CHAPTER 125 Biomechanics of the Spine in Sport
INTRODUCTION
The spine is a complex design of bony and soft tissues, allowing the human form to move through various ranges of motions and positions. It serves both to transfer forces between the upper and lower extremities and to actively generate forces.1,2 Both the biomechanical design of the spine and the biomaterial composition of the various tissues determine its response to external stressors and forces generated within the body. The design and composition also provide an incredible ability to adapt to these stressors; however, there is a finite amount of adaptation that can occur before structural failure and injury can result.3 The epidemiology and biomechanical analysis of sports-related spinal injuries has allowed for the identification of the precise mechanism of various spinal injuries. This has resulted in sporting rules changes, equipment modifications, and changes in skill techniques, all of which have lowered the incidence of catastrophic spinal injury.4–7
FUNCTIONAL ANATOMY
The osseous spine consists of 7 cervical, 12 thoracic, 5 lumbar, 5 fused sacral vertebrae and the coccyx. The ligaments, muscles, and intervertebral discs connect the vertebrae to form the four curves of the spine: the two lordotic curves of the lumbar and cervical spine and the two kyphotic curves of the thoracic spine and sacrum. This structural property helps the spine absorb forces of compression and also contributes to the coupled motions that occur in the spine.1,3
The functional spinal segmental unit is defined as two adjoining vertebrae, the disc between them, and their surrounding soft tissues.1,3,8,9 The functional spinal segment, however, may be further divided into anterior and posterior segments. The anterior segment consists of the anterior longitudinal ligament, the vertebra, the disc, and the posterior longitudinal ligament. The anterior segment with its osseous vertebral body serves as the primary load-bearing portion of the spinal segment.1,3 The posterior segment contains the neural arch, beginning at the pedicles and extending posteriorly to the spinous process. This area is responsible for guiding and restraining the motion that occurs between the spinal segments.3 The vertebral bodies of the anterior motion segment are composed of cancellous bone, surrounded by a thin layer of cortical bone. Various studies have shown that cancellous bone contributes as much as 50% to the strength of the bone during compression. The surrounding cortical bone provides approximately 10% of the strength.1,9 As the spine progresses from C3 to L5, the size of the vertebral bodies increase in size and mass. This is an adaptation of the spine to allow for more load-carrying capacity in the lower lumbar segments. The loss of cancellous bone seen in osteoporotic patients explains the high incidence of fractures occurring with increases in compressive loads.1,3
Specific to each area of the spine are the zygapophyseal joints (Z-joints) and their orientation in space. The Z-joints are located in the posterior functional segment and restrict motion at each spinal segment. Their orientation determines the amount and direction of movement that can occur in each segment of the spine. In the cervical vertebrae (C2–7), the Z-joints are oriented 45 degrees from the horizontal axis (x axis) and parallel to the vertical axis (y axis).3,9 The exception in the cervical spine occurs with the atlas and axis, which have the Z-joints oriented nearly parallel to the horizontal axis.9 In the thoracic spine the Z-joints are oriented 60 degrees from the horizontal plane and 20 degrees from the vertical axis. The lumbar spine Z-joints are oriented 90 degrees from the horizontal axis and 45 degrees from the vertical axis. The inferior articulating processes of lumbar spine Z-joints are convex while the superior articulating processes have a concave surface.9 Articulations with the skull, ribs, and sacrum also influence motion in the spine.
