Chapter 56 Bites and Injuries Inflicted by Wild and Domestic Animals
For online-only figures, please go to www.expertconsult.com ![]()
Wild and domestic animal bites are distinct from other injuries suffered by humans. Tearing, cutting, and crushing injuries may be combined with blunt trauma caused by falls. Animal bites may cause local infection, and offending bacteria reside in numerous environmental sources. However, few traumatic lacerations are as regularly contaminated with as broad a variety of pathogens as are animal bites. Domestic animal bites are common, and their incidence is rising.43,201,297 Wild animal attacks are often more spectacular; however, in the developed world, injuries from domestic animals have a much greater health and economic impact. Humans are not a preferred natural prey of any animal, and, although some attacks are predatory, most attacks are caused by fear of humans (real or perceived), territoriality, protective instinct, or accident. Unfortunately, wild animal attacks may be sensationalized by the lay press, and animals given anthropomorphic characteristics that do not accurately reflect their instinctive responses; this may lead to public misunderstanding of animal behavior. Press reports may ignore the fact that wild animal attacks are rare and that wild animals are far less likely to cause injury than are their domestic counterparts.
As human settlements and populations continue to grow and encroach on the natural world, the incidence of human–animal encounters will increase. Adventure-seeking humans may also seek out animal encounters that historically would have been avoided. A wolf sighting 100 years ago would have been cause for alarm, yet today people travel to Yellowstone National Park to see wolves in the wild and hope to get close enough to take pictures. The increased pressure of human proximity to animals increases the likelihood of an encounter resulting in a negative outcome (Figure 56-1).40
Other special features of human–animal encounters include attacking animals that may terrorize the victim and transmission of systemic diseases, many of which might cause substantial morbidity and mortality (for a discussion of zoonoses, see Chapter 59). In addition, treatment decisions are often made without a strong scientific basis, and management of wild animal attack victims is often based on a much more robust experience with domestic animal attacks (i.e., dog and cat bites).
General Epidemiology
According to the 2008 National Pet Owner Survey, 39% of all households in the United States own a total of 74.8 million dogs, and 34% own 88.3 million cats.10 During 1 year in Pennsylvania, county health officials reported 16,000 animal bites, 75% of which were dog related; the highest incidence of dog bite was among children less than 5 years old. Three-quarters of persons injured received wound treatment, and one-half received antimicrobials. Postexposure rabies prophylaxis administration was prescribed for attacks by species as follows: 44% for cats, 30% for dogs, 7% for raccoons, 4% for bats, 2.5% for squirrels, 2.1% for groundhogs, 2% for foxes, and 8% for all other species.230
Each year, dogs bite 1.8% of all Americans, resulting in 4.7 million wounds. More than 750,000 of these victims seek medical attention.75 Bites to children are common, especially among boys between the ages of 5 to 9 years.75 Over the course of 1 year in Pittsburgh, Pennsylvania, 790 dog bites were reported, but an estimated 1388 went unreported; the annual incidence was 58.9 bites per 10,000 individuals.81 Of 279 reported injuries caused by animals to travelers, 51% were caused by dogs, 21% by monkeys, 8% by cats, and 1% by bats.144 In India, where stray dogs cause 96% of rabies cases, the annual dog bite rate is 25.7 per 1000 individuals, and the most common victims are males.3,86
The annual incidence of cat bites in the United States is approximately 400,000.303 A cat bites one in every 170 people each year, and 80% of these bites become infected.156 Biting cats are typically stray females, and most human victims are female.
Of the approximately 30 million Americans who ride horses, 50,000 a year are treated for horse-related injuries in an emergency department, principally because the rider is unrestrained and can fall off while traveling at speeds of up to 64.4 km/hr (40 mph). Horses can kick with a force of up to 907 kg (1 ton), and frequently bite. A 2-year review of animal bites in Oslo, Norway, revealed that horses caused 2% of 1051 recorded bites; 53% of these horse bite victims were children.104
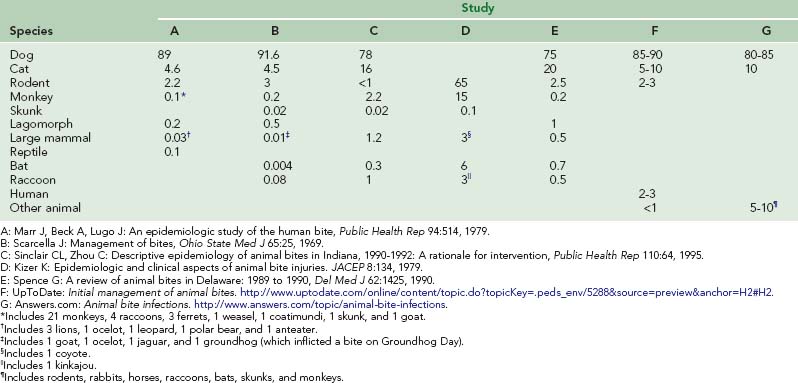
The American Ferret Association estimates that 6 to 8 million domesticated ferrets reside in the United States. The Centers for Disease Control and Prevention (CDC) reports that the number of bites inflicted by ferrets—65 reported bites in 10 years—is substantially lower than that caused by dogs and cats (i.e., between 1 and 3 million)23 (Table 56-1). In Arizona, 11 ferret bites were reported over 11 months; with the ferret population estimated at 4000, the reported bite-to-ferret population ratio is approximately 0.3%.316 The risk of attack by a ferret is greatest among infants and small children.
In Sweden, 3 in 1000 citizens are injured by animals each year.46 Domestic animals accounted for more than 90% of injuries, moose accounted for 6% (almost all were involved in auto accidents), and all other animals accounted for 4%. However, bites were not examined separately, and many injuries occurred during vehicular accidents with animals. Some officials estimate there are two additional bites for every one reported, but a survey of children between the ages of 4 and 18 years old estimated an incidence of more than 36 times the reported bite rate. These figures are most likely based on domestic bites, although this was not specifically stated.32,33 During a 7-year period in Texas, 2% of all large-animal–related trauma was caused by wild animal attacks.243 From 2001 to 2005, there were 472,760 reports by poison control centers of animal bites and stings, which is an average of 94,552 reports per year.202
A 2006 GeoSentinel review of injuries to travelers from 1998 to 2005 showed a total of 320 reported animal-related injuries (i.e., 1.8% of all reported injuries).144 The review revealed that, among travelers, women were more likely than men to be injured by animals. Men were more likely to be injured by dogs, women by monkeys, and children suffered animal injuries at a higher rate than any other travel-related injury. By geographic region, travelers were most likely to experience animal-related injuries in Southeast Asia, followed by Asia, Australia and New Zealand, Africa, Latin America, North America, and Europe.144
Typical Victim
No published reports characterize the typical wild animal attack victim. Two U.S. state health departments report that, if all animal bites (including domestic) are considered, animal bites occur most often among male children between the ages of 5 and 9 years.302,306 However, more than 90% of animal attacks in these states are caused by domestic animals, so this group may not accurately reflect the typical victim of a wild animal attack. In developing countries, many persons are exposed daily to biting animal species that are considered “exotic” in the developed world.
Persons in certain occupations in developed countries (e.g., veterinary and animal control workers, laboratory workers) are at greatest risk for wild animal bites. One study reported that 65% of veterinarians had suffered an animal-related injury during the preceding 12 months.200 The U.S. Bureau of Labor Statistics reported that, during a 5-year period, 186 occupational injury fatalities were caused by animal attacks and that the majority involved cattle.58 In one study of 102 animal control officers, the overall bite rate was 2 per 57 individuals per working day, which is 175 to 500 times the estimated rate for the general population (this study did not differentiate between wild and domestic animal bites).32 The incidence of biting varies with species exposure. In 2003, 93% of Wisconsin and Minnesota veterinarians were victims of dog or cat bites. Cattle and horses inflict the most injuries to veterinarians, with kicking, biting, and crushing being the top three mechanisms of injury.116
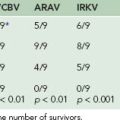
Several thousand people per year are killed by mammalian bites, with most of the deaths inflicted by maneating lions and tigers in Africa and Asia (Table 56-2). By way of comparison, the World Health Organization estimates that 5 million people per year are bitten and 125,000 killed by snakes and that additional millions are killed by insect-borne diseases.349
An estimated 200 persons are killed by animals in the United States each year; 131 of these die in traffic accidents involving deer.170 Bees kill approximately 43 persons, dogs 14, and rattlesnakes 10. Wild animals (e.g., bears, cougars) kill fewer people than do goats, rats, jellyfish, and captive elephants. More than 3 million people visit the wilderness in Yellowstone National Park every year, but the incidence of serious injuries by bears in the park is less than that of being struck by lightning.162
Circumstances Surrounding and Prevention of Animal Bites: Animal Behavior
Analysis of unintentional injuries shows that these are not random events but rather, are predictable events and have identifiable personal and environmental risk factors similar to those of diseases.350 For example, family pets cause most bites, and the animals are usually provoked in some way. Boys experience 150% to 250% the rate of injuries as compared with girls at every age350 (Table 56-3). Injuries are frequently sustained while playing with the animal.81 Most bites occur in the summer months during the late afternoon. Children sustain a higher percentage of head and neck bites than do adults and are more likely to require medical attention.130 Of all dog bites, 9% to 36% occur to the head and neck region, whereas this area is affected in 6% to 20% of persons who sustain cat bites.130 Understanding such patterns of animal bite injuries allows for improved prevention and treatment.
TABLE 56-3 Selected Demographics for Animal-Related Fatalities in the United States From 1991 to 2001* (Based on the International Classification of Diseases Reporting System Codes)
Prevention of animal bites requires thorough knowledge of the patterns of behavior and personalities of various species of animals. A person who wishes to avoid the bite of a particular species will often be able to gain expertise about that species’ behavior only from those who work with it regularly. Detailed information about animal behavior and the attack patterns of animals is also available on the Internet (Box 56-1).
BOX 56-1 Animal Behavior and Attack Prevention Websites
| Dog and cat bite prevention | http://www.cityoffortwayne.org/animal-bite-prevention.html |
| Dog bite prevention | http://www.petplace.com/dogs/preventing-dog-bites-things-to-do-before-you-get-a-dog/page1.aspx |
| Dog bite prevention and legal information | http://www.dogbitelaw.com |
| Moose attack prevention | http://www.survivaltopics.com/survival/survive-a-moose-attack/ |
| Cougar attack prevention | http://www.arkanimals.com/dlg/cougar_attack.htm |
| Wolf behavior and human encounters | http://fwp.mt.gov/wildthings/wolf/human.html |
| Hunter education | http://www.hunter-ed.com/index.html |
| General animal attack information | http://www.articlesbase.com/health-and-safety-articles/how-to-avoid-animal-attack-injury-444613.html |
| Wild animal attack compilation | http://www.attack.igorilla.com |
Basic Principles for Avoiding Animal Bites
Expert recommendations can reduce the chance of being attacked and bitten by a domestic animal (Box 56-2). Specific actions can be taken when an individual is threatened or under attack by a dog (Box 56-3). Dogs are guided by memory and instinct; fear and self-preservation are very strong instincts, so any perceived threat could lead to an attack. Territoriality is still ingrained in domestic dogs, even if humans provide for them. Protection of food can cause aggression, even in a docile dog. Any threat to a dog’s mate, offspring, or owner may result in an attack. Personality changes may lead to aggression; causes include illness (e.g., distemper) and physiologic factors (e.g., a female in heat).
BOX 56-2 Advice for Avoiding the Bites and Attacks of Common Pets*
Dogs
BOX 56-3
Suggested Actions If You Are Under Threat or Attacked By a Dog
Modified from Wilson S: Bite busters: How to deal with dog attacks, New York, 1997, Simon & Schuster; and wikiHow: How to handle a dog attack. http://www.wikihow.com/Handle-a-Dog-Attack.
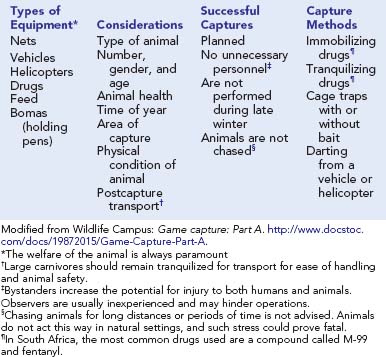
People often capture or restrain wild animals, thereby creating stress that may cause even the most benign animal to attack its captor. Allegedly tame animals are very likely to struggle. Even shy animals that are being captured for treatment of an injury may attack in self-defense and can inflict a life-threatening injury (e.g., goring). Therefore, all situations that involve animal restraint and capture are considered high risk, and careful study of the species’ behavior, the individual animal, and the physical environment and available resources should precede actual attempts at restraint (see Chapter 61).
Because people seem drawn to raising wild animals as pets,211 a large and lucrative market exists, particularly in the United States. No matter how they are raised, these animals remain wild and will never be as predictable, trustworthy, and nonaggressive as animals that have been domesticated for centuries. Often owners of these animals demonstrate a lack of common sense; consider the case of a pet Bengal tiger that attacked and killed its trainer, then did the same to its owner 6 weeks later.21,112
A major principle of animal behavior is that physical attack is often the animal’s last resort. Animals generally give ample warning regarding their intentions. Elaborate rituals and rules that encourage a nonviolent solution so that the victor may successfully defend its territory and itself with little or no injury govern spectacular contests between animals that occur in the wild. Humans can often avoid attack and injury by successfully interpreting visual, auditory, and olfactory warning signs. If a human slowly and carefully backs away without making sudden or threatening gestures, usually no harm will be done. However, the ideal reaction depends on the species. For example, mountain lions have been turned from a full charge by a human who acted aggressively or fought back.35 Given a choice of victims, such a predator prefers the fleeing and panicked victim who demonstrates expected behavior patterns.
If capture of an animal is essential, detailed preparation should be undertaken. For small animals, using nets or heavy cloth and wearing extremely heavy gloves and other protective clothing are advisable. Desperate animals can bite with tremendous force; large carnivores can easily amputate a gloved digit. A wolf can tear apart a stainless steel bowl with its teeth, and a hyena can bite through a 2-inch–thick wooden plank.92 Four men are needed to subdue an adult chimpanzee; an orangutan can maintain a one-fingered grip that an adult human cannot break. Larger animals generally require a team approach by animal control specialists with equipment such as nets, barriers, cages, and immobilizing drugs. Ideal immobilization techniques for various species are detailed in veterinary and wildlife management publications137,142 (Box 56-4).
Evaluation and Treatment of Injuries: Prehospital Care
Many of the complications and serious infections that occur as a result of animal bites are caused by inadequate first aid and delays in medical care. Local wound treatment should be initiated at the scene of the bite (Box 56-5); more than any other therapy, this can determine the course of healing. Simple first-aid measures must be initiated immediately unless definitive or better treatment is available within a short time. Pressure on the wound or pressure points controls most bleeding; avoid tourniquets unless blood loss cannot otherwise be controlled. If the victim is more than 1 hour from a treatment facility, cleanse the wounds at the scene as soon as resuscitation efforts are complete. Early cleansing reduces the chance of bacterial infection and is extremely effective for killing rabies and other viruses. Potable water, preferably boiled or treated with germicidal agents, is adequate for wound irrigation. Ordinary hand soap adds some bactericidal, virucidal, and cleansing properties. If 1% to 5% povidone–iodine in normal saline solution is available, it should be used as an irrigant. Alternatively, thoroughly irrigate the wound with at least a pint of soapy water and then gently debride it of dirt and foreign objects by swabbing with a soft, clean cloth or sterile gauze. Irrigation with a syringe is preferable (see Chapter 22).
BOX 56-5 Summary of Mandatory Animal Bite Wound Treatment for All Wounds
Selective Treatment (Wounds Selected By Risk Factors)
After cleansing, cover the wound with sterile dressings or a clean, dry cloth. Wounds of the hands or feet require immobilization. If the wounds are at high risk for infection, treatment is hours away, and an antibiotic such as amoxicillin–clavulanate (first line), a fluoroquinolone plus clindamycin, trimethoprim-sulfamethoxazole plus clindamycin, amoxicillin plus cephalexin (less effective), azithromycin, or doxycycline is available,1,102,308 then it is reasonable to start immediate treatment with an oral dose (Box 56-6). To most effectively prevent subsequent wound infection, antibiotics should be started within 1 hour of wounding. However, with a severe wound, it is worthwhile to provide the antibiotic, even if delivered substantially later. If antibiotics are unavailable, the wound is infection prone, and medical care is delayed, a simple remedy such as filling the wound with honey may be an effective antibacterial strategy.264 Because of its high osmolarity and weak hydrogen peroxide concentration when diluted, honey can be effective as an antibacterial when used in adequate quantities, although there are no randomized controlled trials to support this recommendation. The wound should be flooded with honey that has been slightly thinned with water and kept flooded like this until definitive treatment is available. The amount of honey needed will depend on the amount of exudate from the wound (because of dilution), and the frequency of dressing changes will depend on how rapidly the exudate dilutes the honey.
