Bites and Stings From Arthropods and Mosquitoes
Disorders
Brown (“Fiddleback” or “Recluse”) Spiders
Necrotic arachnidism, or loxoscelism, is caused by spiders of the genus Loxosceles and other spiders that deposit a venom characterized by its local dermonecrotic activity. The fiddleback spider (see Plate 14) carries the characteristic violin-shaped marking on the dorsum of its cephalothorax. The clinical spectrum of loxoscelism ranges from mild and transient skin irritation to severe local necrosis accompanied by hematologic and renal pathologic conditions.
Signs and Symptoms
1. Most common presentation is an isolated cutaneous lesion.
2. Local symptoms begin the moment of the bite, with a sharp stinging sensation, although some patients report no awareness of having been bitten.
3. Stinging subsides over 6 to 8 hours and is then replaced by aching and pruritus.
4. Site becomes edematous, with an erythematous halo surrounding an irregularly shaped violaceous center of incipient necrosis; white ring of vasospasm and ischemia may be discernible between the central lesion and the halo.
5. Often erythematous margin spreads irregularly, in a gravitationally influenced pattern that leaves the original center near the top of the lesion.
6. In more severe cases, serous or hemorrhagic bullae arise at the center within 24 to 72 hours, with an underlying eschar (see Plate 15).
7. Systemic reactions: hemoglobinuria within 24 hours of envenomation; fever, chills, maculopapular rash, weakness, leukocytosis, arthralgias, nausea, and vomiting within 24 hours of the bite
Treatment
1. Apply cold compresses intermittently for the first 4 days after the bite. Do not apply heat.
2. If the wound appears infected, apply a topical antiseptic (mupirocin, bacitracin) under a sterile dressing. Administer an oral antibiotic such as cephalexin, dicloxacillin, or erythromycin (see Appendix H).
3. Seek advanced medical care to consider adjunctive measures for the bite wound and to evaluate for hospitalization for coagulopathy or renal failure caused by hemolysis and hemoglobinuria.
4. Obtain appropriate tetanus prophylaxis (when available).
5. Reported therapies include dapsone, glucocorticoids, hyperbaric oxygen, electric shock, antivenom, metronidazole, diphenhydramine, phentolamine, and cyproheptadine, although there is scant evidence to support their efficacy.
Widow Spiders
Female spiders of the genus Latrodectus carry the characteristic hourglass marking on the ventral abdomen (see Plate 16).
Signs and Symptoms
1. Initial bite is sometimes sharply painful, but often nearly painless, with only a tiny papule or punctum visible; surrounding skin slightly reddened and sometimes indurated; in many cases, no further progression of symptoms occurs.
2. Neuromuscular symptoms: can become dramatic within 30 to 60 minutes as involuntary spasm and rigidity affect the large muscle groups of the abdomen, limbs, and lower back; worst pain usually occurs within the first 8 to 12 hours but may remain severe for several days.
3. Predominantly abdominal presentation may resemble an acute abdomen
4. Priapism, fasciculations, weakness, ptosis, thready pulse, fever, salivation, diaphoresis, vomiting, bronchorrhea, pulmonary edema, rhabdomyolysis, hypertension with or without seizures
5. Characteristic pattern of facial swelling, known as Latrodectus facies, may develop hours after the bite.
Treatment
1. Cleanse the bite site. Apply a cold pack (ice pack) to the bite site. Provide tetanus prophylaxis (if available).
2. For muscle spasm, administer a benzodiazepine (e.g., diazepam 5-10 mg IV/IM, or lorazepam 1-2 mg IV/IM) or narcotics (e.g., morphine 4-8 mg IV/IM/SC).
3. Administer pain medication (IV opiates preferable).
4. Monitor the patient for hypertension.
a. Administer a centrally acting or vasodilating antihypertensive if the patient develops urgent hypertension and such a drug is available (e.g., nifedipine 30-60 mg ER PO daily, nicardipine 20-40 mg PO q8hr, or nicardipine IV drip started at 5 mg/h IV and increased 2.5 mg/h q5-15 min prn to a maximum of 15 mg/h).
b. Be alert for a seizure associated with rapid elevation in blood pressure.
5. Antivenom is available in the United States from Merck and Co.; in Australia from Commonwealth Serum Laboratories; and in South Africa from the National Health Laboratory Service. In general, antivenom is recommended for respiratory arrest, seizures, uncontrolled hypertension, or pregnancy. The usual dose is one to three vials or ampules intravenously.
6. All symptomatic children, pregnant women, and patients with a history of hypertension with suspected or confirmed envenomations should be admitted to a hospital for treatment and observation.
Funnel-Web Spiders
Funnel-web spiders (see Plate 17) are large, aggressive spiders that deliver a potent neurotoxin.