The cervical spine (C3–7) can move through flexion, extension, lateral flexion, and rotation. Motion in the thoracic spine consists mostly of transverse plane rotation, lateral bending, and a smaller component of flexion and extension. The lumbar spine allows a small amount of rotation, but a much larger amount of flexion, extension, and side-bending. Slightly more rotation occurs at the lumbosacral junction due to the more obliquely oriented Z-joints at this segment.3,9 To summarize, the majority of flexion and extension occurs in the cervical, lower thoracic, and lumbar spine. The majority of rotation occurs in the upper thoracic and cervical spine, and lateral flexion is greatest in the cervical spine.3,9
The combination of the orientation of the Z-joints with the spinal curves results in ‘coupled motions’ occurring at the spinal segment.1,3,9 Assuming a neutral position, cervical lateral flexion will cause rotation of the spinous process towards the convexity of the curve. For example, cervical side-bending left causes the spinous process to rotate towards the right. The same is true in the upper thoracic spine, but not in the lumbar spine. In the lumbar spine, lateral flexion causes rotation of the spinous process towards the concavity of the curve, i.e. side-bend right, rotation of the spinous process right.1,3,9
The exceptions to this motion occur between C1 (atlas) and C2 (axis). The skull articulates with C1, which lacks a vertebral body, and because it has superiorly oriented Z-joints, it is limited to flexion and extension of approximately 10–15 degrees between the occiput (C0) and C1 and approximately 8 degrees of side-bending.3,9 There is almost no rotation at this segment. Rotation occurs at the C1–2 articulation.3,9 Approximately 40 degrees of axial rotation occurs at the C1–2 articulation. This constitutes approximately 50% of total axial plane rotation seen in the cervical spine.
The curves of the thoracic and sacral spine are fairly rigid in comparison to the more flexible curves of the cervical and lumbar spine. It is the transition points of the spine, the cervicothoracic, thoracolumbar, and lumbosacral junctions, where the spine is subjected to the greatest amount of stress. This is due to the differences in mobility that occur at these transitions.1
In general, the cervical spine demonstrates the greatest amount of range of motion in all planes and consequently is less stable and more vulnerable to injury. Also vulnerable to injury are the cervicothoracic and thoracolumbar transition regions. The combination of relatively mobile cervical and lumbar spines with the relatively immobile thoracic spine causes these transition zones to experience more torque. Because the spinal cord is located at both these levels, the potential for catastrophic spinal cord injury is of great concern.1
The biomaterial make-up of the spine is an important consideration when attempting to understand spinal biomechanics. The bony structures, especially the cancellous bone, is very strong when compressive forces are applied, while the ligaments are stronger in tension and buckle under compression.1,3,9
The ligaments of the spine provide stability and store energy during motion. The primary ligaments of the spine are the anterior and posterior longitudinal ligament, the supraspinous ligament and the interspinous ligament. These ligaments have high collagen content, whereas the ligamentum flavum has high elastin content. The capsular ligaments of the Z-joints contribute to their stability.3,9
The ligaments protect the spine by restricting motion to physiologic ranges, as well as helping to absorb external forces applied at high speeds.9 The ability of the ligaments to withstand deformation and their energy-absorbing characteristics were found to diminish with age.9 The high elastin content of the ligamentum flavum bestows a protective effect on the spinal unit. The elasticity allows for rapid flexion–extension motions and prevents permanent deformation of the ligamentum flavum, thereby limiting subsequent impingement of the spinal cord.9
When looking at injuries to the different spinal ligaments, one can identify the likely direction of the motion which caused the injury. For example, a hyperflexion motion would likely cause disruption to the supraspinous ligament. Axial rotation of the spine can cause damage to the capsular ligaments; rotation right would injure the right capsular ligament.9 The ligamentum flavum is stressed with lateral bending. If the intervertebral disc is degenerated, the ligaments are at higher risk for injury.9