BOX 56-6
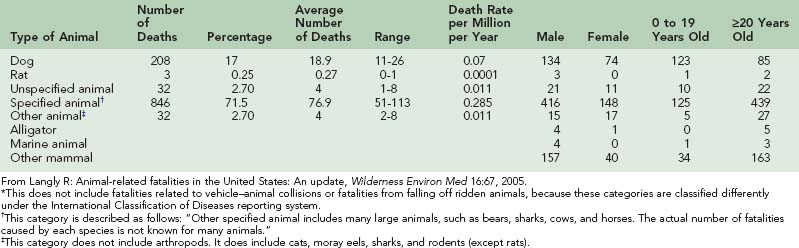
Recommended Empiric Oral Antibiotics for Bite Wound Prophylaxis and Treatment
| Antibiotic | Recommended Adult Dose | Recommended Child Dose* |
|---|---|---|
| Agent of Choice | ||
| A) Amoxicillin–clavulanate | 875/125 mg twice daily | 45 mg/kg per dose (amoxicillin component) twice daily |
| Alternate Combination Therapy: B or C (With Anaerobic Activity) Plus E, F, G, H, or I | ||
| B) Metronidazole | 500 mg three times daily | 10 mg/kg per dose three times daily |
| Or: | ||
| C) Clindamycin | 450 mg three times daily | 10 mg/kg per dose three times daily |
| Plus One of the Following: | ||
| D) Doxycycline | 100 mg twice daily | Not for use in children <8 yr old |
| E) Trimethoprim–sulfamethoxazole | 160/800 mg (1 DS tab) twice daily | 4 to 5 mg/kg (trimethoprim component) per dose* twice daily |
| F) Penicillin V potassium | 500 mg four times daily | 12.5 mg/kg per dose four times daily |
| G) Cefuroxime | 500 mg twice daily | 10 mg/kg per dose twice daily |
| H) Moxifloxacin | 400 mg once daily | Use with caution in children |
* Child dose should not exceed recommended adult dose.
Adapted from Endom EE: Initial management of animal and human bites. In Danzi DS, editor: UpToDate. Waltham, Mass, 2011, UpToDate.
Whenever possible, even in prehospital settings, wounds should be cleansed and irrigated thoroughly. Irrigation should be delivered with pressure equal to about 8 to 12 psi and debrided as effectively as possible. For some wounds that are not at high risk, attempting field closure is reasonable, and a loose closure with a dressing may help to decrease bleeding, prevent infection and make self-evacuation possible. However, in general, field closure of contaminated bite and claw wounds is not recommended. Further discussion of bandaging and wound-repair techniques may be found in Chapters 21, 22, and 23.
In addition to treating the bite victim, try to capture the offending animal for examination, if this can be done without risk of human injury in the process. Unusual behavior, such as unprovoked attack by a wild animal in broad daylight or a complete absence of fear of humans, should raise the suspicion for rabies (see Chapter 60). Live animal capture is optimal, but freshly killed animals are usually satisfactory for examination for fluorescent rabies antibody. Avoid damaging the animal’s head and brain (e.g., by gunshot or bludgeoning), because brain tissue is needed for analysis. Availability of the animal can eliminate the need for costly and uncomfortable rabies prophylaxis. If more than 1 hour will elapse before the animal can be transported to a hospital or public health department prepared to process the body for the determination of rabies, then refrigerate the body. For shipping, wrap the animal’s head and transport it in an insulated container with ice or ice packs. Do not use preservatives. Be sure to include the type of animal, details of the exposure, date of the animal’s death, victim information, and a description of the animal’s behavior in the report accompanying the specimen.304 An examination of the animal is not useful for most other diseases and will not help predict local wound infections. Therefore, use good judgment when deciding how much time and energy to expend on capture.
Evaluation and Treatment of Injuries: Hospital Care
Resuscitation with fluids and possibly blood products may be needed if there is extensive volume loss. When considering diagnostic imaging, the type of animal and its particular attack characteristics should be considered. Blunt trauma often accompanies penetrating injuries such as goring and trampling. Animal attack wounds classified as high risk for infection (Box 56-7) include deep puncture wounds, moderate or severe wounds with associated crush injury, wounds with areas of underlying venous or lymphatic compromise, wounds on the hands or in close proximity to a bone or joint, and bite wounds in compromised hosts (e.g., immunocompromised, absent spleen or splenic dysfunction, diabetes mellitus). Surgical consultation and hospital admission should be considered early in such cases.
BOX 56-7 Risk Factors for Infection from Animal Bites
High Risk
Location
Wound Management
Animal bites are not clean lacerations, and wounding may be compounded by crush injuries with devitalized tissue. All bites should be treated as contaminated wounds. Evaluate all victims of animal bites for blunt trauma and internal injuries, which may be less obvious than the bite wound (see Box 56-5). Internal organ, deep artery and nerve damage, and penetration of joints are all possible. Particularly in children, animal bites can penetrate vital structures, such as joints or the cranium.53,68 Radiographs may be employed whenever these injuries are suspected. A complete head-to-toe evaluation for trauma is advised in all but the most trivial and isolated bite injuries. Laboratory tests are of little use when evaluating animal bite injuries. Unless hematocrit is being assessed for evidence of blood loss, the complete blood cell count is not useful, because it is a nonspecific and unreliable gauge of infection. Definitive trauma evaluation and treatment are discussed in detail in Chapter 21.
Routine wound cultures obtained at the time of initial wounding do not reliably predict whether infection will develop or, if it does develop, the causative pathogens.135 Therefore, culturing an uninfected bite wound does not yield any useful data.49,60,135 If a bite wound appears infected, cultures and gram staining should be obtained before antibiotics are administered. It is useful to alert the laboratory technician that the culture is from a bite wound, because organisms such as Pasteurella multocida are often misidentified.
Many bite injuries are simple contusions that do not break skin. The infection potential of these injuries is low; superficial wound cleansing and symptomatic treatment of pain and swelling suffice. Treatment should include prompt and liberal application of ice or other cold packs during the first 24 hours. However, this is not beneficial for snakebite (see Chapters 54 and 55), and is obviously impractical in many locations.
When skin is broken, the risks of local wound infection or transmission of systemic disease are incurred. Infection can be caused by organisms carried in the animal’s saliva or nasal secretions, by human skin microbes carried into the wound, or by environmental organisms that enter the wound during or after the attack.225
Debridement removes bacteria, clots, and soil far more effectively than does irrigation.135 In addition, debridement is intended to create cleaner surgical wound edges that are easier to repair, heal faster, and produce a smaller scar. Topical antiseptic ointments (e.g., neomycin, bacitracin, polymyxin) are highly effective for promoting healing of minor skin wounds.146,206 Although topical ointments are appropriate for abrasions produced by animal bites, they may be less effective for punctures and sutured lacerations.
A sutured wound is covered by a simple, sterile, dry dressing to protect it from rubbing against clothing or repetitive minor trauma. Delayed primary closure requires that the wound be kept moist; this is usually done with a wet saline dressing twice daily until closure, which is generally planned for 72 hours after wounding.135
Wound Closure and Infection Risk Factors
Three major considerations govern the decision of whether to suture a wound: cosmetics, function, and risk factors. Cosmetic appearance virtually mandates suturing all facial wounds, which are usually low risk. Similar reasons may dictate closure of wounds on other visible portions of the body. Function is of critical importance for wounds of the hand, a high-risk area in which infection can have disastrous consequences. Thus, in general, all but the least complex hand wounds should initially be left open. Risk factors are many and complex, and provide a useful logical framework for making the decision of whether to suture, administer antibiotics, or undertake other treatments. For more information about surgical procedures, see Chapters 21 and 22.
The amount of time elapsed after wounding is a critical risk factor; the longer the interval, the more likely the chance for infection. After the first few hours, adequate wound cleansing is unlikely to be carried out. In developed countries, many victims are seen within hours of wounding, and the results are usually very good. In remote and undeveloped areas and countries, wounds commonly do not receive medical attention for half a day or more, thereby putting them into a high-risk category that may eliminate the possibility of primary repair. Certain species—including primates, wild cats, pigs, and large wild carnivores—seem to inflict infection-prone wounds. Wounds that involve crush injuries, puncture wounds, hands or feet, or affect a compromised host are at high risk for infection, and primary closure should only be attempted after careful consideration and with surgical consultation and concurrence in most cases. If primary closure is not chosen or deemed too risky, surgical consultation for a discussion of other options, including delayed primary closure or vacuum-assisted closure, is prudent.55,135
Many minimally contaminated bites can be safely sutured after proper wound preparation. Data suggest that carefully selected mammalian bite wounds can be sutured with approximately a 6% rate of infection.84 Two separate studies examining the risk of infection after primary closure reported rates of 7.8% (6 of 92 cases)214 and 5.5% (8 of 145 cases).84 The authors of the latter study concluded that the rate of infection after primary closure was acceptable, particularly if a good cosmetic outcome was needed.84
Bites of the Hand
Because hand bites are common and infection can be disastrous,334 the hand is considered at high risk for complications (see Box 56-7). The hand contains many poorly vascularized structures and tendon sheaths that poorly resist infection. The fascial spaces and tendon sheaths of the hand communicate with each other, and movement seals off the wound from external drainage and spreads bacteria and soil internally. Because of the unique anatomy of the hand, thorough irrigation of wounds is often impossible.
Data regarding hand wound infection have been collected mostly from experience with domestic dog and cat bites. From a retrospective study in Oslo, Norway, it was determined that nearly all hand bite wounds healed uneventfully when the wounds were left open, either without antibiotics or with penicillin after wound treatment.104 In another European center, the total infection rate was 18.8% in hand bite wounds; this rose to 25% when the hand wound was closed primarily. The average time from the injury to the first medical treatment was 11 hours in infected wounds and 2 hours in noninfected ones.7
Because of the high morbidity and permanent residual impairment that occurs with hand infections, treating them aggressively is best (see Box 56-5). Hand bite wounds should be irrigated, debrided if possible, and, in higher-risk wounds, initially left open.135,334 Small, uncomplicated lacerations can be repaired within 12 to 24 hours. The hand should be immobilized with a bulky mitten dressing in an elevated position, and the victim usually should be started promptly on antibiotics. Specialty consultation and follow up are mandatory for persons with established infection, and hospitalization should be considered. Persons who are not hospitalized should be rechecked daily until signs of infection clear. In the patient without initial evidence of infection, 5 days of splinting and oral antibiotics should suffice if no complications develop.62 Radiographic examination to search for fractures and imbedded foreign bodies should be considered for all significantly injured extremities.
Puncture Wounds
Punctures may occur as a result of biting, clawing, or goring. The infection rate is related to difficulty irrigating properly and degree of contamination, which is highest in bites. Puncture wounds can be contaminated with pieces of the victims’ clothing or shoes as well. Usually, attempts to irrigate narrow punctures simply result in rapid development of tissue edema from infused irrigant solution, which does not cleanse the wound. However, if the wound is large or can be held open wide enough to permit fluid to escape, irrigation is worth the effort. Large goring-type puncture wounds up to 20.3 cm to 25.4 cm (8 to 10 inches) deep from bison have a low incidence of infection when closed primarily after irrigation and debridement.96 For most smaller puncture wounds, irrigate or debride them as well as possible, suture only if cosmetic or functional considerations require it, and treat as having a high risk of infection.135 Use delayed primary closure liberally.
Facial and Scalp Wounds
Facial and scalp wounds tend to heal rapidly, with little risk of infection; in general, they may be sutured primarily, and do not require prophylactic antibiotics. Typical dog bites of the face and neck (including punctures) have an infection rate of only 3%, even when sutured.7,104,107,342 Generally the cosmetic closure of facial wounds is afforded by the lower incidence of infection. Standard of care in most cases is primary closure of an animal bite wound of the face.342
A major risk associated with facial and scalp wound victims of large carnivores is that the teeth can easily perforate the cranium, producing depressed skull fracture, brain laceration, intracranial abscess, or meningitis.78,260 In young children with such wounds, or in adult victims of large carnivore bites, computed tomography (or in the absence of computed tomography, skull radiography) should be routinely employed to look for evidence of perforation that would mandate immediate neurosurgical consultation and admission to the hospital.
Follow-Up Care
Assuming that the possibility of major or occult trauma has been ruled out, follow-up care for animal bites depends on the risk factors present (see Box 56-7) and the patient’s response to treatment. With only a superficial abrasion, infection is unlikely, and no return visit is needed. With an ordinary low-risk bite wound, one follow-up visit in 2 days to assess any infection will suffice. If the patient is very reliable and no sutures have been placed, a return visit may not be necessary. Infected wounds dictate much closer follow up, with the frequency depending on the wound’s response to treatment and the patient’s risk factors. In a high-risk wound or compromised patient, the initial follow-up visit should be made within 24 hours if the patient is not hospitalized.
Infection: Zoonoses and Rabies
Immense numbers of bacteria inhabit animals’ mouths and can be inoculated into a bite wound. Claw and scratch wounds may be contaminated with soil, urine, and feces. The exact pathogens vary depending on the biting species (Box 56-8). If inoculated in sufficiently large numbers, these microorganisms can cause localized cellulitis and abscess formation, the most common forms of infection. Wild animals also act as vectors for diseases, such as rabies, cat scratch fever, monkeypox virus, simian herpes virus, tularemia, hantavirus, tetanus, Q fever, and toxoplasmosis (see Chapters 59 and 60).
BOX 56-8
Common Bacteria in Animal Bites
| Dog Bites | Cat Bites | Large Reptiles (e.g., crocodiles, alligators) |
|---|---|---|
| Staphylococcus speciesStreptococcus speciesEikenella speciesPasteurella speciesProteus speciesKlebsiella speciesHaemophilus speciesEnterobacter speciesDF2 or Capnocytophaga canimorsus Bacteroides speciesMoraxella speciesCorynebacterium speciesNeisseria speciesFusobacterium species | Pasteurella speciesActinomyces speciesPropionibacterium speciesBacteroides speciesFusobacterium speciesClostridium speciesWolinella speciesPeptostreptococcus speciesStaphylococcus speciesStreptococcus species | Aeromonas hydrophila Pseudomonas pseudomallei Pseudomonas aeruginosa Proteus speciesEnterococcus speciesClostridium species |
| Herbivore Bites | Swine Bites | Rodent Bites (i.e., rat-bite fever) |
| Actinobacillus lignieresii Actinobacillus suis Pasteurella multocida Pasteurella caballi Staphylococcus hyicus subspecies hyicus | Pasteurella aerogenes Pasteurella multocida Bacteroides speciesProteus speciesActinobacillus suis Streptococcus speciesFlavobacterium speciesMycoplasma species | Streptobacillus moniliformis Spirillum minus |
Data from Garth AP: Animal bites in emergency medicine. http://emedicine.medscape.com/article/768875-overview.
Rabies
Rabies is discussed in detail in Chapter 60, so comments here are limited to brief remarks about epidemiology, assessment of risk in the bite victim, and local wound treatment.
The epidemiology of rabies varies widely in different parts of the world. In the United States, Western Europe, and Canada, wild animals are by far the main vectors of rabies, accounting for more than 88% of all reported cases from the past two decades.196 In India, 95% of rabies postexposure prophylaxis treatment is the result of bites from stray dogs.86 In recent years, rabies in humans has become an extremely rare disease in the United States, with only two cases occurring in 1997196 and one case in 2001.123 Since 1980, rabies-infected bats caused 58% of the human cases of rabies diagnosed in the United States.196 Of the more than 7437 cases of animal rabies reported in the United States in 2001, raccoons accounted for nearly 40% of the total. Foxes, bats, and skunks accounted for all but less than 1% of the remainder. Hawaii is the only state without any reported rabies.123 Foxes are the primary offenders in Europe; some countries have eliminated rabies in wild populations by using innovative vaccination programs.89
Because of local variations in animal vectors and endemics, consultation with the state or local health department is prudent before a decision is made to initiate rabies postexposure prophylaxis (PEP).196 Although the number of human cases has declined, about 18,000 people per year in the United States receive rabies PEP.134 In the rest of the world, virtually all rabies occurs in dogs. Worldwide, dogs account for 91% of all human rabies cases; cats 2%, other domestic animals 3%, bats 2%, foxes 1%, and all other wild animals only 1%.89,347 However, in the United States and Puerto Rico in 2004, 92% of all rabies cases were attributed to wildlife, with the majority being raccoons, skunks, and bats.196 It is important to note that 75% of animal injuries to travelers occurred in rabies-endemic countries, including Thailand, India, Indonesia, China, Nepal, and Vietnam.144 Each year in India, 25,000 humans die from rabies, and one-half million receive rabies vaccine.310 In Thailand, 50% of human rabies cases occur among children who are less than 15 years old.315 In Africa, Latin America, and most of Asia, dogs are the principal vector, although jackals are also a factor. In South America and Mexico, rabid vampire bats cause occasional human infection. During recent years, disruption of the natural ecology of vampire bats as a result of introducing humans and domestic animals to the rain forest has produced epidemics of rabies. In Israel, wolves and jackals are the chief vectors, and the mongoose prevails in Puerto Rico. In Eastern and Central Europe, the raccoon dog (Nyctereutes procyonoides) is an increasingly common vector.89
Thorough and rapid early treatment of wounds from suspected rabid animals may decrease viral load. Immediately cleanse all bite wounds and scratches with soap and water and a virucidal agent (e.g., povidone–iodine solution).302 Evaluate all persons exposed to a possibly rabid animal for rabies PEP. The CDC guidelines issued in 2009 recommend that, for previously unvaccinated persons, the entire dose of rabies immune globulin [20 IU/kg body weight] should be infiltrated at the wound site, if possible. In the United States, two types of rabies vaccine are currently available: human diploid cell vaccine and purified chick embryo cell vaccine. The chosen vaccine is given in 1-mL doses on days 0, 3, 7, and 14 after exposure. Rabies immune globulin should not be administered to previously vaccinated persons. Persons previously vaccinated should instead receive two 1-mL doses of vaccine (either purified chick embryo cell vaccine or human diploid cell vaccine) given on days 0 and 3.74 Further information about rabies pre-exposure prophylaxis and PEP is provided in Chapter 60.
Other Neurotropic Infections
Although Creutzfeldt-Jakob disease (CJD) is not caused by bites or wounds, oral transmission of this spongiform encephalitis has been reported to result from the regionally common practice of eating the brains of wild goats, pigs, or squirrels (even when cooked). CJD is characterized by progressive dementia, ataxia, and myoclonus, and is untreatable. It is caused by a virus also identified in the brains of domestic sheep and mule deer.187 Chronic wasting disease (CWD) is another transmissible spongiform encephalitis that is found in elk and deer in the Four Corners area of the United States (i.e., where Colorado, New Mexico, Arizona, and Utah meet). Food-borne transmission of CJD has raised concerns that the species barrier (i.e., the difficulty an infectious disease encounters during transmission from one species to another as a result of structural protein differences between the agent and host) may not protect against CWD. In vitro conversion of CWD to a human infective form has been demonstrated, but further studies are needed. Between 2001 and 2003, six people—all of whom died—were identified as having a CJD variant. All were known to have consumed venison from CWD-endemic areas, although strong data linking CJD with exposure to CWD were lacking. The risk of transmission to humans, even in CWD endemic areas, remains extremely low.36 Mad cow disease is discussed in Chapter 59.