Signs and Symptoms
1. Intense pain at the bite site, with or without a local wheal surrounded by erythema lasting for 30 minutes; localized sweating
a. Begins minutes after venom injection, with local piloerection and muscle fasciculation; becomes generalized over the next 10 to 20 minutes
b. Intense pain at the bite site; perioral tingling, nausea and vomiting, diaphoresis, salivation, lacrimation, diarrhea
Treatment
1. In the field, apply the pressure immobilization technique for venom sequestration at the bite site (see Chapter 37).
2. Give specific antivenom, which is developed in rabbits and is the mainstay of treatment. Adult and pediatric dose is two ampules (100 mg purified IgG per ampule) of antivenom administered intravenously every 15 minutes until symptoms improve.
3. Be aware that general management, in addition to antivenom administration, is supportive.
Banana (Brazilian Wandering or Armed) Spiders
Signs and Symptoms
1. Severe local pain that radiates up the extremity into the trunk, followed within 10 to 20 minutes by tachycardia, hypertension, hypothermia, profuse diaphoresis, salivation, vertigo, visual disturbances, nausea and vomiting, and priapism.
2. If death occurs (usually in 2 to 6 hours), it is usually caused by respiratory paralysis.
Treatment
1. Treat mild envenomation symptomatically by infiltrating the bite site with a local anesthetic.
2. Be aware that narcotics may potentiate the venom’s respiratory depressant effect and should not be used.
3. For severe envenomation, administer monovalent antivenom (Belo Horizonte) or polyvalent antivenom (Sero Antiaracidico Polivalente, Instituto Butantan, available in Brazil).
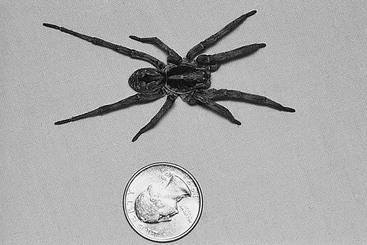
Wolf Spiders
Wolf spiders are diurnal predators that are usually a mottled dark gray or brown (Fig. 38-1).
Tarantulas
Tarantulas are large, slow spiders (Fig. 38-2) capable of inflicting a painful bite when threatened. Several varieties possess urticating hairs, which they flick by the thousands through the air into an attacker’s skin and eyes.

FIGURE 38-2 Mature female tarantula Aphonopelma iodius. (Courtesy Michael Cardwell & Associates, 1997.)
Treatment
1. Therapy is supportive and based on symptoms. To remove urticating hairs, apply and remove sticky tape from the skin in a few repeated applications.
2. Elevate the bitten extremity and immobilize it to reduce pain.
3. Administer analgesics as needed.
4. Topical or systemic corticosteroids and oral antihistamines may be used for urticating hair exposure.
5. For eye exposure, irrigate the eyes, and then consider ophthalmic antibiotic/corticosteroid ointment (e.g., combination bacitracin/neomycin/polymyxin B/hydrocortisone ophthalmic ointment q3-4h for 5-7 days) for keratoconjunctivitis, and follow up with an ophthalmologist as soon as possible.
Hobo Spiders
Treatment
1. Apply cold compresses intermittently for the first 4 days after the bite. Do not apply heat.
2. If the wound appears infected, apply a topical antiseptic (mupirocin, bacitracin) under a sterile dressing. Administer an oral antibiotic such as cephalexin, dicloxacillin, or erythromycin (see Appendix H).
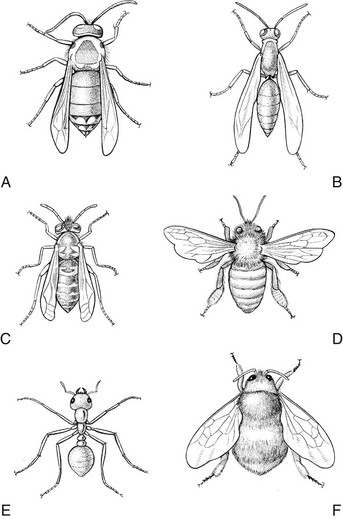
Hymenoptera (Bees, Wasps, and Ants)
By far the most important venomous insects are members of the order Hymenoptera, including bees, wasps, and ants (Fig. 38-3). The abdomen and thorax are connected by a slender pedicle, which may be quite long in certain wasps and ants.
Signs and Symptoms
1. Instantaneous pain, followed by a wheal-and-flare reaction, with variable edema. Most stings are on the head and neck, followed by the foot, leg, hand, and arm. Stings may occur in the mouth, pharynx, or esophagus if the insects are accidentally ingested.
2. Fire ant stings may produce vesicles that subsequently become sterile pustules; this is caused by the ant grasping the skin with mouthparts and inflicting multiple stings (Fig. 38-4).
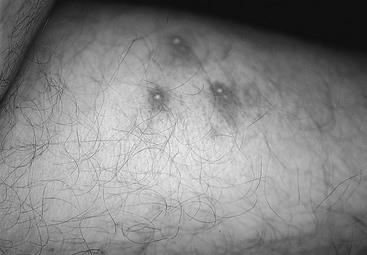
FIGURE 38-4 Fire ant lesions.
