin per RBC. Useful in diagnosing anemia. |
| mean corpuscular hemoglobin concentration (MCHC) | Test to measure the concentration of hemoglobin in RBCs. This test is useful for measuring a patient’s response to treatment for anemia. | |
| partial thromboplastin time (PTT) | thromb/o clot, clotting -plastin forming substance |
Test of blood plasma to detect coagulation defects of the intrinsic system; used to detect hemophilia. |
| prothrombin time (PT) | pro- before -thrombin clotting substance |
Test that measures the amount of time taken for clot formation. It is used to determine the cause of unexplained bleeding, to assess levels of anticoagulation in patients taking warfarin or with vitamin K deficiency, and to assess the ability of the liver to synthesize blood-clotting proteins. |
| Schilling test | Nuclear medicine test used to diagnose pernicious anemia and other metabolic disorders. | |
| white blood cell count (WBC) | Measurement of the number of leukocytes in the blood. An increase may indicate the presence of an infection; a decrease may be caused by radiation or chemotherapy. |
Terms Related to Blood and Bone Marrow Procedures
| Term | Word Origin | Definition |
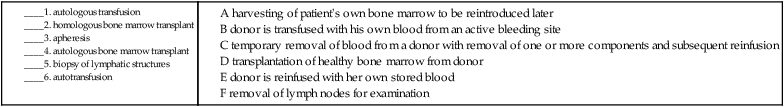
| apheresis | -apheresis removal | Temporary removal of blood from a donor, in which one or more components are removed, and the rest of the blood is reinfused into the donor. Examples include leukapheresis, removal of WBCs; plasmapheresis, removal of plasma; and plateletpheresis, removal of thrombocytes. Also called pheresis. |
| autologous bone marrow transplant | auto- self log/o study -ous pertaining to |
Harvesting of patient’s own healthy bone marrow before treatment for reintroduction later. |
| autologous transfusion | auto- self log/o study -ous pertaining to trans- across -fusion pouring |
Process in which the donor’s own blood is removed and stored in anticipation of a future need. |
| autotransfusion | auto- self trans- across -fusion pouring |
Process in which the donor is transfused with his/her own blood, after anticoagulation and filtration, from an active bleeding site in cases of major surgery or trauma. |
| blood transfusion | trans- across -fusion pouring |
Intravenous transfer of blood from a donor to a recipient, giving either whole blood or its components (Fig. 8-21). |
| bone marrow transplant (BMT) | The transplantation of bone marrow to stimulate production of normal blood cells. | |
| hemostasis | hem/o blood –stasis stopping, controlling |
The control of bleeding by mechanical or chemical means. |
| homologous bone marrow transplant | homo- same (species) log/o study -ous pertaining to |
Transplantation of healthy bone marrow from a donor to a recipient to stimulate formation of new blood cells. |
Terms Related to Lymphatic and Immune System Interventions
| Term | Word Origin | Definition |
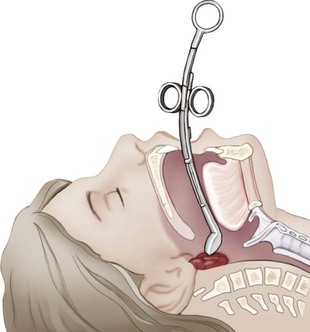
| adenoidectomy | adenoid/o adenoid -ectomy cutting out |
Removal of the adenoids (pharyngeal tonsils) (Fig. 8-22). |
| biopsy (bx) of lymphatic structures | bi/o life -opsy viewing lymphat/o lymph -ic pertaining to |
Removal of the lymph nodes or lymphoid tissue as a means of diagnosis and treatment. |
| lymphadenectomy | lymphaden/o lymph gland -ectomy cutting out |
Removal of a lymph node. |
| splenectomy | splen/o spleen -ectomy cutting out |
Removal of the spleen. |
7. cutting out the spleen ___________________________________________________________________________
8. cutting out the pharyngeal tonsils ________________________________________________________________
9. stopping blood __________________________________________________________________________________
10. cutting out a lymph node ________________________________________________________________________
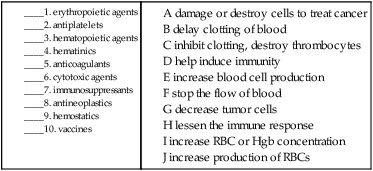
Pharmacology
Blood Drugs
anticoagulants: Prevent or delay the coagulation of blood and the formation of thrombi. Examples include heparin, warfarin (Coumadin), enoxaparin (Lovenox), and apixaban (Eliquis).
antiplatelets: Inhibit the function of platelets or destroy them. Examples include aspirin, clopidogrel (Plavix), dipyridamole (Persantine), ticlopidine (Ticlid), and abciximab (ReoPro).