Indications for Wound Culture
Culture of fresh animal bite wound surfaces, whether judged quantitatively or qualitatively, is useless as a predictor of infection. Some of the pathogens of greatest concern (e.g., genus Eikenella) can take 10 days to grow out in culture, by which time most therapeutic decisions have been made. Other organisms (e.g., genus Pasteurella) are fastidious, hard to identify, and frequently missed by laboratory technicians, who rarely encounter them.150
If a wound is infected or if animal bite sepsis is suspected, obtain wound cultures to guide subsequent antibiotic therapy. In certain cases, cultures should be sent to reference laboratories, such as those in state health departments or at the CDC in Atlanta, Ga, because reference laboratories have successfully isolated more pathogens on identical samples sent simultaneously to both reference and local laboratories.314
Prophylactic Antibiotics
Currently, the weight of evidence does not support use of prophylactic antibiotics for wounds that are not high risk. Many animal bites, human and otherwise, are treated with prophylactic antibiotics, particularly bites to the hands or feet or if the victim is immune suppressed. Human-to-human bites, although outside the scope of this chapter, have similar risks for infection compared with other animal bites. A recent double-blind study of 125 people with superficial human bites showed no statistically significant difference in infection rates between antibiotic and placebo groups.52 A Cochrane Database Systems review of eight randomized controlled trials found no evidence that the use of prophylactic antibiotics is effective for cat or dog bites, except in the case of bites to the hand.225 The use of prophylactic antibiotics is advisable for wounds of the hand; the speed of development, frequency, severity, and complications of hand wound infections can be impressive.135,334 Persons with other risk factors may benefit from prophylactic antibiotics (see Box 56-6). These risk factors include prolonged time from injury to treatment; complex wounds with massive crushing; heavily contaminated wounds; wounds communicating with tendons; fractured bones or joint spaces; or medical conditions such as asplenia, diabetes mellitus, vascular insufficiency, and immune deficiency.
For bite wounds, treatment can begin only after wounding and bacterial inoculation; thus, antibiotics are never truly prophylactic. For major surgery, prophylactic antibiotics are of proved value only in carefully selected high-risk procedures and only if begun before surgery.329 Several controlled studies of dog bite wounds found no significant benefit for using prophylactic antibiotics to treat low-risk facial and scalp wounds.111,206 Other studies recommend the use of prophylactic antibiotics only for high-risk wounds or patients.104,107,155,334,342
To be most effective, prophylactic antibiotics must be administered early. The offending bacteria are already present in the wound when the victim is first seen. Therefore, bite victims who require early antibiotic treatment should be identified promptly, preferably during triage on entry to the treatment facility. The victim should receive immediate antibiotics by protocol; the intravenous route is by far the quickest. The current recommendation for duration of antibiotic prophylaxis is 3 to 5 days (see Box 56-6).
Therapy should be tailored to the largest variety of most likely pathogens for a particular type of bite. For most terrestrial mammals, the choice of antibiotic is based on experience with human, dog, and cat bites. However, with an alligator or crocodile bite, or other wounds incurred in freshwater, antibiotic choice should be directed against Aeromonas hydrophila174,226 (see Chapter 58).
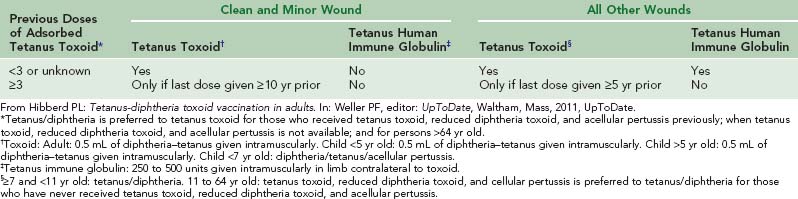
Tetanus Prophylaxis
In the United States, cases of human tetanus from animal bites exceed cases of rabies infection by a ratio of 2 : 1 each year.30 The spores of Clostridium tetani are ubiquitous in soil, on teeth, and in the saliva of animals; therefore, the risk of tetanus may be present from any animal injury that penetrates the skin. Rates of tetanus vaccination are highest in the developed world and fall dramatically in the developing world, with Somalia and Samoa having the lowest rates.346,348 For adults in the United States in 2007, the CDC reported that, out of a sample of 3525 people, 2.1% had received a tetanus booster (tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis) in the past 2 years, and the vaccination rate for tetanus during the prior 10 years was 57% (n = 1727).26,77 Because tetanus is preventable and many persons still do not receive tetanus immunoprophylaxis in accordance with guidelines, proper emergency prophylaxis against tetanus remains an important but often underaccomplished intervention (Table 56-4).
General Complications
Wound infection from animal bites should be treated like infection of any other traumatic wound. Elevate the wound, immobilize the affected part, remove sutures or staples if present, and provide antibiotic therapy (see Box 56-6). The 1999 Emergency Medicine Animal Bite Infection Study Group findings recommended that empiric treatment include a combined β-lactam/β-lactamase inhibitor antibiotic, a second-generation cephalosporin with anaerobic activity, or combination therapy with either penicillin and a first-generation cephalosporin or clindamycin and a fluoroquinolone.135,314 Additional studies recommend azithromycin, trovafloxacin, or telithromycin, which demonstrate good in vitro activity against unusual aerobic and anaerobic animal pathogens.150–152314 In 2002, a study showed that garenoxacin, a des-fluoro(6) quinolone, was very active against 240 aerobic and 180 anaerobic isolates from bite victims. It inhibited 403 of 420 (96%) isolates, including those of Moraxella spp., CDC group EF-4, Eikenella corrodens, all Pasteurella spp., and Bergeyella zoohelcum. Fusobacterium russii and 6 of 11 Fusobacterium nucleatum isolates of animal bite origin were resistant.153
Extremely rare pathogens can cause infection (see Box 56-8). Culture of debrided tissue is the only reliable identification technique, and sensitivity testing may take weeks. In 2002, a 7-year-old girl developed a wound infection as a result of a tiger bite; DNA sequence analysis revealed that one of the causative organisms was a previously undescribed subspecies of Pasteurella multocida, which the authors designated “Pasteurella multocida subspecies tigris.”63 This organism is usually sensitive to ciprofloxacin, cefoxitin, and perhaps rifampin.266 A diabetic patient developed tenosynovitis caused by Mycobacterium kansasii after an accidental bite by his pet dog,305 and Bergeyella zoohelcum has been reported as a fastidious species that is difficult to culture from patients with infected cat bites.294
Septic Complications
Bacteremia and sepsis, although theoretic risks with any animal bite pathogen, have so far been reported with only a limited number of species.9,133,197,260 Clinical manifestations include cellulitis, endocarditis, meningitis, pneumonitis, Waterhouse-Friderichsen syndrome, renal failure, shock, and death. Purpuric lesions are seen in one-third of cases and may progress to symmetric peripheral gangrene and amputation. House cats are an increasing source of human plague in the Southwest United States. Since the onset of the human immunodeficiency virus epidemic, Rochalimaea infection (bacillary angiomatosis) has also become more prominent, and is closely associated with exposure to cats. Although sepsis after an animal bite incident is reported more often among immunosuppressed patients (e.g., there was a case of fatal Pasteurella dagmatis peritonitis and septicemia in a patient with cirrhosis188), there are reports of fatal cases of purpura fulminans with gangrene, sepsis, and meningitis caused by Capnocytophaga canimorsus among previously healthy patients after dog bites. 109,204
Allergic Reactions
Up to 11% of laboratory workers have allergic reactions to laboratory animal dander, hair, or urine.343 One case of proved hypersensitivity to rat saliva after a bite has been reported.157 The patient was subsequently proved to be allergic to the saliva (presumably to saliva proteins) and not to other portions of the rat. The bite produced lymphangitic swelling and itching that subsided within 24 hours. Two cases of anaphylaxis after dwarf hamster bites have also been reported.241
Psychiatric Consequences of Animal Attacks
Victims of traumatic or life-threatening events may develop posttraumatic stress disorder (PTSD). This syndrome has been recognized by the authors as a result of wild animal attack, and is rarely reported in the scientific literature.108 After physical recovery from an attack, the victim may be plagued by recurrent nightmares and flashbacks of the event and may have an aversion to outdoor travel. Violent and multiple attacks or those associated with deep bites have a higher probability of causing PTSD symptoms.262 Critical incident stress debriefing and post-trauma intervention counseling may be important aspects of care for victims of animal attack.108 PTSD has been described among children who are victims of dog bites.262 In a 2004 study, 12 of 27 pediatric patients developed either complete or partial PTSD as a result of dog bites.262
Wild Animal Attacks
Canines
Coyotes
Coyotes (Canis latrans) have not only survived the onslaught of civilization in the United States but have thrived and multiplied. Perhaps as a result, more and more coyote attacks on people have been reported, even in urban areas such as Los Angeles.16,64,177 Most of these incidents occurred in Southern California near a suburban–wildland interface. One study done in 1982 was intended to show the coyote density at such a location. Traps were set for the animals within a one-half mile radius of a particular residence, and 55 coyotes were trapped during an 80-day period.176 Between 2004 and 2007, 541 coyotes were removed on average from Illinois; 312 were from the Chicago area alone. It is estimated that there are 1250 coyotes in the suburban area surrounding Washington, DC.311
Between 1998 and 2003, there were 41 coyote attacks on humans in California, and most were unprovoked; it appears that nonrabid coyotes are becoming more aggressive with humans.79 Rabies is less prevalent among coyotes and foxes with the advent of an oral rabies vaccine for these species.295
Attack incidents are typically preceded by a sequence of increasingly bold coyote behaviors. These may include nighttime coyote attacks on pets; sightings of coyotes in neighborhoods at night; sightings of coyotes during the morning and evening hours; attacks on pets during daylight hours; attacks on pets on leashes; chasing of joggers and bicyclists; and midday sightings of coyotes in the vicinities of children’s playgrounds318 (Figure 56-2, online).

FIGURE 56-2 A hiker at a trailhead bitten on the foot by a coyote while napping.
(Courtesy Luanne Freer, MD.)
Since the 1970s, more than 100 coyote attacks on humans have been recorded in Southern California, with one-half of these incidents involving children who are 10 years old or younger.79 There is one well-documented fatality of a child in 1981, who, despite being rescued by her father, died of blood loss and a broken neck.79 A 5-year-old boy in Middletown, New Jersey (about 64.4 km [40 miles] from New York City) was bitten by a coyote and required 46 stitches to his head.311 A 19-year-old woman was killed by two coyotes (likely coyote–wolf hybrids) in Nova Scotia, Canada while hiking on a trail in October 2009; the woman died of blood loss from multiple bite injuries, and, although one of the animals was wounded, neither coyote was captured.157
The safe environment provided by a wildlife-loving public, which rarely displays aggression toward coyotes, is considered a major contributing factor to the increasing numbers of attacks.79 There has been an increase in reports of coyote attacks in national parks by animals that are subsequently captured and found to be disease free.64
A coyote bite should be treated as a dog bite with respect to antibiotic choice and closure issues; if the animal cannot be captured and examined, rabies prophylaxis should be undertaken. Coyotes have been identified as the reservoir for the human pathogen Bartonella vinsonii sub sp. berkhoffii.80
Wolves
The gray wolf (Canis lupus), also known as the timber wolf, is the largest wild member of the Canidae family (Figure 56-3). There are an estimated 7000 to 11,200 gray wolves in Alaska and more than 5000 in the lower 48 states. Worldwide, the wolf population is estimated at 200,000 in 57 countries.106
Wildlife experts suggest that attacking wolves are habituated to humans and human food sources. However, most unhabituated wolves are traditionally timid. Historically the majority of predatory attacks occurred during the summer months, and victims were predominantly women and children. Predatory attacks by wolves against humans tend to occur in clusters, indicating that human killing is not normal wolf behavior but rather specialized behavior that single wolves or packs develop and maintain until they are killed.335
Throughout Europe and Asia, wolves have well-documented histories of cunning behavior, pack attacks, and human killing.209 In one Indian state, 100 children were injured and 122 killed between 1980 and 1986.274 Between 1840 and 1861, Russia reported 273 nonrabid wolf attacks, resulting in the deaths of 169 children and 7 adults.194 North America has fewer verified cases, although recent research indicates 80 events in Alaska and Canada during which wolves closely approached or attacked people (there were 39 cases of aggression by apparently healthy wolves and 29 cases of fearless behavior by nonaggressive wolves).208,224 Five wolf attacks on humans occurred within a 12-year period in Algonquin Provincial Park in Ontario, Canada, and a kayaker was pulled from his sleeping bag by wolves in British Columbia, Canada.208 In 2005, a hiker in Northern Canada was eaten by wolves, although he likely died of other causes.121,145 Most recently, in March 2010, a woman was killed by wolves in Alaska in what is thought to be the first known fatal attack by wolves in the United States in modern times.235 Villagers in the area had noted increasing aggression from local wolves preceding the attack; wolves are the only large predator in the region, and had been entering the villages at night and frequenting the edges of settlements.
A substantial number of attacks by rabid wolves in Iran over a 10-year period provided the clinical population upon which the human diploid cell vaccine for rabies was tested.24 The reintroduction of wolves to wild habitat in the Yellowstone ecosystem and Idaho in 1995 has resulted in the successful proliferation of many new wolves. However, there has not yet been a negative human interaction since their release.158
Comparison of victims of fatal attacks by domestic dogs and wild wolf packs reveals distinct differences in bite-mark patterns; the necks and faces of domestic dog attack victims were the primary sites of injury, whereas a wolf-pack victim was spared damage to the neck but had facial tissue destroyed postmortem. Most punctures are found on the ventral aspect of victims of domestic canine attacks as opposed to dorsal punctures among victims of wild or feral canines. Wild canine bites involve characteristic crushed and macerated tissue and should be debrided carefully. Other treatment should follow the same guidelines as for victims of domestic canine attack. It is speculated that most wounds are attributable to the dominant animals of a pack. Differences in bite-mark patterns may be attributed to differences in genetics, training, breeding, socialization, and impetus of attack between wolves and dogs.344
Foxes
Most human attacks by foxes are inflicted by rabid animals; fox bites have caused eyelid lacerations among children who are sleeping in tents and leg punctures among adults.195,313,327 One child died of rabies from fox bites despite appropriate PEP.313 A rabid gray fox bit several people during a single afternoon in 2008 in Arizona.14 Foxes can cause more puncture wounds than other canines, making their bites more prone to infection. Oral vaccination of fox populations has led to a decline in the number of rabid animals.295
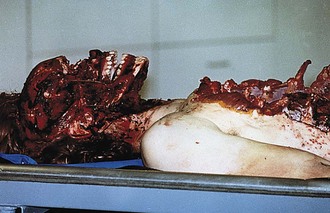
Hyenas
Hyenas have tremendously strong jaws, with a bite force of 1000 psi, and can leave teeth marks in forged steel (Figure 56-4). They have been known to amputate limbs and behead small children.210 The hyena frequently attacks humans in Africa, and, in certain areas in which locals leave dead or dying people in the bush for predators to eat, hyenas become accustomed to the taste of human flesh. Hyenas forage around campsites and villages, and are wary of awake people. During the summer months, when Africans sleep outside of their huts, many are assaulted with one clean, massive bite that removes the face or the entire head. Young children have been dragged from their huts while sleeping when a family member leaves briefly without latching the door, and it is common for the hyena to injure or amputate the thumb of a sleeping victim as it drags the victim (by the thumb) to a more convenient place for consumption.2 Campers are frequently bitten on the face or limbs while they sleep at night, particularly if they have left food nearby. Victims usually survive but are massively disfigured. In some parts of Africa, the hyena is a more consistent maneater than the leopard or lion.
Other Canines
In Australia, during a 5-year period, dingoes that had been habituated to people were responsible for 224 attacks on humans that required medical treatment and for several fatal attacks on children.272 However, dingoes are disappearing from Australia quickly183 and in general pose little threat to humans. Jackals are found in Africa, Southeast Europe, and Asia. Jackal attacks are typically only from rabid animals. In Sri Lanka in 2007, one village reported four different attacks by a jackal that was acting abnormally.281 In many areas of the developing world, the main concern with jackals is transmission of rabies to domestic dogs. Two other canines that traditionally hunt in packs are the cape hunting dog of Africa and the Indian “devil dog.” Although both are feared in their respective environments, typically they do not deliberately attack humans.
Felines
Big cats typically attack from behind and bite the neck and occiput of their prey in an attempt to maneuver their canine teeth between the victim’s cervical vertebrae and into the spinal cord.95,282,333 The goal of rapidly paralyzing the prey is also accomplished by a violent shake of the cat’s head, which fractures the cervical spine. In a study of fatalities from jaguar attack, 77% of victims were bitten on the nape of the neck, and one-half of the bites were made to the base of the skull.95 In 20% of cases, the killing bite was to the head, with at least one canine piercing the skull or ear canal. Cheetahs prefer to attack the throats of their prey, crushing the larynx and strangling the victim; this method is also used by lions and leopards.209 In addition, big cats claw their prey and produce deep, parallel, incised wounds. Several victims have died of exsanguination without evidence of strangulation or cervical spine injury.95,282 Because of the growing propensity for people in developed countries to keep exotic animals as pets or raise them for profit for hunting purposes, injuries by big cats can occur anywhere.