3. In the case of multiple bee, wasp, yellow jacket, or hornet stings, vomiting, diarrhea, generalized edema, dyspnea, hypotension, and collapse may develop. The lethal dose of honeybee venom has been estimated at 500 to 1500 stings.
4. Large local reactions are relatively common, spreading more than 15 cm (5.9 inches) beyond the sting and persisting longer than 24 hours.
a. Reactions occur in areas remote from the sting and typically include pruritus, hives, difficulty breathing, nausea, papular urticaria, and angioedema. Other symptoms include abdominal pain and vomiting.
b. When reaction is life threatening, there is marked respiratory distress, hypotension, loss of consciousness, and arrhythmias.
c. Most fatalities occur from anaphylaxis, and most of these occur within 1 hour of the sting.
Treatment
1. Be aware that the treatment of anaphylactic reaction follows conventional guidelines, as follows:
a. Maintain the airway, and administer oxygen (if available).
b. Obtain intravenous or intraosseous access. Administer lactated Ringer’s or normal saline solution to support the systolic blood pressure at a level of at least 90 mm Hg.
c. Administer epinephrine. Begin with aqueous epinephrine 1 : 1000 intramuscularly in the deltoid region. The dose for adults is 0.3 to 0.5 mL, and for children 0.01 mL/kg. An alternative is to inject the contents of an EpiPen or EpiPen Jr. intramuscularly into the lateral thigh region. Alternative products are the Twinject or Twinject Jr., or Adrenadick. Repeat in 20 minutes if relief is partial. If the reaction is limited to pruritus and urticaria, there is no wheezing or facial swelling, and the patient is older than 45 years, administer an antihistamine and reserve epinephrine for a worsened condition.
d. In the presence of profound hypotension, when skin is not adequately perfused, 2 to 5 mL of a 1 : 10,000 epinephrine solution may be given by slow IV push, or an infusion may be initiated by mixing 1 mg in 250 mL and infusing at a rate of 0.25 to 1 mL/min.
e. Relieve bronchospasm. Administer micronized albuterol or metaproterenol by handheld metered-dose inhaler.
f. Administer antihistamines. Manage mild reactions with diphenhydramine, 50 to 75 mg IV, IM, or PO. The dose for children is 1 mg/kg. Nonsedating antihistamines, such as fexofenadine 60 mg or cimetidine 300 mg, are adjuncts.
g. Administer corticosteroids. If the reaction is severe or prolonged or if the patient is regularly medicated with corticosteroids, administer hydrocortisone 200 mg, methylprednisolone 50 mg, or dexamethasone 15 mg, IV with a 5-day oral course or 10-day oral taper to follow. The parenteral dose of hydrocortisone for children is 2.5 mg/kg. If the therapy is initiated orally, administer prednisone, 60 to 100 mg for adults and 1 mg/kg for children.
2. For mild hymenopteran stings, apply ice packs to provide relief.
3. Be aware that a honeybee or yellow jacket may leave an embedded stinger. Remove the stinger (and possibly, attached venom sac) as quickly as possible with a sharp edge or forceps. Do not be overly concerned about squeezing the sac—it is more important to remove the stinger and sac as quickly as possible.
4. Note that a home remedy such as a paste of unseasoned meat tenderizer or baking soda is of variable usefulness, although some report the former to be effective. Topical anesthetics in “sting sticks” have limited usefulness.
5. Because infection is common, apply antimicrobial ointment such as mupirocin to cover the wound. Debridement of fire ant blisters is not recommended.
6. Envenomation from multiple hymenopteran stings may require more aggressive therapy, including intravenous calcium gluconate (5 to 10 mL of 10% solution) in conjunction with a parenteral antihistamine and corticosteroid to relieve pain, swelling, and nausea and vomiting. A corticosteroid, such as methylprednisolone, 24 mg the first day then tapered over 5 days, often hastens resolution of a large local reaction to a bee or wasp sting.
7. Manage delayed serum sickness in response to multiple hymenopteran stings with a corticosteroid such as prednisone, 60 to 100 mg for adults and 1 mg/kg for children, tapered over 2 weeks.
Lepidoptera (Caterpillars)
Signs and Symptoms
1. With caterpillars that have hollow spines and venom glands, instant nettling pain, followed by redness and swelling, after direct contact with the live insect
a. Ordinarily, no systemic manifestations; symptoms subsiding within 24 hours
b. Possibly intense pain with central radiation, accompanied by nausea and vomiting, headache, fever, and lymphadenopathy
2. With attached or detached spines from certain caterpillars or moths, itching and erythematous, papular, or urticarial rash within a few hours to 2 days after contact
Treatment
1. Apply adhesive tape, a commercial facial peel, or a thin layer of rubber cement to remove spines.
2. Administer an oral antihistamine and/or a nonsteroidal antiinflammatory drug. If the dermatitis is severe and persistent, consider administering a corticosteroid such as prednisone, 60 to 100 mg for adults and 1 mg/kg for children, tapered over 10 days. An oral antihistamine such as fexofenadine may be helpful. Pain medication is added as needed to control discomfort.