The function of the intervertebral discs is to resist compression, help distribute some of the compressive load placed on the vertebral column, and to resist tensile and torsional loads as well.3,9 The disc is composed of an outer covering of fibrocartilage, the anulus fibrosus. The anulus is organized in concentric layers, with the fibers oriented ±30 degrees to the horizontal axis, and 120 degrees to the adjacent layer. The inner layers are attached to the cartilaginous endplates of the vertebral body, while the outermost layers, known as Sharpey’s fibers, attach directly to the osseous tissues. This outer vertebral attachment is stronger than the attachment to the vertebral endplate.1,3,9
The anulus fibrosus surrounds the nucleus pulposus. It is composed of glycosaminoglycans, which have a high water-binding capacity. Approximately 80–90% of the nucleus pulposus is water, which desiccates with age.10
Flexion and rotation of the spine results in tension, compression, and shear stress to the disc.9 When loads are applied slowly over a long period of time, adequate time is allowed for deformation to occur. With degeneration of the disc its viscoelastic properties are reduced, thereby decreasing its ability to absorb loads.9
Compression forces cause bulging of the discs and increased tensile stress in the anulus. Studies have shown that pure axial compression caused deformation of the disc, but no actual herniation of the disc. The vertebral endplate was more likely to fracture, with herniation of the disc into the vertebral body (Schmorl’s node).1,11
In flexion, the posterior portion of the disc is subjected to tensile stresses, while the anterior portion experiences tension while in extension. In a study evaluating disc injury, a side-bending motion with hyperflexion caused increased tension in the posterolateral aspect of the anulus, opposite to the induced side-bending; a sudden compressive load was then applied which resulted in disc prolapse in a posterolateral direction.1,9,12,13
The spine consisting only of ligaments, discs, and bony vertebrae, and absent of any musculature can only resist 20 N before collapse.1,9,14 The rib cage acts to strengthen and stiffen the spine as well as provides energy absorption during trauma.9 When the rib cage is added only 70 lb can be supported.1,9 It is the addition of the spinal musculature which provides additional strength, stability, and movement of the spine and protection from large externally applied forces (i.e. football tackles).9,15 The stability of the spine comes from the osseous and ligamentous structures, which provide a more passive stiffness, as well as the dynamic or more active stiffness provided by the muscles.16
The anteriorly located spinal flexors consist of the deeply located psoas, and the more superficial abdominal muscles: the internal/external abdominal obliques, transversus abdominis, and the rectus femoris.9,16,17 The posteriorly located spinal extensors can be divided by location into deep and superficial muscles. The deep muscles include the rotators, intertransversari, multifidi, semispinalis thoracicis, cervicis, and capitis. The superficial muscles include the more laterally located iliocostalis and the medially located longissimus and spinalis.9,16 McGill has identified the muscles attaching directly to the vertebra as most important in spinal stabilization: the multifidi, the quadratus lumborum, the longissimus and the iliocostalis. The abdominal muscles also have an important role in spinal stabilization.18
Richardson et al. have divided the muscles into either local muscles or global muscles. The local muscles act at the spinal segmental level and function as postural or segmental stabilizers. These muscles are the multifidi, quadratus lumborum, the lumbar portions of the iliocostalis and longissimus posteriorly, and the psoas, transversus abdominis, internal oblique and the diaphragm. The global muscles are dynamic and have greater torque-production capabilities. These consist of the rectus abdominis, external oblique, internal oblique (anterior fibers) and iliocostalis (thoracic portion).19
A term used often in rehabilitation of the lumbar spine is ‘core strengthening.’ This is an approach which strengthens the muscles about the spine in order to provide better dynamic stabilization, or muscular control, on the core. This core consists of the abdominals anteriorly, the paraspinals and gluteals posteriorly, the diaphragm above and the pelvic floor musculature and hip muscles below.16,19
The thoracodorsal fascia is an important structure with regards to lumbar stabilization and maintenance of correct spinal mechanics.2,16,20 This fibrous connective tissue encases the spinal extensors and is made up of three layers. These have been identified as the anterior, middle, and posterior layers. It extends inferiorly from the posterior thoracic spine, to the sacral and ilial attachments of the hip musculature. It also expands anteriorly to enmesh with the fibers of the internal oblique, and transversus abdominus, and extends superiorly to the serratus posterior inferior.2,16,20–22 The superficial laminae of the posterior layer have fibrous connections with the latissimus dorsi and the gluteus maximus. This is a key link between the upper and lower extremities.16,20,23