Wound care is the same as for other species, with special attention paid to evaluation for major internal injury. In particular, observe for penetration of deep structures of the cranium and neck, and rule out injuries of the cervical spine and deep cervical vessels (see Box 56-5).95 One victim with an apparently trivial puncture wound after a bite to the neck from a pet cougar was discharged from the emergency department.190 Within hours, her voice was hoarse; on return, she recalled that the cougar had shaken her in its jaws when it bit her, and air was found in the prevertebral and retropharyngeal spaces on radiographic examination.
If a big cat is encountered in the wild, humans should not run but instead stand their ground; running will provoke an instinctive response from the cat to chase. Humans should make themselves look as large as possible, such as by raising arms and jackets over the head. Shouting and acting aggressively may deter an attack. Humans should not turn their backs or crouch when confronted by a big cat. However, as with other large animals, fighting back once an attack has begun may cause a cat to abandon the attack.85
Like domestic cats, big cats usually carry Pasteurella as normal flora. Because of the deep penetration of their large teeth, Pasteurella septic arthritis, meningitis, and other serious deep infections can occur.143 Cat-scratch disease (Bartonella henselae), which is common with domestic cats, may also be transmitted by wild cats; it has been isolated in puma and bobcat populations in the Americas.90
Tigers
Tigers are a major threat to human life in the cats’ native regions.222 Although the number of tigers in the world is dwindling rapidly, historically they have been the number one animal killer of humans (see Table 56-2). Nonetheless, man-killing almost invariably results from stress (e.g., wounds, old age) or lack of natural prey and habitat that forces the animal to prey on humans. A tiger subsisting solely on human meat would have to kill approximately 60 adults per year; documented cases in selected regions have approached this rate over periods of up to 8 years.
Unlike leopards, tigers rarely enter human settlements, preferring to remain on the outskirts. Maneating tigers in India between 1906 and 1941 ate an estimated 125 persons each, and one had killed 436 persons. However, compared with lions, tigers are not thought to become exclusive man-eaters; rather, they are opportunistic man-eaters in lieu of plentiful natural prey, and tiger biologists hypothesize that these animals have become unafraid of man.222
Over the last five centuries, an estimated 1 million people have been eaten by tigers. During the nineteenth century, the tigers’ toll in India averaged 2000 victims per year. From 1930 to 1940, the annual number never dropped below 1300. During the late 1940s, this rate dropped to 800 per year, where it remains. In other regions, rapid habitat loss as a result of climate change has caused an increase in tiger attacks in the Sundarban Islands of Northern India. In this region, seven fisherman were reported to have been killed by tigers during the first half of 2008.125
Adult tigers are so powerful that their human victims are often killed instantly. It is not unusual for a limb to be severed with a single bite,117,205 and a tiger’s swiping blow to the human head can cause skull fracture.270 Like many big cats, tigers typically strike without warning from behind, biting the head and neck and often shaking the head violently so that it severs the victim’s spinal cord.193
Lions
The lion (Panthera leo) is grouped with the four big cats of the genus Panthera (Figure 56-5). Despite their appearance and reputation, lions are not as feared or respected by experienced hunters as are tigers (Figure 56-6). Lions are primarily scavengers, making fewer original kills than hyenas do.
Conversion to maneating has been blamed on drought, famine, and human epidemics in which large numbers of corpses are abandoned in the bush. Although some consideration has been given to the theory that infirm lions are more prone to maneating behavior and although tooth decay may explain some incidents, prey depletion in human-dominated areas is a likelier cause of lion predation on humans.256 In addition, there is an historic predator–prey relationship between Panthera and primate genus members, which suggests that maneating behavior is neither unusual nor aberrant.261 Lion attacks tend to cluster during harvest times and during periods when prey is scarce.254 Wounded or sorely provoked animals, usually in dense brush (Figure 56-7), kill the majority of hunters who succumb to lions.
American and Tanzanian scientists report that maneating behavior in rural areas of Tanzania increased from 1990 to 2005. At least 563 villagers were attacked and many eaten over this period.254 Lions are estimated to eat 300 to 500 Africans per year, and rank second to tigers among man-eaters. During the late 1930s and early 1940s, three generations of a single pride in Tanzania were credited with between 1500 and 2000 human kills. A protected population of 250 Asiatic lions in India has attacked 193 humans, killing 28 between 1977 and 1991; biologists credit drought and lion baiting for tourist shows for this carnage.283
Leopards
Leopards are the smallest of the four big cats in the genus Panthera (Figure 56-8). Like the other big cats, leopards suffer from a loss of habitat and hunting pressure that have reduced their range. Originally inhabiting wild land from Korea through Africa, leopards now exist primarily in sub-Saharan Africa, with isolated pockets across the Asian subcontinent. However, leopard numbers still top all others in the genus Panthera.
Most attacking leopards have been previously wounded or attacked by a dog; when wounded, trapped, or cornered, a leopard is unpredictable and ruthless, attacking the first person within striking distance. Unmolested and in normal health, the leopard is a shy and nervous animal with a marked fear of humans. Unlike a lion or tiger, the leopard relies on fast claw work and biting. Like the jaguar, the leopard may go for the neck (in an effort to sever the spinal cord) or attempt disemboweling by raking at the victim’s abdomen with its claws. The leopard seems inclined to retreat when much resistance is offered; the chance of surviving a leopard attack is higher than the chance of surviving a lion or tiger attack. There is a documented report of a man armed only with a screwdriver who fought and killed an attacking leopard.198,199 Before the era of antibiotics, three-fourths of people mauled by leopards died from wound infection; however, modern morbidity from these attacks is estimated to be less than 10%.25,92
Mauling by leopards is much more common than killing; estimated casualties are 400 per year, mostly in Africa. The leopard does not often turn into a man-eater; when it does, it attacks mainly children or sick adults. In the state of Bihar in India, leopards ate 300 people between 1959 and 1960.92 The maneating leopard of Rudraprayag in India killed 150 people between 1918 and 1926. Becoming increasingly bold, it eventually took its prey by banging down doors, leaping through windows, or clawing its way through the walls of mud huts. The Panar leopard killed more than 400 people after injury by a poacher made it unable to hunt normal prey.169 Like maneating lions, maneating leopards completely change their normal hunting patterns when the prey becomes exclusively human.
Jaguars
The jaguar is last of the four big cats in the genus Panthera and the only one native to the Americas; it is not known to be a man-eater. However, attacks do occur. In February 2007, a zookeeper in the United States was mauled to death by a jaguar.227 In January 2009, a Maryland zoo worker at a private zoo was badly mauled.139 There have also been undocumented reports of jaguar attacks in the jungles of South and Central America.
The jaguar has an exceptionally powerful bite, even relative to other big cats. It employs a variation of the deep throat bite and suffocation technique employed by other Panthera. Using its canine teeth, it pierces directly through the temporal bones of the skull between the ears of its prey, piercing the brain.124
Cougars
The North American cougar (Puma concolor), also called mountain lion or puma, is a clever and shy cat. It is the most widely distributed large animal on the American continent, and the second biggest cat in the Western hemisphere (after the jaguar), although it is more closely related to smaller cats. Cougars are encroaching with increasing frequency into populated areas of the western United States; this is probably because of human expansion into the wilderness and an increased population of protected cougars.192 The current cougar population in Oregon is estimated to be more than 5700,249 and the U.S. population of cougars is estimated at 16,000.321 Humans live, exercise, or picnic in cougar country with increasing frequency.309 Thus, modern suburban dwellers (who are typically ignorant of wild animal behavior) are now in regular close contact with cougars in their homes and parks, whether they know it or not.
In North America between 1890 and 2004, there were 88 confirmed cougar attacks on humans, resulting in 48 nonfatal injuries and 20 human deaths.13 More people have been attacked since 1975 than during the entire previous century,5,21,131 and most attacks occurred in the Western United States and Canada. Throughout the United States, cougars ranked sixteenth in recent years as an animal-related cause of deaths, just behind jellyfish and goats.275 In California, no attacks occurred from 1925 until 1986, when two children were attacked in a regional park in Southern California,190 and the first cougar attack in 34 years occurred in New Mexico in 2008.239
Victims jogging and biking may evoke a predatory response. Young animals that are forced out by adults and must find their own territory are the most frequent attackers of humans,192 and children tend to be the preferred victims: 64% of attacks and 86% of fatalities involve children.35,182,186 There has been only one alleged report of a cougar as a primary man-eater, but cougars commonly consume victims of their attacks (Figure 56-9).32,282
The cougar hunts like a domestic cat: crouching, slinking, sprinting, pouncing, and then breaking the neck of the prey. Neck, head, and spinal injuries are common and sometimes fatal. Like many potentially dangerous wild animals, the cougar can often be scared off by the victim’s aggressive behavior, even after the attack has begun.170 In 2002, a man fought off and killed an attacking cougar with a 7.5-cm (3-inch) pocketknife.328
Bobcats
Although it is unusual, bobcats occasionally attack humans. In most cases, the bobcat is rabid and unusually aggressive. In 2000, a Minnesota woman reported suffering puncture wounds to her hand and arm that were consistent with the bites of a bobcat. Another woman was the victim of a witnessed bobcat attack in Big Bend National Park.44 In this case, although experts believed that the animal was behaving normally, the victim was empirically treated for rabies exposure. A hunter sustained injury to the eye and ocular adnexa requiring surgical repair after a bobcat attack.173 Two people were attacked by a rabid bobcat in 2008 in Arizona while hiking in the mountains, suffering puncture wounds and scratches; the bobcat was described as unusually aggressive, and pursued the couple up a hill.132 A man in Florida reported being attacked by a rabid bobcat on his front porch, where he was clawed and bitten until he managed to strangle the animal.215
Primates
The Primates order is divided into two main groups: the prosimians, which have characteristics most like those of the earliest primates, and the simians, which is comprised of monkeys and apes. Simians are further divided into the New World monkeys of South and Central America and the Old World monkeys of Africa and Southeastern Asia (Figures 56-10 and 56-11; Figure 56-11, online).
Monkeys and other primates inflict vicious bites that virtually always become infected, despite use of prophylactic antibiotics.154 Although in developed countries human–primate conflict is a problem limited to laboratory workers, in tropical developing countries, large apes (e.g., baboons) are both at large and often aggressive. Weighing up to 40.8 kg (90 lbs), a large baboon can be dangerous and lethal, particularly when the animal has frequent contact with humans and loses fear of them. There are multiple reports of baboon attacks in South Africa against visitors, typically when the baboon is foraging for food.61 There have been numerous recent reports of packs of wild monkeys driven out of the jungle by hunger, attacking humans who get in the way of food sources.278,285,307 Feral macaque populations have been reported in regions of Texas and Florida.252
Monkeys often bite hands and have been known to amputate parts of fingers. A literature review revealed 132 cases of simian bites in which Bacteroides, Fusobacterium species, and Eikenella corrodens were isolated from some of the wounds.154 Three victims of simian bites with infected wounds grew diverse bacteria, including β-hemolytic streptococci, enterococci, Staphylococcus epidermidis, and Enterobacteriaceae.154 At the present time, simian bites should be considered high risk and treated in the same manner as human bites.
Old World macaque monkeys (i.e., rhesus macaque, cynomolgus, and other Asiatic macaque monkeys) are often infected with simian herpes virus (B virus). Transmission to humans is rare, but the risk is real, especially for animal control and laboratory workers.114,240 As with rabies, local wound treatment may be important; of 61 persons bitten by probably infectious monkeys who received wound cleansing with cetrimide and iodine solution, none became infected.320 The mortality rate for B virus is 80% without treatment; through 2002, there were 26 documented cases of B virus infection in humans and 16 deaths. Twenty of the victims developed some degree of encephalitis. The most recently documented case occurred in 2008 and involved a woman who was bitten by a vervet monkey in the Democratic Republic of the Congo in Africa (see Chapter 59).244,331
The wild gorilla, despite its reputation and appearance, is shy and avoids humans. Although it may charge in defense, it seldom attacks, and can be easily confronted and forced to retreat. When a gorilla attacks, it typically takes one bite and runs. In Africa, gorillas are responsible for two or three attacks per year, none of which is fatal, and few of which are severe. Chimpanzees occasionally attack humans, but usually only if provoked or cornered. Rare instances of chimpanzees eating children and women have been reported. The baboon is responsible for one to two attacks per year, almost all in South Africa; these are usually by pets. Occasionally, maneating has been reported. The incidence of hunting and meat eating by these animals has increased over the last century, perhaps paralleling the evolution of humans into hunters and meat eaters.92
Herbivores and Ungulates
Wild Swine
Wild pigs are more likely to inflict injury than their domestic counterparts. With a population of over one-half million roaming the French countryside, wild pigs cause crop loss and occasionally gore and bite humans.213 A typical wild boar attack can result in multiple penetrating injuries to the lower part of the body caused by the boar’s tusks (Figure 56-12, online). In an unusual incident, an Indian laborer was gored from behind by a boar, which then returned and attacked his head while he was on the ground; the man died of severe craniofacial injuries.216,292
Domestic pigs can easily become feral, and such populations often revert to the behavior and appearance of a wild boar. In the United States, feral pigs—some weighing up to 181.4 kg (400 lbs) with 10.2-cm (4-inch) tusks and prolific breeding qualities (i.e., some litters of up to 19 have been reported)—are experiencing explosive population growth. More than 1.5 million wild swine roam the state of Texas, and motor vehicle collisions as well as attacks on humans are increasing.54 As of 2008, it was estimated that the population of 4 million feral hogs caused approximately $800 million worth of property damage per year in the United States.51 Swine wounds should be treated as high risk for development of infection, warranting broad-spectrum prophylactic antibiotics (perhaps parenterally) and close follow up if the victim is not admitted to a hospital.
African Buffalo
Known as one of the “big five” (i.e., the five most difficult African animals to hunt on foot: buffalo, lion, elephant, black rhino and leopard), African buffalo (Syncerus caffer) gore and kill more than 200 people each year. The unprovoked African buffalo usually does not attack. However, when provoked (i.e., shot or cornered), it charges, is difficult to avoid or stop, and can hook the victim 3 m (10 feet) into the air with its horns (Figure 56-13). Buffalo that charge humans are usually old solitary bulls that have left the safety of the large herds, most often because of wounds from poachers’ snares or spears, or from lion attacks. The buffalo is also wily and intelligent; wounded buffalo may lie in wait for trackers, or may double around and come up behind hunters on the trail, often with fatal consequences for the humans (Figure 56-14, online). One hunter was treed by a buffalo but could not get his feet high enough to keep them clear of the animal; the buffalo repeatedly hooked the man’s feet with his horns, eventually cutting them so that the hunter bled to death while still hanging in the tree. In another anecdotal series, a single buffalo injured several humans in one day; all of the wounds were impaling injuries through the anus.2
When the victim is prostrate, the buffalo gores into the ground with its horns and the heavy horny boss across its forehead and then whips its head from side to side, disemboweling the victim with the sharp horn tips. The horns are always covered with mud, so goring wounds may be heavily contaminated. However, victims who do not have major traumatic injuries generally do well.291
Water buffalo were once a common wild animal on the Indian subcontinent and in Southeast Asia, but are primarily domesticated work animals in these regions today. Domesticated animals pose little threat to humans, but are still capable of attack if provoked. A water buffalo attacked and gored a man to death in Australia in 2005, the first recorded death from a water buffalo in 12 years in that country.317 The buffalo had been acting strangely for several weeks, charging people and entering towns, and was thought to be stressed because of drought in the region.
American Bison
Brought back from the brink of extinction, a free-ranging herd of North American bison (Bison bison) with a fluctuating population of 2300 to 4500 now lives on land in and around Yellowstone National Park and is responsible for an average of three tourist injuries per year.237 Fifty-six injuries and three deaths were documented from 1975 to 1993 in Yellowstone as a result of bison–human interaction.97 Despite warnings to avoid approaching these animals any closer than 7.6 m (25 feet), most attacks involve close human approaches to obtain photographs. The mechanism of injury in bison attack is usually penetrating injury, with punctures from goring by horns and blunt injury caused by being tossed in the air and falling or being butted by the animal’s massive head (Figure 56-15). Goring injuries most frequently involve the buttocks or posterior thighs as the victim turns away from the bison to flee (Figure 56-16).97 Gored abdomens and evisceration have also been reported. Despite the inevitable contamination of these deep punctures, wound infection is rare if careful operative irrigation and debridement with closure are combined with broad-spectrum prophylactic antibiotics. Cephalosporins were used in most cases in one series of reported injuries.97
Elephants
The elephant (Proboscidea elephantidae) can be one of the most dangerous wild animals and was, until recently, probably the greatest killer of hunters. It is the largest land animal (Figure 56-17), and there are three living species: African forest, African bush, and Asian (Elephas maximus). The annual human death toll related to these animals in Central Africa is probably between 200 and 500.92 Most injuries occur when humans accidentally approach elephants too closely, which the animals interpret as a threat. However, elephants turn rogue from time to time and deliberately attack and kill humans (Figure 56-18, online). As humans and elephants compete for the same space and humans despoil and devastate forests, conflicts increase (Figure 56-19, online).