Hemiptera (Sucking Bugs)
“Sucking bugs” have sucking mouthparts, generally in the form of a beak. Included are the assassin bugs, kissing bugs (see Fig. 38-6, B), and flying bedbugs. Many of these bugs bite at night on exposed parts of the body. The bites themselves may be painless.
Signs and Symptoms
1. On initial exposure, usually no reaction
2. With repeated bites, erythematous pruritic papules that may persist for up to 1 week; bites often grouped in a cluster or line and may be accompanied by giant urticarial wheals, lymphadenopathy, hemorrhagic bullae, and fever
Beetles
Signs and Symptoms
1. With the blister beetle, contact painless and seldom remembered by the patient; blisters induced by cantharidin toxin appear 2 to 5 hours after contact, generally as single or multiple areas, usually 5 to 50 mm (0.2 to 2 inches) in diameter and thin walled; unless broken or rubbed, they are not usually painful
2. With the rove beetle, vesicant substance is an alkaloid; if the beetle is crushed or rubbed on the skin, redness occurs after several hours, followed by a crop of small blisters that persist for 2 to 3 days; conjunctivitis occurs if the secretion is rubbed into the eyes
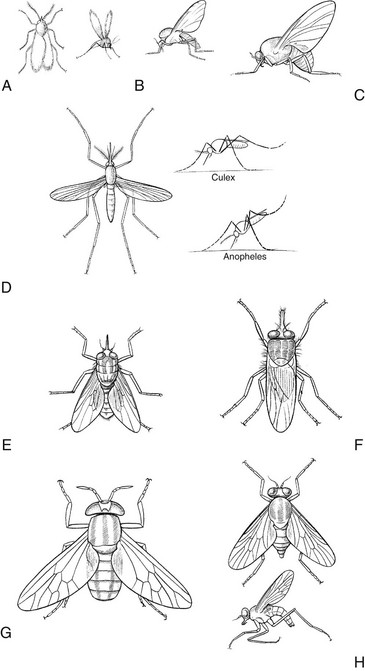
Diptera (Two-Winged Flies, Biting Midges, and Mosquitoes)
Insects of this order have one pair of wings and are indiscriminate feeders on feces and human foodstuffs (Fig. 38-5). These habits make them by far the most important arthropod vectors of human disease. See Chapter 39 for information about protection against blood-feeding arthropods.
Mosquitoes
Treatment
1. Immediately after the bite, apply a cold (ice) pack.
2. Apply a topical antipruritic lotion or cream.
3. If the reaction is severe or prolonged, consider the administration of a corticosteroid such as prednisone, 60 to 100 mg for adults and 1 mg/kg for children, for a 5-day course or tapered over 7 to 14 days. A topical corticosteroid cream or ointment may be helpful.
Dengue (Fever)
Signs and Symptoms
1. From bite to clinical infection, 4- to 6-day incubation period
2. High fever (>39° C [102.2° F]), myalgias, headache, arthralgias, and rash
3. Positive tourniquet test for capillary fragility: the appearance of 20 or more petechiae over a square-inch patch on the forearm after deflation of the blood pressure cuff (held for 5 minutes between systolic and diastolic pressures)
4. Irritability, depression, encephalitis, seizures
5. Differentiation between dengue fever and dengue hemorrhagic fever (DHF) is development of plasma leakage in DHF. Following 2 to 7 days of higher fever come bleeding (ranging from petechiae, ecchymoses, epistaxis, and mucosal bleeding to gastrointestinal bleeding and hematuria), thrombocytopenia (<100,000/mm3), hemoconcentration, and hepatomegaly. Other symptoms include abdominal pain, nausea and vomiting, and restlessness or lethargy.
Treatment
1. Prognosis for patients with dengue fever is generally good, with an acute phase of 1 week and up to 2 weeks of convalescence with general malaise and anorexia. DHF or dengue shock syndrome have more dire prognoses.
2. Resuscitate aggressively with fluid and electrolytes.
3. Use acetaminophen as an antipyretic, and do not use aspirin.
4. Provide blood transfusion for severe anemia; consider administration of platelets and fresh frozen plasma for severe bleeding only if attributed to coagulopathy.
West Nile Virus
Signs and Symptoms
1. The incubation period from bite to clinical infection is 3 to 14 days.
2. Most infections are asymptomatic or associated with a mild influenza-like illness with fever, malaise, fatigue, difficulty concentrating, headache, nausea, vomiting, anorexia, lymphadenopathy, and rash.
3. Severe infections include encephalitis, meningitis, or meningoencephalitis. Encephalitis may present with parkinsonian features or other movement disorders, such as myoclonus or intention tremor, or with acute flaccid paralysis or asymmetric weakness.
Cutaneous Myiasis
Signs and Symptoms
1. As the larva grows under the skin, the initial pruritic papule becomes a furuncle with a characteristic central opening from which serosanguineous fluid exudes (see Plate 18).