blood-flow modifiers: Promote blood flow by keeping platelets from clumping or decreasing blood viscosity. Examples include the prescription medications cilostazol (Pletal) and pentoxifylline (Trental) and the herbal product ginkgo biloba.
colony-stimulating factors (CSFs): Stimulate the production of white blood cells in the bone marrow. The two kinds are granulocyte CSF (G-CSF) and granulocyte-macrophage CSF (GM-CSF). Available synthetic agents of each type are filgrastim (Neupogen) and sargramostim (Leukine), respectively.
erythropoietic agents: Increase production of RBCs by stimulating erythropoiesis. Two available agents are epoetin alfa (Epogen, Procrit) and darbepoetin alfa (Aranesp).
hematinics: Increase the number of erythrocytes and/or hemoglobin concentration in the erythrocytes usually to treat iron-deficiency anemia. Examples are iron supplements and B-complex vitamins.
hematopoietic agents: Stimulate blood cell production. Subdivisions of this class include colony-stimulating factors, erythropoietic agents, and thrombopoietic factors.
hemostatics: Help stop the flow of blood. Examples include aminocaproic acid (Amicar) and tranexamic acid (Cyklokapron).
thrombopoietic factors: Stimulate the production of thrombocytes or platelets. Oprelvekin (Neumega) is an available agent.
Immune Drugs
antineoplastics: Treat cancer by preventing growth or promoting destruction of neoplastic (tumor) cells. Numerous drugs, including methotrexate and rituximab (Rituxan), fall into this category.
antiretrovirals: Minimize the replication of HIV and its progression into AIDS. Examples include zidovudine or AZT (Retrovir) and efavirenz (Sustiva).
corticosteroids: Steroids that suppress the immune system and reduce inflammation. Examples include fluticasone (Flovent, Flonase), hydrocortisone (Cortizone), and prednisone (Rayos).
cytotoxic agents: Damage or destroy cells to treat cancer; often act as immunosuppressants or antineoplastics.
immune modulators: Reduce the impact of immune system disorders. Dimethyl fumarate (Tecfidera) is an example of a drug used to treat multiple sclerosis.
immunosuppressants: Minimize the immune response. Examples include azathioprine (Imuran), cyclophosphamide (Cytoxan), cyclosporine (Sandimmune), and tacrolimus (Prograf).
protease inhibitors: Antiretrovirals used to treat HIV infection. By blocking the production of an essential enzyme called protease, these drugs keep the virus from replicating. Examples are indinavir (Crixivan), nelfinavir (Viracept), and saquinavir (Invirase).
vaccines: Modified disease-causing microbial components administered to induce immunity or reduce the pathological effects of a disease. Examples are the measles, mumps, rubella, and chickenpox vaccine. A vaccination is an injection or oral solution derived from dead or weakened (attenuated) virus.
Recognizing Suffixes for PCS
Suffixes and Root Operations for the Blood, Blood-Forming Organs, and Immune Mechanisms
| Suffix | Root Operation |
| -ectomy | Excision, resection |
| Abbreviation | Meaning |
| A, B, AB, O | blood types |
| AIDS | acquired immunodeficiency syndrome |
| ALL | acute lymphocytic leukemia |
| ALPS | autoimmune lymphoproliferative syndrome |
| AML | acute myelogenous leukemia |
| basos | basophils |
| BMP | basic metabolic panel |
| BMT | bone marrow transplant |
| BUN | blood urea nitrogen |
| bx | biopsy |
| CBC | complete blood cell count |
| Cl | chloride |
| CLL | chronic lymphocytic leukemia |
| CML | chronic myelogenous leukemia |
| CMP | comprehensive metabolic panel |
| CO2 | carbon dioxide |
| DIC | disseminated intravascular coagulopathy |
| diff | differential WBC count |
| EBV | Epstein-Barr virus |
| eosins | eosinophils |
| ESR | erythrocyte sedimentation rate |
| G6PD | glucose-6-phosphate-dehydrogenase |
| GVHD | graft-versus-host disease |
| Hb, Hgb | hemoglobin |
| Hct | hematocrit, packed-cell volume |
| HDN | hemolytic disease of the newborn |
| HIV | human immunodeficiency virus |
| HSC | hematopoietic stem cell |
| Ig | immunoglobulin |
| K | potassium |
| lymphs | lymphocytes |
| MCH | mean corpuscular hemoglobin |
| MCHC | mean corpuscular hemoglobin concentration |
| Na | sodium |
| neuts | neutrophils |
| NK | natural killer cells |
| PCV | packed-cell volume, hematocrit |
| plats | platelets, thrombocytes |
| PMNs, polys | polymorphonucleocytes |
| PT | prothrombin time |
| PTT | partial thromboplastin time |
| RBC | red blood cell (count) |
| segs | segmented neutrophils |
| SIRS | systemic immune response syndrome |
| stabs | band cells |
| WBC | white blood cell (count) |