A few rare stories suggest that elephants may actually be man-eaters. One of these instances occurred in 1944 at the Zurich Zoo. Elephants that are captive in zoos and circuses may cause deaths while temporarily deranged. Since 1990, captive elephants have killed 39 humans and injured more than 100 worldwide.259 In 2007, a domesticated elephant in Vietnam gored his two handlers to death after they forced him to work without eating.171
Some experts theorize that elephants are capable of vindictive motivation for attack.179,296 In Africa, groups of young elephants have attacked villages in what is thought to be revenge for the destruction of their society by massive hunting done during the 1970s and 1980s.172
India is home to most of the world’s 40,000 Indian elephants (sub sp. Elephas maximus indicus), which reside throughout the subcontinent. In the Indian state of Jharkhand, 300 people were killed by elephants between 2000 and 2004, and, in Assam, 239 people have been killed since 2001.179,296 Elephants kill about 50 people each year in Sri Lanka. Such encounters force some families to sleep in trees, and elephants in one area with a human population of only 25,000 kill at least four people a year.18 In 2004, 22 people were killed in Assam by rogue elephants that repeatedly trampled homes and ate local crops. Reportedly, the elephants were also seeking rice beer, for which they had developed a taste.17 Elephant attacks have become so common that a new statistical category known as human–elephant conflict has been created by elephant researchers.296
Elephants kill by trampling, goring with the tusks, or striking and throwing with the trunk. After the victim has been run over or skewered with the tusks, the elephant then crushes him or her by kneeling (Figure 56-20). Elephants have been known to use weapons during their attacks: a villager who retreated safely up a baobab tree was hit by a tree branch that a bull elephant had picked up in its trunk and used as a club. Elephants frequently rip the victim’s body apart and scatter the pieces, later covering them with grass and branches. Another elephant tactic is to toss a victim into the trees or straight over his or her back; a number of victims have survived this experience. Some hunters pursued by elephants have diverted them by throwing off items of clothing.
Hippopotami
The hippopotamus (Hippopotamus amphibius) is a frequent killer in Africa (Figure 56-21). Its placid appearance in zoos belies its activity and personality in the wild; they are ill tempered at best, and have been known to attack crocodiles. A hippopotamus can run at speeds of up to 72.4 km/hr (45 mph) on land. It will attack boats and people in the water if it feels trapped (e.g., between a boat and deep water) or if its calf is threatened. Hippopotami graze on land and habitually run along established narrow tracks back to the river, mostly at night but also in the day. They are not known to change course when challenged, and humans who make the mistake of staying in their tracks may be trampled. With its large canine teeth, a hippopotamus can chop canoes (and the people in them) in half, as it does several times a year on the Zambezi River in Zimbabwe. Surviving a hippopotamus attack is uncommon. Injuries are typically very extensive and can include significant crush injuries to internal organs and other tissues as well as long bone fractures.120,207,265
Moose and Elk
Moose (Alces alces) are large and potentially aggressive animals, especially during fall rutting and spring calving seasons. When moose are fed by humans, they become more aggressive when food is no longer available.8 Moose consider dogs predatory and will attack and kill them without other obvious provocation. If the rump hairs are raised, ears laid back, or the moose is licking its lips, it is likely to charge. The subject of the attack should get behind a large solid object for protection. If knocked to the ground by a moose, a victim should roll into a ball, protecting his or her head with the hands and arms, and remaining still until the moose leaves.8 In 1995, a man was killed by a moose in urban Alaska when he approached a cow with a calf who had been harassed by students throwing snowballs.238
Most human injuries caused by moose result from moose-related motor vehicle collisions, which are quite hazardous in New England and Sweden.46,129 In a New England report, it was stated that an average of two persons per year are seriously injured when their vehicle strikes a moose, usually after dark; 70% of those injured have head and facial injuries, and 26% have cervical spine injuries.129 The mortality rate in this series was 9%, and morbidity declined with the use of seat belts and rear seat location. Each year in British Columbia, it is estimated that three people are killed and an additional 368 injured in wildlife collisions (i.e., deer, moose, and elk); 17,200 animals are killed by these collisions as well312 (Figure 56-22).
Similar to moose, bull elk may attack humans during rutting season, and cows may attack by butting and stomping when protecting their young.257 A study done in Michigan from 2002 to 2005 showed a less than 1% prevalence of Mycobacterium bovis in elk.245 Elk can also be carriers of Brucella abortus, which can be transmitted through direct contact with infected animals.279
Deer
The deer population continues to grow in parts of the United States. As a reservoir of the tick that are vectors, deer may be credited with the increasing incidence of human Lyme disease.232 Block Island, a 17.7-km2 (11-mile2) island off of Rhode Island, reintroduced one buck and four does to its area in 1968, and had a herd of more than 1000 animals and 45 recorded cases of Lyme disease among residents as of 1997.232 Residents also report having been attacked by deer in their own yards.
Deer rarely attack humans, but deer–motor vehicle collisions are quite common in densely populated areas. About 1.5 million deer–vehicle collisions happen each year in the United States, according to the National Highway Traffic Safety Administration93; those accidents cause about 150 deaths and $1.1 billion in property damage. More than 21,000 collisions occurred in Finland in one year, with the majority of events occurring during the first hour after sunset.164 One deer jumped through a window of a law office and injured an attorney,20 and another buck in rut carried a man in its antlers for 45 minutes, then pinned the man on the ground until he was rescued.39 A startled buck gored a child when the boy was feeding the animal; the antler penetrated the child’s axilla, lacerated his pulmonary artery, and caused death by exsanguination.128 Deer may bite, and, like other ungulates, may carry Pasteurella as oral flora. Female deer bite other deer when fighting. Males bite when testosterone levels are low; at these times, antlers are soft and pain sensitive, and cannot be used as weapons. Foreleg kicks are more common, because the deer stands on its back legs. Because deer have a dental pad rather than upper incisors, bites are rarely serious and are usually directed at the arms or back, which are normally well covered by clothing. These bites are usually single nips.
Rhinoceri
The black rhinoceros has been represented as one of the meanest animals in Africa because it charges any moving object, including trains. A click of a camera, gentle movement, or scent is enough to induce a charge. Because the rhinoceros has poor eyesight but excellent hearing, it may well be running toward sounds to investigate them. Contrary to the popular belief that because of its nearsightedness it can be easily sidestepped, the rhinoceros can turn on a dime.91 At the end of its charge, it usually hooks right and left with its horns, and is generally satisfied with tossing the victim high (i.e., 3.7 m [12 feet]) in the air. However, like so many large wild animals, it probably does not desire confrontation. Rhinoceri often flee after they have identified a sound as originating from something dangerous (e.g., a human), and persons who have fallen while running from a charge have been investigated with a few typical snorts and then ignored. However, severe injuries can result if the human fails to get out of the way of a rhinoceros. Black rhinoceri in Africa kill a handful of people each year.120 As with the hippopotamus, injuries and death may have more to do with being in the path of a very large and fast-moving object than with the animal’s malicious intent. The white rhinoceros is typically docile; its attacks on humans are extremely rare.
Tapirs
The tapir (Tapirus terrestris) lives in the rainforests of South America, Central America, and Mexico. The female reaches a length of up to 2 m (6.6 feet) and a height of up to 1 m (3.3 feet), and weighs up to 200 kg (441 lbs). Tapirs are herbivorous and generally docile. They seek refuge in brush when threatened or submerge themselves in water until the threat is gone; however, they may defend themselves by biting with their powerful jaws and teeth. A tapir bit off the arm of a zookeeper in 1998 who came between the usually docile animal and its calf,114,180 and a man died of exsanguination from arm and neck lacerations after a tapir attack in Brazil.163,338 The Environmental Minister of Costa Rica sustained a tapir bite in Corcovado National Park in 2006; this attack also involved a female defending its calf.276
Other Wild Herbivores
Other wild species, such as the giraffe, may turn rogue, but this is exceedingly rare. The black wildebeest has killed one or two zookeepers, as have the spiral-horned kudo and bushbuck. Other antelopes have killed or wounded hunters or zookeepers with their sharp horns. Zebras are known to bite tourists who approach too closely.319
Bears
Bears are among the most feared and powerful predators on Earth, yet the incidence of bear attacks on humans is small compared with other animals discussed in this chapter. However, the scientific literature about bear behavior and human interactions is more plentiful than that about, for example, tiger or alligator attacks. Chapter 57 is devoted to a discussion on bear attacks (Figure 56-23, online).
Kangaroo
Kangaroos (family Macropodidae) are the largest living marsupials in the world, weighing up to 79.4 kg (175 lbs). They use their tails for balance when they jump, and can leap almost 9.1 m (30 feet) forward and 2.4 m (8 feet) high. They are active in the evening and at night, when groups of kangaroos, called mobs, forage on grasses and other plants. A university study from New South Wales reported that kangaroos account for 60% of all animal-related automobile crashes in Australia resulting in fatalities and for 40% of automobile–animal accidents resulting in injuries.224 From 1996 to 2006, there were 2100 kangaroo–vehicle collisions and 13 human deaths from kangaroo–vehicle incidents. In remote areas of Australia, the odds of hitting a kangaroo are so high that residents fit their vehicles with “roo bars” to deflect kangaroos off of the front of the vehicle.4
In 2004, there were several unprovoked kangaroo attacks in Australia, which led to speculation about a rabies-like disease affecting marsupials; however, there is no published evidence to support this theory. The only well-documented kangaroo attack resulting in a fatality was in 1936, when a hunter was killed trying to separate his dogs from a fight with a kangaroo. Erratic kangaroo behavior may also result from extreme thirst and hunger.336 Kangaroos attack using a combination of kicking and trampling with their powerful hind legs. They are also capable of delivering slashing wounds with their feet.
Large Birds
Ostriches (Struthio camelus) are responsible for one to two deaths per year, mostly in Africa, where they are raised commercially19 (Figure 56-24, online). Most of the fatal attacks involve kicks to the head and abdomen. Disembowelment, eye injuries, and esophageal perforations have all been reported.83,189,234 The ostrich (Figure 56-25) can kick only forward, but when it does, a sharp toenail flicks out like a switchblade and can penetrate the abdomen. Because the ostrich can easily outrun a human being, the only protection is to lie prone to protect against disembowelment and to cover the neck to protect against pecks. Eventually, the ostrich loses interest and allows the victim to escape.
The cassowary, which is common in New Guinea, can easily disembowel a hunter with a single kick from its long, sharp toe claws. Birds of paradise have been found to secrete venom on their feathers, although cases of human toxicity from this have not been reported and the phenomenon is little studied. The emu is a flightless bird native to Australia that may weigh 45.4 to 68 kg (100 to 150 lbs). It is usually docile, but when cornered or frightened may lacerate a human handler by kicking.185
Raccoons
Raccoons (Procyon lotor) are medium-sized animals native to North America that adapt well to a wide range of changing habitats. The raccoon is at home as much in urban settings as in deciduous forest ranges, and can be found across the United States. A population was established as a game animal in Germany during the mid-20th century, and is now well established in several northern European countries.337 As raccoons expand their range to include urban settings, conflict with humans will increase. Raccoons are on occasion kept as pets. In 2009, a young boy was bitten by an immature raccoon housed in a box.217 Raccoons tend to be opportunistic hunters, and keeping food and garbage cleaned up and stored properly can eliminate potential encounters.
Of the 6940 documented animal rabies cases reported in the United States in 2006, 2615 (37.7%) were in raccoons,47 which represents the highest carrier rate for rabies.196 In the United States, large raccoon rabies epizootics in New England and the middle Atlantic states are spreading, and most rabies-positive animals are captured near private homes.298,340 In 2003, raccoon variant rabies caused a human death in the United States, although the route of transmission was unclear, because there was no bite.70 Because rabies is so common in raccoons, rabies PEP should be strongly considered for victims of attack or unusual close contact. Some other important diseases associated with raccoons are leptospirosis, listeriosis, tetanus, and tularemia.212 Raccoons are the definitive host of Baylisascaris procyonis, a zoonotic nematode parasite that may cause larva migrans syndromes in humans.353
Porcupines
Porcupines are a member of the order Rodentia, further divided into New World species (12 identified) and Old World species (11 identified). They are rarely reported to bite, but their quills may become embedded in the skin of humans. Quills are released on contact, or can be dropped out when the porcupine shakes its body, but cannot be projected at attackers. Because of the structure of quills, they not only embed themselves and are extremely difficult to extract, but can migrate as much as 25.4 cm (10 inches) under the skin. The average porcupine has 30,000 quills, which range from less than 2.5 cm (1 inch) to 10.2 cm (4 inches) in length. The quills are barbed, and their cores are spongy; if they are not removed from a “quilled” victim immediately, they absorb body fluid and expand, causing them to flare farther outward. Thus, each movement of the victim’s muscles or body helps a quill embed deeper. Anecdotally, such migration has led to internal organ damage and death in humans. Quilled dogs have suffered a variety of illnesses, including brain penetration as a result of migration105 (Figure 56-26). Infection seldom results, because quills have mild antiseptic properties, presumably to protect the porcupines, which sometimes impale themselves.
No medical reports of appropriate human treatment or complications of porcupine quill injuries exist, although anecdotal reports of human tetanus from porcupine quill puncture have come from Africa.2 Most veterinarians remove quills from animals by simple extraction; the same technique is probably sufficient in humans after local anesthesia and disinfection of the skin.
Coatis
The ring-tailed coati, Nasua nasua, is widely distributed in the Americas. It is a social animal whose omnivorous diet includes insects, fruits, and small vertebrates. There is only one published report in the medical literature describing coati attack; two children in their home were injured by a startled coati, causing skin lesions from deep scratches and bites45 (Figures 56-27 and 56-28).
Quokkas
The quokka is one of the smallest members of the wallaby family, which resides in Western Australia. The quokka typically only bites humans who attempt to feed or pet it. Bites usually occur on the finger or hand. On Rottnest Island, Australia, quokka have been known to steal food after breaking into homes. The island’s infirmary reported 60 quokka bites in 2006.119 Despite the presence of mixed coliform bacteria in quokka mouth cultures, the incidence of bite-wound infection in this series was zero.221
Opossums
The American opossum (Didelphis virginiana) is a non-native species that has adapted to urban living and presents difficulties for animal control agencies. It inflicts bite injuries both when hunted for food and when accidentally provoked while handled in captivity. Opossums compromise a major reservoir of endemic typhus in Los Angeles County in California.101
Aerobically cultured organisms from the mouths of seven wild opossums included streptococci, coagulase-positive and coagulase-negative staphylococci, Aeromonas species, Citrobacter freundii, Eikenella corrodens, and Escherichia coli.175
Skunks
Skunks are small mammals belonging to the family Mephitidae, order Carnivora. They are capable of secreting a strong, foul-smelling odor. A skunk’s most frequent means of defense is spraying the secretions of its anal sac. A skunk that is ready to spray directs its hindquarters toward the enemy, with its feet firmly planted and tail straight in the air, often stamping the front feet in warning. The spray is accurate to 4 m (13 feet), and, contrary to popular belief, can be discharged when the animal is lifted by its tail.113,339
Skunk musk causes skin irritation, keratoconjunctivitis, temporary blindness, nausea, and occasionally convulsions and loss of consciousness.137 The chief component of the musk is butyl mercaptan; this can be neutralized by strong oxidizing agents, such as sodium hypochlorite in a 5.25% solution (household bleach) further diluted 1 : 5 or 1 : 10 in water. The chlorine forms odorless sulfate or sulfone compounds by oxidizing the mercaptan and breaking the sulfur free from the carbon chain. This solution can be cleansed with tincture of green soap and followed by a dilute bleach rinse. Other effective means of eliminating skunk odor include Summer’s Eve Douche or a mixture of 1 quart of 3% hydrogen peroxide, 0.25 cup of baking soda, and 1 teaspoon of liquid soap. Tomato juice is not an effective means of removing skunk odor.
The CDC recorded 1494 cases of rabies in skunks in the United States in 2006; this was 21.5% of reported cases in all species.47,73 Skunks bite readily when captured, but, in one series, only 21 bites were reported for the entire United States for a 10-year period.110
Bats
Bats are mammals in the order Chiroptera. There are about 1100 species worldwide, which comprises 20% of all classified mammal species.345 Bats carry a large number of zoonotic pathogens, including rabies, severe acute respiratory syndrome, and possibly Ebola viruses.148 Less than 1% of all bats carry rabies. However, the few cases of rabies reported in the United States each year not caused by dogs are usually caused by bats.220 Bats infected with rabies are clumsy and have difficulty flying, making it more likely they will come into contact with humans.
Vampire bats are a vector of rabies in Central and South America; 177 cases were reported from 1980 to 1990, with 27 of these cases in Brazil.30 Sometimes small “epidemics” of bites occur in isolated villages in the jungle, as in one outbreak of 26 bat bites in Honoropois, Brazil; all victims were treated with rabies prophylaxis, and no clinical human rabies was reported.30 In 2004, a rabies outbreak from vampire bats occurred in Columbia, resulting in 14 human deaths.324 Such clusters of attacks may be triggered by human destruction of wild or domestic hosts of the bats (e.g., pigs).219 Vampire bats feed at night on animal blood, including that of humans, by making an incision in the skin to lap up the blood from the victims’ earlobes, forehead, fingers, or toes. One bat can eat a maximum of 1 oz of blood per night. A cave of 1000 bats needs 15 gallons of blood each night, which amounts to more than 5750 gallons per year.91 Protection against vampire bats is effectively achieved with the use of mosquito nets.
Insectivorous bats (e.g., free-tailed bats) are noteworthy for the nearly undetectable bite wounds that they leave on their victims.147 All bats should be considered high risk for rabies, and contact, even with captive “pet” bats, should be avoided. The known pathogenesis of rabies and available data suggest that nearly all cases of human rabies attributable to bats were transmitted by bat bites that were minimized or unrecognized by the victims. Non-bite transmission of rabies is very rare, and aerosol transmission has never been well documented in the natural environment.147 Some situations mandating rabies prophylaxis are rather bizarre and reveal more about human nature than about rabies or bats. For example, rabies prophylaxis was initiated after a patient dunked a dead bat in his beer, chewed on the bat’s ear, and then drank the beer.115 In a similar case, prophylaxis was needed when a miner swallowed a live bat on a bet.42 Most bats have small teeth that cannot penetrate human skin, so the risk of bacterial wound infection is low.
Venomous Mammals
Only two types of venomous mammals are known. The short-tailed shrew (Blarina brevicauda) of the northeastern United States secretes a protein venom from its maxillary venom glands and injects it with the lower incisors. The venom may cause edema, a few days of burning sensation, and pain that lasts up to 2 weeks.78 No specific antivenin is available, and treatment is symptomatic. No bites from this species have been reported since the 1930s. A similar venom is possessed by the European water shrew (Neomys fidiens) and the primitive Cuban insectivore (Solenodon paradoxus).56 Documented bites from these animals are exceedingly rare.