2. Pain often accompanies movement of the older larvae, but lesions are not particularly tender to palpation.
3. The tip of the larva may protrude from the central opening, or bubbles produced by its respiration may be seen.
4. Lymphadenopathy, fever, and secondary infection are rare.
Treatment
1. Sometimes simple pressure will extrude the organism, particularly if it is small.
2. Occlusion of the breathing hole with heavy oil, nail polish, or animal fat (e.g., bacon) may cause the larva to emerge sufficiently for it to be grasped and withdrawn.
3. Alternatively, inject about 2 mL of local anesthetic into the base of the lesion, thus extruding the larva by fluid pressure.
4. If you attempt surgical excision under local anesthesia, take care not to break or rupture the larva because this might result in an inflammatory reaction that predisposes to infection.
Lice (Order Anoplura)
Signs and Symptoms
1. Small, red macule in response to secretions released by the louse during biting and feeding
2. Characteristic body louse bite: a central hemorrhagic punctum in many of the macules
3. Excoriations, crusts, eczematization in a parallel pattern from scratching, particularly on the shoulders, trunk, and buttocks (favorite sites for bites)
4. Severe pruritus and inflammation caused by sensitization after repeated exposure to bites; patient possibly infested for weeks before pruritus becomes marked
5. Occipital and posterior cervical adenopathy associated with head lice
Treatment
1. Treat head lice with one application of 1% permethrin cream rinse or 0.5% malathion lotion. Hair should be washed, rinsed, and dried, and the treatment preparation is applied for 10 to 20 minutes before being washed off. A fine-toothed comb may be used to remove nits after rinsing. Combing should be repeated in 1 to 2 days to confirm treatment success. If head lice are resistant, use 0.3% pyrethrins and 3% piperonyl butoxide in combination. Use 1% hexachlorocyclohexane (lindane) shampoo for patients intolerant of permethrin. Note that lindane is contraindicated in children, infants, and pregnant women, and should be used only as a last resort for elders. Apply it to the wet hair, lather, and leave it in place for 4 minutes before rinsing. Repeat the treatment 7 to 10 days later as a precaution in case some nits were not killed by the first application.
2. Treat body lice with the same medications, but be aware that parasites and nits are not usually found on the skin. These must be eradicated from the clothing. Take a good bath, and launder all clothing.
3. Treat pubic lice with the same medications. One method is to apply permethrin 1% cream rinse for 10 to 20 minutes and then rinse. Another method is to rub crotamiton lotion into the affected area daily for several weeks to destroy hatching ova and prevent a persistent infection. Manage eyelash infection by careful application of physostigmine ophthalmic ointment, using a cotton-tipped applicator.
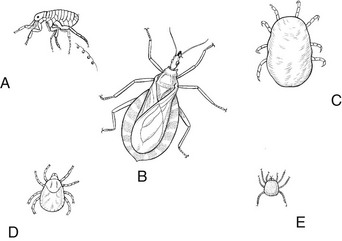
Fleas (Order Siphonaptera) (Fig. 38-6, a)
Signs and Symptoms
1. Small, central, hemorrhagic punctum surrounded by erythema and urticaria; bullae or even ulceration after bite in highly sensitive individuals
2. Intensely pruritic, with scratching often resulting in crusting and the development of impetigo
3. Tungiasis caused by burrowing flea (jigger, chigo, sand flea), usually on the feet, buttocks, or perineum of a person who wears no shoes or frequently squats
Treatment
1. Relieve pruritus by applying corticosteroid creams or calamine lotion with phenol.
2. Administer a systemic antihistamine to help control itching.
3. Clean excoriations, and apply a topical antiseptic ointment such as mupirocin.
4. With a burrowing flea infestation (tungiasis), remove the burrowing flea or a pustule will rupture, leaving an ulcer.
5. Preparations containing 9.1% imidacloprid eliminate or reduce fleas on dogs when applied to the skin. An oral preparation used for dogs and cats contains lufenuron, an inhibitor of insect development.
Mites (Class Arachnida, Order Acarina)
Signs and Symptoms
1. Hallmark of scabies: severe nocturnal pruritus
a. Itching also provoked by any warming of the body
b. Elapsed time of 4 to 6 weeks between infestation and onset of severe pruritus
2. Cutaneous manifestations: an epidermal burrow (a linear or serpentine track, rarely longer than 5 to 10 mm [0.2 to 0.4 inch]) with a predilection for the interdigital spaces, palms, flexor surfaces of the wrists, elbows, feet, ankles, belt line, anterior axillary folds, lower buttocks, penis, and scrotum
Treatment
1. A single overnight application of 5% permethrin cream is curative. Also apply the chemical beneath the fingernails. Symptoms may persist for more than a month until the mite and mite products are shed with the epidermis. One percent hexachlorocyclohexane (lindane) cream or lotion is curative, although it is contraindicated in infants and pregnant women.
2. Sulfur in petrolatum 5% to 10% or another suitable vehicle applied for 3 consecutive nights is an alternative, as is crotamiton cream 10% or lotion applied for 2 consecutive nights.