A second type of venomous mammal is the male platypus (Ornithorhynchus anatinus), which injects venom from a hollow spur in its hind leg. This venom resembles viperine snake venom and causes local pain, edema, and lymphangitis.56 The pain can be excruciating and unresponsive to intravenous narcotics. Regional nerve block has been reported to be effective in combination with limb immobilization.131 Localized edema also occurs; however, no specific treatment is available, and the exact pathophysiology is unknown. Functional recovery may be delayed for up to 3 months. The echidna or spiny anteater possesses a similar spur and venom, but envenomation has not been reported.137
Large Reptiles (See Chapters 54 and 55)
Historically, the Nile crocodile (Crocodylus niloticus) has accounted for 1000 human deaths per year in Africa91 (Figure 56-29, online). Most attacks take place in the water, where crocodiles are accustomed to scavenging for dead, sick, and deformed human infants tossed into the water to be disposed of by these reptiles. The crocodile has tremendous grip strength and locks this grip by slotting two lower teeth into holes in the upper jaw. When a crocodile is unable to drag the victim completely underwater, it may grasp a limb and then spin over until the limb is detached.
During a 10-year period in Australia, there were 16 attacks and 4 fatalities caused by crocodiles; most victims were swimming or wading at night, and alcohol ingestion was present in one-half of them.226 Wound infections with Aeromonas hydrophila, Pseudomonas pseudomallei, and Proteus, Enterococcus, and Clostridium spp. were reported in 6 of 11 survivors in this series.226 In Malawi, over a period of 4 years, 60 victims were admitted to hospitals after injury by crocodiles; 40% had serious injuries resulting in permanent deformity, and one person died from sepsis.326
The American alligator (Alligator mississippiensis) is thriving in the southern United States, and its habitat is so greatly threatened by human expansion that incidents of alligators appearing in suburban backyards and swimming pools are now common (Figure 56-30). Attacks on children and pets are increasing, with 127 attacks and five deaths reported in Florida from 1973 to 1990.174 Between 2001 and 2007, there were 13 alligator-caused deaths in the United States (mostly in Florida). All of the attacks involved some level of predation.136 The alligator causes crushing injuries to the torso and open extremity fractures, and may roll underwater with the victim, resulting in drowning. Blunt trauma may result from a strike by the animal’s massive tail. Prevention of alligator attacks includes avoiding touching or feeding the animal and not swimming at feeding time (dusk) with a dog or in waters with heavy vegetation.97
Komodo dragons (Varanus komodoensis), native to Indonesia, have also suffered from habitat and prey depletion. Members of the monitor lizard family, Komodo dragons have sharp teeth built for tearing and a venomous bite containing several different toxic proteins. Their bite is not designed for crushing; in fact, its force is similar to that of a house cat.29 The venom causes inhibition of blood clotting, paralysis, and hypotension leading to shock and loss of consciousness in bitten prey.6,141 With the discovery of venom action, the previous assumption that bacteria found in the dragon’s saliva and teeth cause death has been disproved. However, the saliva of the dragon, given its primary food source of carrion, predisposes its bite to contain diverse bacteria, including Escherichia coli, Staphylococcus sp., Providencia spp., Proteus morgani, and Proteus mirabilis.229 Up to 57 different strains of bacteria have been identified in a Komodo dragon’s saliva, including resistant strains of four usually susceptible pathogens.229 Probably because they are fed a cleaner diet, captive animals have cleaner mouths. Komodo dragons are apex predators that hunt game using stealth, ambush, and a keen sense of smell.
Komodo dragon attacks on humans are rare, but have been increasing over the past decade. Reports of dragon-related injuries and deaths date back to the 1940s, and five people have been killed by dragons since 1974. The animals are considered especially dangerous to children. In 2007, a Komodo dragon attacked an 8-year-old boy on Komodo Island; the boy died of massive bleeding.22 Locals blamed the attack on the suspension of goat sacrifices, claiming that the hungry dragons wandered into settlements in search of food. In 2009, two Komodo dragons killed a fisherman after he fell out of a tree and was then left bleeding badly from bites to his hands, body, legs, and neck.5 A well-publicized incident involving a publisher occurred in 2001 at the Los Angeles Zoo in California, when the man was invited into a Komodo dragon exhibit and was bitten on the foot.31
Marine Mammals
Marine mammals account for about 120 different species of animals and include cetaceans (whales, dolphins), sirenians (manatees), pinnipeds (true seals and walruses), and mustelidaens (otters). Polar bears (see Chapter 57) are sometimes considered marine mammals as well, because they spend most of their lives on pack ice; however, this section only considers seals, walruses, and otters.
One survey revealed that 54% of workers in contact with marine mammals reported experiencing at least one injury or illness (mostly cuts, scrapes, bites, and rashes).323 Eleven percent reported developing seal finger, which is discussed later in this chapter. Injury occurred in 52% of these individuals while they were handling the animals or animal tissue. Of these injuries, 36% were severe and included deep wounds and fractures. In another survey of 483 marine mammal workers, 50% suffered an injury caused by a marine mammal, and 23% developed a skin rash.181 Marine mammal work-related illnesses commonly reported by survey participants included seal finger, conjunctivitis, viral dermatitis, bacterial dermatitis, and nonspecific contact dermatitis. Severe illness was less commonly reported and included tuberculosis, leptospirosis, and brucellosis. Traumatic injury included deep wounds (77), bites (38), wounds requiring sutures (26), and fractures (Figure 56-31, online).
Marine mammals carry many of the pathogens associated with food-borne gastroenteritis, such as Escherichia coli, Salmonella, and Listeria, although there are no documented cases of transmission to humans. Like other wildlife, seals and sea lions can shed the protozoan Giardia lamblia in their feces. In rare cases, marine mammals have been infected with rabies virus or Mycobacterium tuberculosis. From 1972 to 1977, five researchers were diagnosed with leptospirosis after working with California sea lions.300
The organism most likely responsible for seal finger is Mycoplasma phocacerebrale. Seal finger (see Chapter 79) is a condition that has been frequently reported by seal researchers and handlers. Although seal finger is usually treated effectively with tetracycline, serious sequelae, including septicemia, have been reported.181,322 In 1998, a calicivirus (i.e., the San Miguel sea lion virus) was isolated from blisters on the hands and feet of a laboratory worker.325 Sealpox is a cutaneous condition caused by parapoxvirus that usually affects seal handlers who have been bitten by infected harbor or grey seals.325 In 1987, two researchers developed cutaneous lesions consistent with sealpox after working with grey harbor seals.323
Seals
Pinnipeds are comprised of true seals, earless seals, and walruses. Attacks on humans are rare. Grey harbor seals have pointed sharp teeth for tearing and grasping, and often use their back teeth for crushing shells. In 2005, a woman was trying to help a seal back into the water when it bit off her nose.288 In San Francisco, California, in 2006, the Aquatic Park reported 14 separate biting incidents, all attributed to the same baby harbor seal. On average, 10 seal bites per year are reported in the United States277 (Figure 56-32, online).

FIGURE 56-32 Monk seal.
(Courtesy National Oceanic and Atmospheric Administration Fisheries, Pacific Islands Fisheries Science Center, taken under Marine Mammal Protection Act/Endangered Species Act Permit #848-1365.)
The much larger leopard seals of the Antarctic are apex predators, weighing up to 500 kg (1102.3 lbs) with canine teeth that are 2.5 cm (1 inch) long. Attacks on humans are rare. In 1985, an explorer reported having been bitten twice by a leopard seal as it tried to drag him into the sea; in 2003, a leopard seal killed a researcher when she was pulled underwater and drowned.65,253 Ernest Shackleton described a leopard seal attack that occurred during his ill-fated Antarctic expedition.253
Walruses
Walruses (Odobenus rosmarus) are large marine mammals with a discontinuous circumpolar distribution in the Arctic Ocean. The most prominent physical features of the walrus are long tusks (actually elongated canines) that are present in both genders and can reach a length of 1 m (3.3 feet). They have few other teeth, and use the tusks to rake the ocean bottom for food.41 A full-grown bull can weigh 1814.4 kg (2 tons) and challenge a polar bear. Few human attacks have been documented as a result of both geographic isolation and the walrus’ generally shy nature. The rare human conflict usually involves an injured or provoked animal.
Sea Lions
Sea lions (family Otariidae) have four large canine teeth with smaller incisors and cone-shaped teeth. A sea lion’s teeth are designed for grasping and tearing rather than chewing. Sea lions tend to flee if possible, but they are capable of delivering powerful bites when threatened. Although sea lions are not typically aggressive, a series of attacks was reported in San Francisco Bay in California in 2006, when 14 people were bitten. In 2004, a sea lion pulled a fisherman from his boat, but he was able to escape unharmed.341
Elephant Seals
Elephant seals (genus Mirounga) are very large mammals that can move surprisingly fast on land. Attacks on humans are rare and in most cases provoked (e.g., when the seal is surprised or approached too closely). Northern (Mirounga angustirostris) and southern (Mirounga leonina) species are both found in the Pacific region. Elephant seals have large incisors and are capable of breaking bones with even a small bite.223 In 2007, a series of attacks were attributed to one bull elephant seal in the San Francisco Bay Area of California; the animal bit a surfer, a kayaker, and a pitbull dog.223 As is the case with other marine mammals, seal finger is a potential complication of an elephant seal bite.34
River Otters
The first recorded biting of a human by a river otter was in 1998 in Minnesota. In 2004, a family of three was attacked while swimming in calm river water near Belden, California.166 A 12-year-old boy was suddenly attacked both above and below the water by a river otter, and was bitten and scratched over much of his body. The otter then attacked the child’s mother and father when they arrived to help, and the attack was described as “vicious and unrelenting” despite many attempts by the three to strike and repel the animal. State game officials were unable to locate or capture the animal. The victims’ sutured lacerations healed without incident after prophylactic treatment with amoxicillin–clavulanate, and they received rabies PEP (Figure 56-33).
The CDC has recorded 24 rabies cases in river otters, and wildlife experts suppose that, as a result of low population densities and a semi-aquatic existence, otters probably have limited opportunities to contract diseases from other species. Otters travel along rivers while denning, allowing contact with raccoons, which carry a rabies strain that is enzootic in raccoon populations.289
Domestic Animal Attacks
Most animal bites are from domestic dogs and cats. The great majority of bites (approximately 80% to 90%) are inflicted by dogs,160 and approximately 1 in every 775 persons seeks emergency care for dog bites each year.332 In 2001, an estimated 368,245 people were treated in U.S. hospitals for nonfatal dog-bite–related injuries.75 Domestic cats account for about 5% to 15% of treated bites, although some studies report a figure as high as 25%.160,218,351 The bite location and affected populations vary by animal. Most dog bites occur on the extremities. Facial bites are more common among children, and up to two-thirds of cat bites are on the upper extremities, especially the hand.149,303
A comprehensive study that evaluated 50 patients with dog bites and 57 patients with cat bites identified a median of five bacterial isolates per culture (see Box 56-8).314 Pasteurella species were the most common pathogens found in bites of both dogs (50%) and cats (75%).314 The association of Pasteurella with infections of rapid onset was confirmed. Streptococcus, Staphylococcus, Moraxella, Corynebacterium, and Neisseria were the next most frequent aerobic isolates. Eikenella corrodens, usually associated with human bite infections, was found in only one cat and one dog bite wound. Capnocytophaga species and Weeksella zoohelcum, both of which can cause invasive sepsis, were uncommon in this study and may be opportunistic pathogens. Fusobacterium, Bacteroides, Porphyromonas, and Prevotella were common anaerobic isolates.27
Dogs
Dogs who are less than 1 year old are responsible for the highest incidence of bites.75 The incidence of biting increases substantially during the summer months. The increased susceptibility of children results from their smaller size, relative inability to defend themselves, interest in animals, and unintentional abuse of animals.
Wounds from dog attacks may comprise a mixture of biting, clawing, and crushing forces. An adult dog can exert 200 to 300 psi of pressure.11 As a result, deeper tissues may also be injured. Treatment may naturally focus on the crush component of the wound, but the penetrating component may cause the most morbidity. The dog may move and shake its head during the attack, further tearing tissue. Snorting, grunting, or wound manipulation by the biting animal may force air into the tissues. In addition to infectious organisms, foreign debris and teeth may be deposited. During a severe attack, the dog may eat tissue and blood or scavenge on an unconscious or intoxicated victim.159,268 Dog bites to the genitalia have been reported, rarely resulting in orchiectomy.118,155
Dog attacks kill 10 to 20 people in the United States annually,332 and the majority of those killed are children.284 Forty-nine states reported dog-related fatalities, with Alaska reporting the highest death rate from dog attacks. The number of dog-related deaths appears to be increasing.202
Worldwide, dogs are responsible for about 50% of animal-related injuries to travelers.144 A study done in Thailand of adult travelers at the international airport reported that 1.3% had been bitten by a dog.263
In Africa, there are more people than dogs living in cities compared with villages, and in Asia, there are more dogs than people in cities compared with villages.191 This would suggest that one is more likely to be bitten by a dog while traveling in rural Africa or urban Asia.
Risk factors for increased biting propensity include male dog gender and unneutered status. Many dogs that seriously wound or kill humans have long histories of aggressive behavior. Strategies that reduce biting risk include education of owners and the public, selection of dogs, and training, care, and socialization (see Box 56-2).
Cats
Cats have a weaker biting force than do dogs, but possess sharp, slender teeth, often producing deep puncture wounds. Their bites are associated with a 15% to 80% infection rate314 and a higher incidence of osteomyelitis and septic arthritis compared with dog bites. Cat bites frequently introduce two risk factors for infection: hand location and increased depth of puncture. Other risk factors in cat bites associated with wound infections include older victims, longer delay to emergency department treatment, wound inflicted by a pet rather than a stray, wound care at home, and more severe wounds.111
Cat-scratch disease is an uncommon disease; 90% of cases are caused by scratches from domestic cats, although it has also been reported in one big-cat attack victim.100,190 The average incubation period is 3 to 10 days. The characteristic feature is regional lymphadenitis, which usually involves the lymph nodes of the arm or leg. In most cases, clinical diagnosis is based on finding three of the following four criteria:100
Detailed information about the diagnosis and treatment of this disease is found in Chapter 59.
Because the hands and lower extremities are common sites of injury and wounds may be deep and penetrating, most cat bites are considered to be high risk for infection. Such wounds should prompt administration of prophylactic antibiotics (see Box 56-6). Superficial cat bites and scratches elsewhere on the body are not high risk and should receive standard wound care without antibiotic coverage.
Rodents
Rodents do not tend to bite unless severely provoked; their bites are usually small and do not cause much disability. The exact number of rodents in the world is unknown, but they probably number in the hundreds of millions. A 2007 U.S. pet ownership survey showed the following ownership per 1000 households: 1060 ferrets, 1239 hamsters, 1004 guinea pigs, 431 gerbils, and 949 other rodents.10 Despite these numbers, rodent bites account for only 1.7% to 10% of animal bites brought to medical attention.248
Rats, Mice, and Other Small Rodents
Rat bites have an infection rate of 2% to 10%, even without treatment, and the rate is usually on the low end of this spectrum.248 Other than bites inflicted by laboratory animals, the vast majority occur in poor communities while the victim is sleeping and involve the face and neck, usually of infants or physically or mentally disabled adults.247,248 There were 415 reported rat bites in New York City between 1986 and 1994.87 Sometimes these can be severe; a week-old infant was bitten around the eyes by a rat, resulting in perforations of the globe, an estimated vascular loss of 55% of red blood cell mass (with an initial hematocrit value of 20%), and eventual blindness.236 Despite the rat’s reputation for spreading disease, however, infection did not occur. Similar bites in infants have resulted in loss of more than three-fourths of the eyelids.352
The bacteriology of a rat bite is similar to other animal species; the various systemic diseases transmitted by rats are discussed in Chapters 59 and 60. Sporotrichosis has been reported; this widely distributed saprophyte is found on various plants, in the soil, and on many animals.140
Although rodents occasionally become infected with rabies, they seldom secrete this virus in saliva; therefore, they inflict extremely low-risk bites with regard to the transmission of the disease. However, local epidemics can occur, as documented in the 1980s among rodents and lagomorphs on the east coast of the United States.233 During that epidemic, woodchucks constituted 80% of all rabid animals; the remainder were squirrels, beavers, rabbits (lagomorphs, not rodents), and one rat. Some of these rabid animals were very aggressive; a woodchuck attacked and knocked down an elderly woman in her garden, biting her repeatedly. Rabies was isolated from the buccal cavity of the woodchuck in question. A reasonable current recommendation is that a biting wild rat in the United States should be caught and examined for rabies, and rabies PEP should be initiated only if the rabies test is positive; rabies PEP is probably appropriate for bites from uncaptured rodents inflicted outside of the United States and Canada.248 A case has been reported of a cowpox-virus–like infection transmitted by a probable rat bite.342 Rodents are believed to be the natural reservoir of the cowpox virus.
Rat-bite fever is an acute illness caused by Streptobacillus moniliformis or Spirillum minus, which are part of the normal oral flora of rodents, including squirrels. It may also result from bites of wild and domestic carnivores, such as weasels, dogs, cats, and pigs, which may have become infected when hunting rats and mice.290 Carrier rates among wild rats vary from 50% to 100%.330 Fewer than 100 cases have been reported in the North American literature, and rat-bite fever is not a reportable disease in the United States.330 Although relatively rare, cases can occur in any setting, and can easily be fatal, particularly when the proper diagnosis is not suspected.100,287,330 Further information is found in Chapter 59.
Plague is caused by the bacterium Yersinia pestis. Wild plague is endemic in many parts of the world, chiefly among rats, mice, moles, marmots, squirrels, hares, cats, and mongeese. One of the larger areas of endemic plague is the western United States, where voles, field mice, ground squirrels, prairie dogs, and pack rats carry the infection. Between 1971 and 1999, there was an average of 13 cases of plague per year in that area of the country, but only 2 cases were reported in 2001; however, worldwide, there were 2861 cases reported by 10 countries.103 The infection is usually transmitted to humans by the bites of arthropods that infest infected animals. Handling infected animals allows Yersinia pestis to enter cuts and abrasions, as seen among veterinarians and hunters who skin and clean infected rabbits.72 Transmission by bite or scratch has never been reported. The disease is mentioned here because of its historic significance and the frequency of occurrence among wild animals. Further information is found in Chapter 59.
Tularemia represents various syndromes caused by Francisella tularensis. This bacterium normally parasitizes about 100 different mammals and arthropods, most commonly cottontail rabbits, rodents, hares, moles, beavers, muskrats, squirrels, rats, and mice. The primary mode of transmission to humans is via a bloodsucking arthropod (e.g., a tick) or by skin or eye inoculation resulting from skinning, dressing, or handling diseased animals. Other routes of infection include ingestion of water that has been contaminated by urine or feces and inhalation of dust. Infections after bites or scratches from dogs, cats, skunks, coyotes, foxes, and hogs have been reported, although these are rare.273 The disease is an occupational hazard of hunters, butchers, cooks, campers, and laboratory technicians. Humans are quite susceptible, and, although tularemia was removed from the national notifiable disease list in 1995, 105 cases were reported in 1997 in the United States.76 More information is found in Chapter 59.
Rabbits
Rabbits are a common household pet. They are not true rodents but rather part of the Lagomorpha order and more closely related to horses. Rabbits cannot see in front of their noses, so they may bite a hand that is placed there. They also nip as a means of communication, although such behavior on the part of the rabbit can be interpreted as aggression. Biting is uncommon, but rabbits can inflict painful scratches with their rear limbs when restrained.168
Pasteurella multocida from scratches may cause cutaneous infection in humans.167 Other diseases to which rabbits are susceptible, such as salmonellosis, yersiniosis, and tularemia, are rare. Direct zoonotic transmission of Yersinia pseudotuberculosis from domestic rabbits has been documented.138 More commonly, some external parasites of the rabbit, including fur mite acariasis (Cheyletiella) and dermatophytosis (Trichophyton), may be transmitted to humans.167
Ferrets
The two species of ferret in the United States are the common ferret Mustela putorius furo, which is sold as a domestic pet, and the wild black-footed ferret Mustela nigripes, which is an endangered species. The pet ferret was domesticated from the wild European polecat, and was first introduced into the United States during the late 19th century. Ferrets are kept in increasing numbers as domestic pets, especially by urban apartment dwellers (Figure 56-34).
Ferrets were bred to hunt and kill small game and rodents in their burrows, and are particularly attracted to suckling animals, possibly because of the scent of milk. The animals have 34 teeth and sharp claws on all four feet. Severe injuries caused by ferrets are not common. When they occur, an infant is often the victim, and is typically sleeping or in a crib. The face, ears, and nose may be mutilated.12 Scratches, lacerations, and puncture wounds are seen, and the ferret may chew on a victim (e.g., a baby’s ear). The neck is also a common target.
In a comprehensive review of 452 ferret attacks over 10 years, virtually all unprovoked attacks were on the faces of unattended infants.98 Most victims were less than 3 years old and were attacked while sleeping or lying down. Several injuries were severe, and one child died. Bites were usually multiple, and sometimes the ferret’s jaws had to be pried open or the ferret had to be killed to secure release.255 Nearly all provoked incidents involve neglect, abuse, or roughhousing with the ferret that it likely perceived as an attack; some of the animals involved in these incidents were ferret–polecat hybrid crosses.37
Ferrets are unusually adept at escaping from cages and enclosures, guaranteeing that they will occasionally be loose unsupervised in the house and also that they can escape to the wild, where they may be exposed to endemic rabies. In one study, 4% of biting ferrets were found to be positive for rabies virus.98 Ferrets are now classified in the same category as cats and dogs (rather than as wild terrestrial carnivores) with regard to rabies pathogenesis and viral shedding patterns. They may be confined and observed for 10 days rather than being routinely euthanized after biting. An effective rabies vaccine for ferrets, IMRAB-3, has been available since 1990, although it requires annual vaccination.
Little is known about infection rates or bacteriology in ferret-inflicted wounds, although unusual species such as Mycobacterium bovis have been observed.184 Initial treatment should be the same as it is for dog bites.
Domestic Herbivores and Ungulates
From 1992 to 2000, there were averages of 40 deaths and 12,400 nonfatal injuries and illnesses related to animals in the United States annually. Most of these incidents involved domestic farm animals.82,228 Between 1990 and 1993, horses were the second leading cause of farm-related injuries.280 Farm animals cause a disproportionate number of injuries relative to other animals, especially among youth; 6438 on-farm injuries occurred among young victims in 1998. Approximately 41% of those injured were less than 10 years old; 37% of incidents involved horses, and 31% involved cattle. Most of the cattle-related injuries were work related, whereas horse-related injuries were mainly nonoccupational.301 One out of every five youth injuries that occurs on farms in the United States is animal related.301 A Wisconsin study showed that, for injuries requiring hospital admission, farm animals were the cause of 40% of the injuries. The study also revealed that the types of injuries caused by farm animals include those to the head, upper extremities, maxilla, legs, and thoracoabdominal region.94 A study of youth on farms in Australia indicated that 86% reported working with farm animals and in 44% of injuries among this population, the injury was caused by a farm animal. In addition, 72% of youths surveyed perceived working with animals as the most dangerous activity on the farm.82
Little is known about incidence of wound infection after herbivore bite, but the infection rate after camel bites may be as high as 86%.203 Species of Actinobacillus lignieresii, Actinobacillus suis, and Pasteurella multocida have been isolated from infected horse and sheep bites.38,258 Most domestic herbivores carry Pasteurella, and most are given frequent and regular doses of different antibiotics, especially in their feed, leading to antibiotic resistance of bite wound organisms.269 Pasteurella caballi has been isolated from a horse bite wound.127 Staphylococcus hyicus subsp. hyicus, a well-known cause of disease in many animals, has been reported as a human wound pathogen after a donkey bite.251 Bites from horses, donkeys, cattle, sheep, camels, deer, and most other herbivores are treated with the same antibiotics as are bites from dogs, cats, and humans (see Box 56-6).
Horses and Donkeys
The horse (Figure 56-35) is inclined to both bite and kick, but most horse-related injuries follow a fall during riding activities. More accidents occur per hour riding horses than during motorcycling.88 Young females are most often injured by falls,57 and head injuries cause the majority of deaths.165 Appropriate helmets and footwear help to reduce the severity of injuries. A report of a series of horse- and cow-related injuries found a high correlation of occult craniofacial and torso injuries when field assessment documents the presence of upper extremity injury.243 Falls from horses typically result in head and upper extremity injuries; the most common injuries are fractures, lacerations, and contusions.67 From 1992 to 1994, 109 traumatic brain injuries caused by falls from horses were reported in Oklahoma; these included 3 deaths.71 Twenty-three other traumatic brain injuries resulted from horse-caused injury but were not associated with riding; 21 of these traumatic brain injuries resulted from a direct kick to the head.71
Horse bites are common but usually do not cause severe injuries. The occlusal surfaces of both the horse’s lower and upper incisors are flattened. However, most male horses possess canines that may be used to grab onto a mare’s neck during mounting. The soft-tissue contusions inflicted by a horse can be substantial, but, in a series of 24 horse bites, 21 healed uneventfully.122 Bites can still produce significant injury, including muscle rupture and fat necrosis, with no external wound. Horses also have a propensity for biting human nipples, which are at the same height as a horse’s mouth.
Horse kicks from the rear legs can be extremely powerful and cause severe blunt trauma, including cardiac rupture50 and massive pulmonary embolism.267 Donkeys also bite, and death has been reported from fat embolism caused by fractures after a donkey bite.48
Cattle
Cattle are usually docile, but can inflict a variety of injuries. Serious bites are infrequent, because these animals possess neither upper incisors nor canines. A cow typically weighs 635 kg (1400 lbs), and a bull can exceed 1360.8 kg (3000 lbs). Accidental treading on the human victim or butting can cause major crush injuries and fractures. Farm animals in Wisconsin kill about six people each year.59 One hospital in rural Wisconsin treated an average of 22 persons per year for horse and cattle injuries, most of which were inflicted by a kick or another assault. In addition, domestic cattle can become infected with rabies (Figure 56-36, online).
Cattle horn injuries or gorings (Figure 56-37) present typical and unique damage patterns. The horns are used in an inward hooking motion to butt and fling the victim, or the horn tip can be used for goring. Goring injuries seen in bullfighting typically involve the perineum and thigh; they tend to be deep and sometimes fatal. By contrast, bull horn injuries from domestic cattle involve a sweeping arc at the level of the bull’s head, which is at the level of the human abdomen. The semicircular motion of the horn often produces a relatively superficial laceration that leaves deeper structures of the abdomen intact. In one series of 29 cases in which the peritoneum was breached, which usually produced a prolapse of bowel or omentum, 27 laparotomies demonstrated no additional injuries; in only a few cases was the bowel itself damaged.293 The wound infection rate in this series was high (54%), probably as a result of delayed treatment.
There were 108 cattle-related deaths in the United States between 2003 and 2007. Twenty-one deaths from working with domestic cattle were reported between 2003 and 2008 in the four U.S. states that accounted for 16% of all cattle operations in the United States. Ten of these fatalities involved attacks by bulls, six were attacks by individual cows, and five involved multiple cattle. In seven attacks, the bull or cow was known to have exhibited past aggressive behavior, and one-third of the deaths occurred in March and April. The victims’ most common activities at the time of death were working with and treating cattle in enclosed spaces (e.g., pens, chutes) and moving or sorting cattle in pens, barns, or pastures. In 16 of the cases, the animal was deemed to have purposefully struck the victim; five other deaths were caused by being crushed against a stationary object or struck by a gate. All but one death resulted from blunt force trauma to the chest, head, or both.69
Camels
In regions in which camels are used for domestic or agricultural purposes, bite injuries are quite common.203 Although herbivores and usually docile, camels are much more likely to bite in the winter rutting season, and bite fatalities have been reported. Camels have 34 teeth, including large backward-inclined upper canines or tushes (Figure 56-38). The lower tushes are placed relatively forward, and the resultant mouth grip is very effective. Jerking movements of the head result in severe tissue damage and limb avulsion, and rarely can break the human victim’s neck. The forearm is often injured, and bites to the face are well documented.66,246,299 Virtually all camel bites are single.286 Injury or death can also occur if the camel presses the victim to the ground and crushes him or her after gripping the person in its jaws.203
Domestic Swine
Bites from domestic swine are rare; however, when pigs attack, they can be aggressive and inflict deep goring or bite injuries, often on the posterior thigh as the pig approaches from behind.28,242
Pigs have a reputation for inflicting bites that are at high risk for infection, and care should include thorough wound exploration and debridement. The usual wide range of bacterial pathogens is reported, including Pasteurella aerogenes, Pasteurella multocida, Bacteroides, Proteus, Actinobacillus suis,126,161 and hemolytic streptococci, including Streptococcus milleri.28 Unusual gram-negative bacteria, such as Flavobacterium group IIb, have been isolated, as has Mycoplasma.42,231 Both of these organisms are resistant to amoxicillin–clavulanate, so the addition of ciprofloxacin is recommended as prophylaxis for a serious pig bite wound.231
Birds
Birds may be kept as domestic pets or on farms, and can be responsible for serious injuries. On farms, rooster attacks, often by male fowl defending their territory, are well documented. Children, especially infants, are particularly vulnerable to attack. Rooster injuries have included serious clawing of the face and a fractured skull.271 In one report, a rooster spur was retained in a wound, resulting in chronic infection.99 Septic arthritis was reported in a child after a bite from a domestic fowl.178
Medicolegal Considerations
Although most wild animals by definition do not have an owner, some exotic species are kept as “pets.” An owner’s failure to meet local regulations regarding licensure and vaccination can lead to legal action. In addition, the victim may seek compensation from the owner of the animal, with the result being that the health care provided and the victim’s medical record will be reviewed in court. The injury may be related to the victim’s employment, generating worker’s compensation or other insurance claims. Therefore, injuries and their circumstances should be documented as fully as possible, with line drawings or photographs added to the medical record whenever possible. In a recent tragic example in Connecticut, a woman was attacked by a friend’s pet chimpanzee. Her injuries required 7 hours of extensive surgery, and the patient is predicted to have permanent disabilities. Her family has filed litigation against the owner of the chimpanzee.15
2 Adolph H: Personal communication, 1999.
4 Agence France-Presse. Kangaroos a deadly Aussie road menace: study. http://www.google.com/hostednews/afp/article/ALeqM5hcuoFuPtSXcjOgzQkU9ot6RiWpcA.
5 Agence France-Presse. Komodo dragon kills man in Indonesia. http://www.news.com.au/breaking-news/komodo-dragon-kills-man/story-e6frfku0-1225696990556.
6 Agence France-Presse. Scientists discover deadly secret of Komodo’s bite. http://www.google.com/hostednews/afp/article/ALeqM5hVmc_PKzCdhfs-dEi2kE0CS2CybA.
8 Alaska Department of Fish and Game. What to do about aggressive moose? http://www.adfg.alaska.gov/index.cfm?adfg=livewith.aggressivemoose.
9 Alberio L, Lammle B. Capnocytophaga canimorsus sepsis. N Engl J Med. 1998;339:1827.
10 American Veterinary Medical Association. U.S. pet ownership & demographics sourcebook (2007 edition). http://www.avma.org/reference/marketstats/sourcebook.asp.
11 Answers.com. What dog breed has the strongest bite force? http://wiki.answers.com/Q/What_dog_breed_has_the_strongest_bite_force.
12 Applegate JA, Walhout MF. Childhood risks from the ferret. J Emerg Med. 1998;16:425.
13 Arizona Game and Fish Department. Confirmed mountain lion attacks in the United States and Canada 1890—present. http://www.azgfd.gov/w_c/mtn_lion_attacks.shtml.
14 Arizona reporting a busy year for rabies. Bozeman Daily Chronicle May 4, 2008.
15 Associated Press. Chimp attack victim may have brain damage. http://www.nypost.com/p/news/regional/chimp_attack_victim_may_have_brain_kf8LkZrDOjMCjDBjkKFLUL.
16 Associated Press: Coyote attacks 3-year old boy on Cape Cod. Boston Globe July 30, 1998.
17 Associated Press. Elephants rampage through villages in India. http://www.foxnews.com/story/0,2933,138495,00.html.
18 Associated Press: Humans and elephants battle for survival: 8 people, 10 animals dead in Sri Lanka. San Francisco Chronicle September 27, 1993.
19 Associated Press: Ostrich kicks 63 year old woman to death in South Africa. Globe Newspaper Co December 29, 1997.
20 Associated Press. Runaway deer makes surprise visit to law firm. http://www.igorilla.com/gorilla/animal/runaway_deer_makes_surprise_visit.html.
21 Associated Press: White-tiger owner killed in attack, Gainesville Sun November 22, 1998.
22 Attewill F. Boy killed in dragon attack. http://www.guardian.co.uk/world/2007/jun/04/1.
23 August JR. Dog and cat bites. J Am Vet Med Assoc. 1988;193:1394.
27 Barnham M. Once bitten twice shy: The microbiology of bites. Rev Med Microbiol. 1991;2:31.
29 Barry C. Komodo dragon’s bite is “weaker than a house cat’s.”. http://news.nationalgeographic.com/news/2008/04/080418-komodo-dragons.html.
31 BBC News. Lizard bites Sharon Stone’s husband. http://news.bbc.co.uk/2/hi/entertainment/1382755.stm.
32 Beck AM. The epidemiology and prevention of animal bites. Semin Vet Med Surg. 1991;6:186.
33 Beck AM, Jones B. Unreported dog bite in children. Public Health Rep. 1985;100:315.
34 Becker B: Personal communication, 2009.
37 Bell JA. Are ferrets good pets for children? http://www.peteducation.com/article.cfm?c=11&aid=527.
39 Berner R: The St. Nick of Belle Fourche, S.D., survives raucous reindeer attack. Wall Street Journal November 28, 1997.
40 Berryman Institute. Personnel: Faculty affiliates. http://www.wildlifeconflicts.org/personnel/affiliate.html.
41 Berta A, Sumich JL. Marine mammals: Evolutionary biology. San Diego, Calif: Academic Press; 1999.
42 Bettor eats a live bat. San Francisco Chronicle, August 31, 1989.
44 Big Bend Chat. Bobcat attack Wednesday. http://www.bigbendchat.com/portal/forum/big-bend-national-park-qa/bobcat-attack-wednesday-t192.0.html;msg1701.
46 Björnstig U, Eriksson A, Ornehult L. Injuries caused by animals. Injury. 1991;22:295.
48 Bloch B. Fatal fat embolism following severe donkey bites. J Forensic Sci Soc. 1976;16:231.
51 Brick M. Bacon a hard way: Hog-tying 400 pounds of fury. http://www.nytimes.com/2008/06/21/sports/othersports/21hogs.html?hp.
53 Brogan TV, Bratton SL, Dowd MD, et al. Severe dog bites in children. Pediatrics. 1995;96:947.
54 Brook TV: USA experiences population boom—of feral hogs, USA Today May 17, 2004.
58 Bureau of Labor Statistics. The editor’s desk: Animal attacks and on-the-job fatalities. http://www.bls.gov/opub/ted/2001/Jan/wk4/art04.htm.
61 Cape Argus. Baboon attacks Cape Point visitor. http://www.capeargus.co.za/index.php?fSectionId=49&fArticleId=21&94506.