3. Treat contacts simultaneously. Clothing and linens should be laundered the morning after treatment to kill mites that may have strayed from the skin.
Trombiculid (Chigger) Mites (see Fig. 38-6, E)
Signs and Symptoms
1. Maddeningly pruritic hemorrhagic punctum that usually becomes surrounded by intense erythema within 24 hours
2. Bites may number in the hundreds and can be associated with an allergic reaction.
3. Blisters, purplish discoloration, swelling of feet and ankles, secondary infection in excoriated skin
Ticks (see Fig. 38-6, c and D)
Tick Paralysis
Signs and Symptoms
1. From 5 to 6 days after the adult female tick attaches: restlessness, irritability, paresthesias in the hands and feet
2. Over the ensuing 24 to 48 hours: ascending, symmetric, and flaccid paralysis with loss of deep tendon reflexes; weakness usually greater in the lower extremities
3. Within 1 to 2 days: severe generalized weakness possible, accompanied by bulbar and respiratory paralysis
Lyme Disease
Signs and Symptoms
a. Average 7 to 10 days (range: 3 to 32 days) after inoculation, patient develops an expanding, annular, and erythematous skin lesion (erythema migrans) (Fig. 38-7; see Plate 19)
b. Initially, central red macule or papule, but as lesion expands, partial central clearing usually seen while outer borders remain bright red
c. Borders usually flat but may be raised
d. Center of some early lesions intensely red and indurated, vesicular, or necrotic; sometimes area develops multiple red rings within the outside margin, or the central area turns blue before clearing
e. Lesion diameter 15 cm (5.9 inches) (range: 2 to 60 cm [0.8 to 23.6 inches]) and may be anywhere on the body, although most common sites are thigh, groin, and axilla
f. Lesion warm to the touch and usually described as burning, but occasionally as itching or painful
g. Rash fading after an average of 28 days (range: 1 to 14 weeks) without treatment; with antibiotics, lesion resolves after several days
h. Constitutional symptoms accompany erythema migrans, but usually mild and consisting of regional lymphadenopathy, fever, fatigue, neck stiffness, arthralgia, myalgia, and malaise
i. Annular erythematous lesions occur hours after bite, representative of hypersensitivity reaction and not to be confused with erythema migrans.
2. Stage II (early disseminated)
a. During hematogenous spread of microorganisms (a few days to weeks after bite), multiple annular skin lesions in 20% to 50% of patients
• Generally smaller, migrate less, and lack indurated centers
b. Other skin manifestations: malar rash; rarely, urticaria
c. Most common constitutional symptoms: malaise and fatigue, which may be severe and are usually constant throughout the duration of the illness
d. Fever, typically low grade and intermittent, is common
e. Tender regional lymphadenopathy along distribution of erythema migrans or posterior cervical chains
f. Generalized lymphadenopathy and splenomegaly
g. Symptoms of meningeal irritation in some patients, including severe intermittent headaches, stiff neck with extreme forward flexion, and lack of Kernig or Brudzinski sign
h. Mild encephalopathy with somnolence, insomnia, memory disturbances, emotional lability, dizziness, poor balance, and clumsiness
j. Musculoskeletal complaints, including arthralgias; migratory pain in tendons, bursae, and bones; and generalized stiffness or severe cramping pain, particularly in the calves, thighs, and back
k. Symptoms of hepatitis and generalized abdominal pain
l. Conjunctivitis in 10% to 15% of patients
m. Neurologic manifestations an average of 4 weeks after the onset of erythema migrans, including meningoencephalitis, with headache as a major symptom; facial nerve palsy (in 11% of Lyme disease patients and 50% of patients with Lyme disease meningitis, but may be an isolated finding); radiculoneuritis (triad of meningitis, cranial neuritis, and radiculoneuritis suggests Lyme disease in the differential diagnosis)
n. Cardiac abnormalities in 4% to 10% of patients, including atrioventricular block that can progress to complete heart block
o. Arthritis in about 60% of untreated persons with erythema migrans
3. Knee most frequently involved, followed by the shoulder, elbow, temporomandibular joint, ankle, wrist, hip, and small joints of the hands and feet
4. Stage II (late disease)—begins a year or more after the onset of erythema migrans, although patients may present with stage III disease as the initial manifestation of Lyme disease
Treatment
1. For stage I disease in adults, give tetracycline 250 mg PO q6h, doxycycline 100 mg PO q12h, or amoxicillin or cefuroxime 500 mg PO q8h for 14 to 28 days. Another alternative not yet approved by the U.S. Food and Drug Administration is azithromycin, 200 mg PO q12h for 3 weeks. For stage I disease in children, give tetracycline or doxycycline at adult doses if older than 8 years. For children younger than 8 years, give amoxicillin 50 mg/kg/day PO divided q8h, or erythromycin 30 to 50 mg/kg/day PO divided q6h. Anticipate a Jarisch-Herxheimer reaction within the first 24 hours of therapy.
2. Treat any manifestations of stage II disease with the above agents for 21 to 28 days. Alternatively, administer ceftriaxone, 1 g IV q12h, for 2 to 4 weeks.
Prophylaxis
• Attached tick identified as an adult or nymphal I. scapularis tick (deer tick).
• Tick is estimated to have been attached for 36 hours or longer (by degree of engorgement or time of exposure).
• Prophylaxis is begun within 72 hours of tick removal.
• Local rate of infection of ticks with B. burgdorferi is 20% or higher (e.g., New England, parts of the mid-Atlantic states, and parts of Minnesota and Wisconsin).
• Doxycycline is not contraindicated (i.e., the patient is not younger than 8 years, pregnant, or lactating).
Relapsing Fever
Signs and Symptoms
1. Abrupt onset of fever lasting about 3 days, afebrile period of variable duration (average 6 to 7 days), and relapse with return of fever and other clinical manifestations
a. Fever usually high, greater than 39° C (102.2° F)
b. Initial febrile period averaging 3 days but possibly lasting 1 to 17 days
c. Febrile period terminating with rapid defervescence (the crisis), accompanied by drenching sweats and intense thirst
2. Pruritic eschar at the site of the tick bite possible but usually absent by the onset of clinical symptoms
3. Incubation period of about 7 days, then fever, frequently accompanied by shaking chills, severe headache, myalgias, arthralgias, muscular weakness, lethargy, upper abdominal pain, nausea, and vomiting
4. Splenomegaly, hepatomegaly, altered sensorium, peripheral neuropathy, pupillary abnormalities, pathologic deep tendon reflexes
5. Rash, ranging from a macular eruption to petechiae and erythema multiforme, developing in about 25% of patients
Treatment
1. Tetracycline and erythromycin are both effective. A 7- to 10-day course (500 mg PO q6h) of either drug is recommended.
2. A Jarisch-Herxheimer reaction is common after the first dose of antibiotics. It is often severe and may be fatal.
a. The reaction begins with a rise in body temperature and exacerbation of existing signs and symptoms. Vasodilation and fall in blood pressure follow.
b. Pretreat any patient who will be receiving the initial dose of an antibiotic to treat relapsing fever with an intravenous infusion of isotonic saline solution in anticipation of the Jarisch-Herxheimer reaction.
c. A lower initial dose of antibiotic may reduce the frequency of this reaction.
Rocky Mountain Spotted Fever
Signs and Symptoms
1. Ranges from mild, subclinical illness to fulminant disease with vascular collapse and death within 3 to 6 days of onset
2. Incubation period 2 to 14 days, with severe disease associated with the shorter incubation period
3. Typically a sudden onset of fever, chills, headache, and myalgias; fever is usually high, greater than 39° C (102.2° F)
4. Most characteristic feature: rash, which develops 2 to 5 days after the onset of illness in 85% to 90% of patients
a. Typically develops first on the wrists, hands, ankles, and feet, spreading rapidly in centripetal fashion to cover most of the body, including the palms, soles, and face
b. Lesions initially pink macules, 2 to 5 mm (0.1 to 0.2 inch) in diameter, that readily blanch with pressure
c. After 2 to 3 days: lesions fixed, darker red, papular, and finally petechial
d. Hemorrhagic lesions coalescing to form large areas of ecchymoses
e. Unfortunately, rash often absent on initial presentation, making diagnosis more difficult; in 10% to 15% of patients, no rash ever noted (“spotless fever”)
5. Other signs and symptoms: abdominal pain, vomiting, diarrhea, confusion, conjunctivitis, peripheral edema
6. Seizures possible during acute phase of illness but rarely persist
7. Lethargy and confusion common, possibly progressing to stupor or coma
Treatment
1. Initiate antibiotic therapy at the earliest suggestion of RMSF. Unfortunately, the classic triad of rash, fever, and tick bite is rarely present.
2. Give either tetracycline or chloramphenicol, both of which are very effective, although neither drug is rickettsicidal. These antibiotics inhibit the rickettsiae until an adequate immune response by the patient eradicates the infection.
a. Give tetracycline 500 mg PO q6h in adults and 25 to 50 mg/kg/day PO divided q6h in children.
b. Give chloramphenicol 50 mg/kg/day PO for adults and 75 mg/kg/day for children.
3. Continue treatment until the patient is afebrile for 48 hours, or for a minimum of 5 to 7 days. Be aware that relapses are common but may be treated with the same drug when they occur.