64 Carbyn LN. Coyote attacks on children in western North America. Wildl Soc Bull. 1989;17:444.
65 Carrington D. Inquiry into fatal leopard seal attack begins. http://www.newscientist.com/article/dn3978-inquiry-into-fatal-leopard-seal-attack-begins.html.
73 Centers for Disease Control and Prevention. Human rabies. http://www.cdc.gov/rabies/location/usa/surveillance/human_rabies.html.
74 Centers for Disease Control and Prevention. Medical care: Rabies. http://www.cdc.gov/rabies/exposure/postexposure.html.
77 Centers for Disease Control and Prevention. Vaccination coverage among U.S. adults: National immunization survey—Adult, 2007. http://www.cdc.gov/vaccines/stats-surv/nis/downloads/nis-adult-summer-2007.pdf.
78 Chadwick J. New England’s venomous mammals. N Engl J Med. 1969;281:274.
79 Chang A. Scientists probe recent coyote attacks in California. http://www.usatoday.com/news/nation/2008-05-12-246483821_x.htm.
85 Chester T. Mountain lion attacks on people in the U.S. and Canada. http://tchester.org/sgm/lists/lion_attacks.html.
86 Chhabra M, Ichhpujani RL, Tewari KN, et al. Human rabies in Delhi. Indian J Pediatr. 2004;71:217.
92 Clarke J. Man is the prey. London: Andre Deutsch; 1969.
93 CNN. Worst states for auto deer crashes. http://www.cnn.com/2006/AUTOS/11/14/deer_crash/index.html.
94 Cogbill TH, Busch HM, Stiers GR. Farm accidents in children. Pediatrics. 1985;76:562.
95 Cohle SD, Harlan CW, Harlan G. Fatal big cat attacks. Am J Forensic Med Pathol. 1990;11:208.
101 County of Los Angeles Department of Health Services. Overview of zoonoses. http://www.lapublichealth.org/vet/docs/zoonosis_manual.pdf.
103 CureResearch.com. Prevalence and incidence of plague. http://www.cureresearch.com/p/plague/prevalence.htm.
105 Daoust PY. Porcupine quill in the brain of a dog. Vet Rec. 1991;128:436.
106 Defenders of Wildlife. Gray wolf. http://www.defenders.org/wildlife_and_habitat/wildlife/wolf,_gray.php.
112 Dixon A: Startled tiger kills trainer. Associated Press October 8, 1998.
113 Dragoo JW, Honeycutt RL. Systematics of mustelid-like carnivores. J Mammal. 1997;78:426.
114 Dreesen D: Zoonoses in animal care facilities. In Proceedings of the 4th National Symposium on Biosafety, 1996.
115 Drinking man nibbles bat ear. San Francisco Chronicle September 30, 1988.
117 Drummond A: British wildlife expert sought after Thai tiger savages boy. Times Newspapers Ltd 1998.
118 Dubosq F. Management of dog bite trauma of the external genital organs. Prog Urol. 2004;14:232.
119 Dunn R. The Quokka chronicles. http://www.nwf.org/News-and-Magazines/National-Wildlife/Animals/Archives/2007/The-Quokka-Chronicles.aspx.
121 Edberg J. Four wolves suspected in man’s death in remote area of Canada. http://www.timberwolfinformation.org/info/archieve/newspapers/viewnews.cfm?ID=2803.
122 Edixhoven P, Sinha SC, Dandy DJ. Horse injuries. Injury. 1981;12:279.
123 eMedTV. Statistics on rabies. http://rabies.emedtv.com/rabies/statistics-on-rabies.html.
125 Environmental News Network. Climate change linked to Indian tiger attacks. http://www.enn.com/wildlife/article/38442.
128 Farabe B: Personal communication, 1999.
130 Fell SD, Kukula CL. Animal bites. http://www.emedicinehealth.com/animal_bites/article_em.html.
132 Fimbres G. Rabid bobcat attacks two local hikers. http://www.tucsoncitizen.com/ss/local/83387.php.
134 Fishbein D. Rabies. Infect Dis Clin North Am. 1991;5:53.
135 Fleisher GR. The management of bite wounds. New Engl J Med. 1999;340:138.
136 Florida Fish and Wildlife Conservation Commission. Historic alligator bites on humans in Florida. http://myfwc.com/media/310203/Alligator_GatorBites.pdf.
139 Fox News. Jaguars quarantined following attack on zookeeper. http://www.foxnews.com/story/0,2933,480661,00.html.
141 Fry BG, Wroe S, Teeuwisse W, et al. A central role for venom in predation by Varanus komodoensis (Komodo Dragon) and the extinct giant Varanus (Megalania) priscus. http://www.pnas.org/content/early/2009/05/15/0810883106.
142 Gannon WL, Sikes RS. Guidelines of the American Society of Mammalogists for the use of wild mammals in research. Journal of Mammalogy. 2007;88:809, http://asmjournals.org/doi/abs/10.1644/06-MAMM-F-185R1.1?prevSearch=%5BAllField%3A+gannon+mammalian+bites%5D&searchHistoryKey=.
143 Garcia VF. Animal bites and Pasteurella infections. Pediatr Rev. 1997;18:127.
145 George J. Wolf attack a tragic, cautionary tale. http://www.sfgate.com/cgi-bin/article.cgi?f=/c/a/2006/01/14/HOGCRGL75U1.DTL.
149 Goldstein EJ. Bite wounds and infection. Clin Infect Dis. 1992;14:633.
156 Gomestic. Cat bites, ouch—More than you know about cat bites. http://gomestic.com/pets/cat-bites-ouch-more-than-you-know-about-cat-bites.
157 Gordon J. Woman killed by coyotes. http://www.sciencebuzz.org/blog/bursts/woman-killed-coyotes.
158 Greater Yellowstone Coalition. Home page. http://www.greateryellowstone.org.
162 Gunther K: Personal communication, 1999.
166 Hanna J: Personal communication, 2004.
167 Harkness JE. Rabbit husbandry and medicine. Vet Clin North Am Small Anim Pract. 1987;17:1019.
170 Haynes J: Wildlife encounters seldom fatal. San Francisco Examiner May 24, 1992.
171 Hewitt H. 2 elephant handlers killed in Vietnam. http://www.highbeam.com/doc/1Y1-106595121.html.
172 Highfield R. Elephant rage: They never forgive, either. http://www.smh.com.au/articles/2006/02/16/1140064206413.html.
179 Huggler J. Animal behaviour: Rogue elephants. http://www.independent.co.uk/environment/animal-behaviour-rogue-elephants-419678.html.
180 Hughes J: Tapir bites off zoo worker’s arm. Associated Press November 21, 1998.
181 Hunt TD, Ziccardi MH, Gulland FMD, et al. Health risks for marine mammal workers. http://www.int-res.com/articles/dao_oa/d081p081.pdf.
182 Jaffe AC. Animal bites. Pediatr Clin North Am. 1983;30:405.
185 Jones TR. Injuries by emus. Am J Emerg Med. 1996;14:336.
188 Kannikeswaran N, Kamat D. Mammalian bites. Clin Pediatr (Phila). 2008;48:145.
192 Knox ML: Close encounters of the feline kind: Big cats on the prowl. San Francisco Examiner January 6, 1991.
194 Korytin S: Sex and age structure of people attacked by wolves in different seasons. In Proceedings of the Scientific Conference: Issues of applied ecology, game management and fur farming. 1997.
195 Koslow B: Woman recalls attack by rabid fox, News-Journal Web Edition June 4, 1997.
198 Kvinta P: Stomping grounds. National Geographic Adventure August 2004, p 65.
199 LaGuardia A: Animal attack files. Electronic Telegraph London October 2, 1998.
200 Landercasper J, Cogbill T, Strutt P, et al. Trauma and the veterinarian. J Trauma. 1988;28:1255.
201 Langley J. The incidence of dog bites in New Zealand. N Z Med J. 1992;105:33.
205 Leonard T: Tiger bites off keeper’s arm. London Daily Telegraph February 26, 1998.
208 Linnell JDC, Andersen R, Andersone Z, et al. The fear of wolves: A review of wolfs attacks on humans. http://www.nina.no/archive/nina/PppBasePdf/oppdragsmelding/2002/731.pdf.
209 Loefler IJ. Letter to editor. J Trauma. 1997;43:560.
211 Lyons R. 90’s pets, the more exotic the better. New York Times. 1991;140:34(L).
212 MacClintock D. A natural history of raccoons. Caldwell, NJ: Blackburn Press; 1981.
213 MacIntyre B: Wild boars lay waste to French countryside. Times Newspapers Ltd January 6, 1998.
215 Man strangles bobcat that attacked him. Chicago Tribune June 21, 2007.
217 Matarazzo BJr. Salem family’s ‘pet’ raccoon bites child. http://www.salemnews.com/local/x1048572752/Salem-familys-pet-raccoon-bites-child.
220 McColl KA, Tordo N, Aguilar Setién AA. Bat lyssavirus infections. Rev Sci Tech. 2000;19:177.
223 McHugh P. Aggressive elephant seal menaces Sonoma Beach. http://www.sfgate.com/c/acrobat/2007/04/24/Chronicle.04-24-2007.ALL.A.1.MainNews.5star-dot.pdf.
224 McNay ME. A case history of wolf-human encounters in Alaska and Canada. http://www.adfg.alaska.gov/static/home/library/pdfs/wildlife/research_pdfs/techb13p1.pdf.
225 Medeiros I, Saconato H: Antibiotic prophylaxis for mammalian bites. Cochrane Database Syst Rev (2):CD001738, 2001.
227 Mitchell K, Aguilera E, Espinoza A. Zoo mourns mauled keeper. http://www.denverpost.com/news/ci_5298391.
231 Morgan MS. Treatment of pig bites [letter]. Lancet. 1996;348:1246.
232 Morin R: Block Island struggles with deer. Globe Newspaper Co October 5, 1997.
235 Murphy K. Wolves kill teacher in Alaska. http://articles.latimes.com/2010/mar/13/nation/la-na-wolf-attack13-2010mar13.
237 National Park Service, U.S. Department of the Interior. Yellowstone: Frequently asked questions about bison: How many bison live in Yellowstone National park? http://www.nps.gov/yell/naturescience/bisonqa.htm.
238 NBC Anchorage Affiliate Channel 2 evening news. January 9, 1995.
239 New Mexico Wildlife News. Search continues for mountain lion that killed Pinos Altos man. http://www.wildlife.state.nm.us/publications/press_releases/documents/2008/062308pinosaltoslion.html.
240 Newcomer CE: Zoonoses in animal care facilities. In Proceedings of the 4th National Symposium on Biosafety. 1996.
247 Olivarius F. Rat bites. Cutis. 1994;53:302.
248 Ordog G, Balasubramanium S, Wasserberger J. Rat bites: Fifty cases. Ann Emerg Med. 1985;14:126.
249 Oregon Department of Fish and Wildlife. Key facts about cougars in Oregon and the cougar management plan. http://www.dfw.state.or.us/wildlife/cougar/.
250 Osborn L. Number of species identified on Earth. http://www.currentresults.com/Environment-Facts/Plants-Animals/number-species.php.
253 Owen J. Leopard seal kills scientist in Antarctica. http://news.nationalgeographic.com/news/2003/08/0806_030806_sealkiller.html.
257 Peaco J: Personal communication, 1999.
259 People for the Ethical Treatment of Animals. Circuses. http://www.peta.org/issues/animals-in-entertainment/circuses.aspx.
265 Pickles G. Injuries by wild animals in the African bush. J R Army Med Corps. 1987;133:159.
271 Preiser G, Lavell TE. Rooster attacks on children. Pediatrics. 1987;79:426.
272 Queensland Environmental Protection Agency. Risk assessment: Risk to humans posed by the dingo population on Fraser Island. http://www.env.qld.gov.au/cgi-bin/w3-msql/environment/park/fraser/msqwelcome.html:page+dingo_risk.pdf.
273 Quenzer R, Mostow S, Emerson J. Cat-bite tularemia. JAMA. 1977;238:1845.
274 Rajpurohi KS. Child lifting: Wolves in Hazaribagh, India. http://www.faqs.org/abstracts/Environmental-issues/Child-lifting-wolves-in-hazaribagh-India-Geospatial-indicators-of-emerging-water-stress-An-applicati.html.
275 Rauber P: When nature turns nasty. Sierra November/December:46, 1993.
276 Reuters. Lost Costa Rica minister found with tapir bite. http://www.thehumorsource.com/item/76057?order=views.
277 Reuters. Seal bites off woman’s nose. http://www.underwatertimes.com/forum/viewtopic.php?p=1920.
278 Reuters: Wild monkeys wound 26 people in attacks on Japanese town. Nando Times January 26, 1998.
281 Rodrigo M. Day of the jackal. http://sundaytimes.lk/070923/Plus/plus00024.html.
284 Sacks JJ, Lockwood R, Hornreich J, et al. Fatal dog attacks, 1989-1994. Pediatrics. 1996;97:891.
285 Sathu JN: Kashmir monkeys storm city. Electronic Telegraph February 3, 1999.
286 Saxena PS, Sharma SM, Singh M, et al. Camel bite injuries. J Indian Med Assoc. 1982;79:65.
288 Seal attacks swimmers in aquatic park. San Francisco Examiner November 16, 2006.
289 Serfass T. Rabies in a river otter intended for reintroduction. J Zoo Wildl Med. 1995;26:311.
291 Shattock F. Injuries caused by wild animals. Lancet. 1968;1:412.
293 Shukla HS, Mittal DK, Naithani YP. Bull horn injury: A clinical study. Injury. 1977;9:164.
296 Siebert C. An elephant crackup? http://www.nytimes.com/2006/10/08/magazine/08elephant.html.
303 Smith PF, Meadowcroft AM, May DS. Treating mammalian bite wounds. J Clin Pharm Ther. 2000;25:85.
304 South Dakota Department of Health. How to submit animal specimens to the South Dakota Public Health Laboratory for rabies testing. http://doh.sd.gov/Lab/rabies.aspx.
306 Spence G. A review of animal bites in Delaware—1989 to 1990. Del Med J. 1990;62:1425.
307 Spillius A: Hungry monkeys on rampage. The Telegraph UK November 12, 1998.
309 Stevens WK: Survival of the big cats brings conflict with man. New York Times August 2, 1994.
311 Suhr J: Urban coyotes: Predators thriving in big cities throughout the East, Midwest. Bozeman Chronicle June 18, 2007.
312 Suite 101. Wildlife preservation: Preventing moose road accidents. http://wildlifepreservation.suite101.com/article.cfm/preventing_moose_road_accidents.
316 The American Ferret Association. Home page. http://www.ferret.org.
317 The Hunting Report. Water buffalo incident in Australia. http://www.huntingreport.com/hunting_article_details.cfm?id=1517.
318 Timm RM, Baker RO, Bennett JR, et al. Coyote attacks: An increasing suburban problem. http://repositories.cdlib.org/anrrec/hrec/timm_baker_P047.
321 United States Forest Service. Eastern cougar. http://www.fs.fed.us/r9/forests/white_mountain/projects/forest_plan_revision/viability/animals/eastern_cougar.pdf.
322 University of California Davis School of Veterinary Medicine. Marine mammal zoonotic bacteria. http://www.vetmed.ucdavis.edu/whc/mmz/bacteria.htm#Marine%20Mammal%20Zoonotic%20Bacteria%A0.
323 University of California Davis School of Veterinary Medicine. Working with marine mammals and your health. http://www.vetmed.ucdavis.edu/whc/mmz/Occupational%20Safety.htm.
326 Vanwersch K. Crocodile bite injury in southern Malawi. Trop Doct. 1998;28:221.
327 Varadarajan T: Fear of U.S. epidemic grows after young girl is bitten by rabid fox. Times Newspapers Ltd February 25, 1998.
328 Varty JD: Man survives cougar attack by killing it. CP Broadcast News, August 2, 2002.
333 Wiens MB, Harrison PB. Big cat attack: A case study. J Trauma. 1996;40:829.
335 Wikipedia. Gray wolf: Attacks on humans. http://en.wikipedia.org/wiki/Gray_Wolf#Attacks_on_humans.
336 Wikipedia. Kangaroos: Interactions with humans. http://en.wikipedia.org/wiki/Kangaroo#Interaction_with_humans.
337 Wikipedia. Raccoons: Distribution in Germany. http://en.wikipedia.org/wiki/Raccoon#Distribution_in_Germany.
338 Wilderness Medical Society: Personal communication, 2004.
341 Wohlsen M. Sea lion attacks raise flags. http://dsc.discovery.com/news/2006/11/28/sealion_ani.html.
343 Wong AK, Huang SW, Burnett JW. Hypersensitivity to rat saliva. J Am Acad Dermatol. 1984;4:606.
346 World Health Organization. First dose of diphtheria toxoid, tetanus toxoid and pertussis vaccine. Reported estimates of DTP 1 coverage. http://apps.who.int/immunization_monitoring/en/globalsummary/timeseries/tscoveragedtp1.htm.
347 World Health Organization. Scene setting: Epidemiological and geographical distribution of rabies and envenomings, and the need for more good quality animal derived sera. http://www.who.int/bloodproducts/animal_sera/01-updated-WarrelWHO.pdf.
348 World Health Organization. Third dose of diphtheria toxoid, tetanus toxoid and pertussis vaccine. Reported estimates of DTP 3 coverage. http://apps.who.int/immunization_monitoring/en/globalsummary/timeseries/tswucoveragedtp3.htm.
349 World Health Organization. World health report. Geneva: World Health Organization; 1999.
350 World Health Organization; Pan American Health Organization. Reducing rates of unintentional injury. http://www.amro.who.int/English/DD/PUB/BBH_Violence.pdf.
352 Wykes WN. Rat bite injury to the eyelids in a 3-month-old child. Br J Ophthalmol. 1989;73:202.