Ehrlichiosis
Signs and Symptoms
1. After an average incubation period of 7 days (range: 1 to 21 days): high fever, headache, chills or rigors, malaise, myalgia, anorexia
2. Rash, which may be maculopapular or petechial, in 20% to 40% of patients about 8 days after onset of illness
3. Severe complications: more likely in older persons and include cough, pneumonitis, dyspnea, respiratory failure, meningoencephalitis, and renal failure
Colorado Tick Fever
Signs and Symptoms
1. Usually begins with an abrupt onset of fever
a. Most characteristic feature of illness (seen in 50% of patients): biphasic, or “saddleback,” fever pattern
b. From 2 to 3 days of fever, followed by 1 or 2 days of remission, then an additional 2 to 3 days of fever
c. During fever, also have severe headache, myalgias, lethargy
2. Photophobia, ocular pain, anorexia, nausea, vomiting, abdominal pain
3. Macular or maculopapular rash in 5% to 12% of patients
4. Usually mild, but severe complications possible, especially in children younger than 10 years; include meningoencephalitis or hemorrhagic diathesis
5. Three weeks or longer required for full recovery, with most common persistent symptoms malaise and weakness
Babesiosis
Signs and Symptoms
1. Acute babesiosis: gradual onset of malaise, anorexia, and fatigue followed within several days to a week by fever, sweats, and myalgias
2. Less common symptoms: headache, nausea, vomiting, depression, shaking chills, splenomegaly, jaundice, hepatomegaly
3. No rash associated with disease
4. Hemolytic anemia more pronounced in splenectomized patients
Treatment
1. Currently treatment is only recommended for the seriously ill patient or the patient with asplenia, immunosuppression, or elder status.
2. For severe infections, give azithromycin 500 mg PO on day 1, followed by 250 mg PO on days 2 through 7, combined with atovaquone 750 mg PO q12h for 7 days.
3. Alternative therapy with similar efficacy but more side effects is a combination of clindamycin and quinine.
Prevention of Tick-Borne Diseases
Close and regular inspection of all parts of the body should be performed when traveling in tick-infested areas. Protective clothing (long pants cinched at the ankles or tucked into boots and socks) should be worn when in tick-infested areas. Spraying clothes with an insect repellent may provide an additional barrier against ticks (Box 38-1; see also Fig. 39-1). Adult ixodid ticks are generally on the body for 1 to 2 hours before attaching. See Chapter 39 for more information.
Scorpions
Centruroides exilicauda, the bark scorpion (see Plate 20) of Arizona, is usually less than 5 cm (2 inches) long, yellow to brown, and possibly striped. It carries the identifying subaculear tooth beneath its stinger. Some scorpions fluoresce under a “black light,” which can be used to inspect clothing, sleeping bags, etc. Other scorpions worldwide cause similar syndromes.
Signs and Symptoms
1. Begin immediately after envenomation and progress to maximum severity in 5 hours
2. Infants: extreme illness possible 15 to 30 minutes after a sting
3. Improvement without administration of antivenom within 9 to 30 hours
4. Paresthesias and pain persisting for days to 2 weeks
5. Grade I: local pain and paresthesias at the site of envenomation, which can be elicited by tapping on the sting site
6. Grade II: pain and paresthesias remote from the sting bite, along with local findings. The patient may complain of a “thick tongue” and “trouble swallowing.” Children and adults frequently rub their nose, eyes, and ears, and infants may show unexplained crying
7. Grade III: either cranial nerve or somatic skeletal neuromuscular dysfunction
a. Cranial nerve dysfunction: blurred vision, wandering eye movements (involuntary, conjugate, slow, roving); hypersalivation; difficulty swallowing; tongue fasciculation; upper airway obstruction; slurred speech
b. Somatic skeletal neuromuscular dysfunction: jerking of the upper extremities, restlessness, arching of the back, and severe involuntary shaking and jerking that may be mistaken for a seizure (true seizures are caused by some scorpion species)
8. Grade IV: both cranial nerve and somatic skeletal neuromuscular dysfunction
9. Hypertension, nausea, vomiting, hyperthermia, tachycardia, and respiratory distress also possible
Treatment
1. Control local pain with ice packs, which may be applied for 30 minutes each hour. Give oral analgesics as needed. Infiltration with a local anesthetic or application of a digital or regional nerve block may be used. Although not studied, topical anesthetic patches (e.g., Lidoderm patch) can also be used.
2. Observe the patient of mild to moderate (grade I to II) envenomation for progression to more severe symptoms (grade III to IV).
3. Avoid the use of narcotics, barbiturates, benzodiazepines, or other potent analgesics to control symptoms of agitation or motor hyperactivity unless prepared to definitively manage the airway because these agents may lead to apnea and loss of protective airway reflexes.
4. Manage hyperthermia from uncontrolled muscular activity with administration of acetaminophen or, if extremely severe, physical cooling methods.
5. Atropine may be used for severe bradycardia.
6. Sublingual (oral) nifedipine (5 to 10 mg by puncturing and swallowing the gelatin capsule) may be used to block excessive adrenergic tone. Alternatively, prazosin, a selective α-adrenergic blocker, may be given at an initial dose of 0.5 mg PO for adults and 0.25 mg PO for children, repeated at 4 hours and then q6h as needed for up to 24 hours.
7. Antivenom administration is controversial worldwide. Some recommend it for reversal of grade III envenomation with respiratory distress or grade IV envenomation. Administration carries the risk for anaphylaxis. Ideally, it should be administered in a hospital critical care setting as soon as possible.