This posterior layer is the most important layer with regards to providing support to the lumbar spine and abdominals.16 The two lamina of the posterior layer have fibers which are directed inferiomedially and laterally. The middle and deep layers of the thoracolumbar fascia form connections with the transversus abdominus.2,16,19,20
The thoracolumbar fascia functions as a site of muscular attachment and aids in trunk rotation. It also works with the spinal ligaments to increase stiffness of the spine.20,21
The thoracolumbar fascia is not the only fascia present in the spine. The dorsal fascia of the cervical spine extends from the ligamentum nuchae, forming attachments to the spinous process of the cervical spine, with attachments made to the sternocleidomastoid, trapezius, acromion, scapular spine, and even as far anterior as the manubrium.20 This forms a functional connection between the head, neck, and shoulder girdle.20,24
The quadratus lumborum has three fascicles, the inferior oblique, superior oblique, and the longitudinal fascicles. The inferior oblique works isometrically to stabilize the spine and laterally flex the spine.16,18 The other fibers of the quadratus lumborum actually work during stabilizing the twelfth rib.16
The abdominal muscles, internal/external obliques, transversus abdominus, and rectus abdominus make up the anterior portion of the ‘core.’ The act of ‘hollowing out’ the abdomen selectively activates the transversus abdominus, while isometrically bracing the abdomen activates the transversus abdominis, and external/internal obliques. The pelvic floor muscles also fire with activation of the transversus abdominis.16,18 The rectus abdominus is activated by doing curl-ups of the trunk, and in essence flexes the lumbar spine.
The obliques work with the transversus abdominis to increase intra-abdominal pressure. The connection of these muscles with the thoracolumbar fascia, as noted previously, transfers contractile stresses in a ‘hooplike’ direction about the trunk, thereby increasing stability to the lumbar spine.16,17 The external oblique helps to prevent anterior pelvic tilt, and eccentrically controls lumbar extension and torsion.16
The diaphragm and pelvic floor serve as the roof and floor of the core, respectively. Akuthota and Nadler noted poor muscular coordination in both in those individuals with sacroiliac pain. As noted earlier, firing of the transversus abdominis also causes activation of the pelvic floor, and may be a way to improve muscular control of the pelvic floor. Instruction in diaphragmatic breathing may be a way to improve recruitment of the diaphragm.16
Regarding the cervical musculature, the muscles responsible for flexion of the cervical spine when firing bilaterally are the longus colli, scalenes, and the sternocleidomastoid. The muscles of extension, again firing bilaterally, are the splenius capitis, semispinalis capitis and cervicis. Muscles producing lateral flexion are the iliocostalis cervicis, longissimus capitis and cervices, splenius capitis and cervicis, trapezius, sternocleidomastoid, and the scalenes. Rotation is produced by the unilateral action of the rotators, semispinalis capitis and cervicis, the multifidi, and the splenius cervicis.9,24 In general, the muscles posterior to the spinal column are stronger than those located anteriorly (Table 125.1).25
Table 125.1 A summary of the cervical paraspinal muscles based on location
| Anterior cervical muscles | Posterior cervical muscles | Lateral cervical muscles |
|---|---|---|
| Longus colli | Superficial | Trapezius |
| Longus capitis | Splenius capitis and cervicis | Sternocleidomastoid |
| Rectus capitis anterior and lateralis | Longissimus capitis and cervicis | Scalenes – anterior, middle, and posterior |
| Iliocostalis cervicis | ||
| Deep | ||
| Semispinalis cervicis and capitis | ||
| Rotatores |
BIOMECHANICS OF SPINAL INJURY
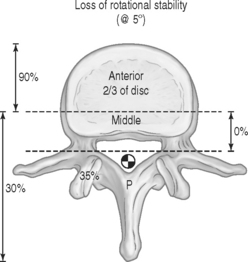
Denis derived a functional system to predict spinal vulnerability to injury. In this system, the spine is seen as divided into three columns, the anterior, middle, and posterior columns. The anterior segment extends from the anterior longitudinal ligament posteriorly through two-thirds of the vertebral body and intervertebral disc. The middle column extends from the posterior one-third of the vertebral body/discs to the posterior longitudinal ligament. The posterior segment extends from the lamina posteriorly to the spinous process.26 Haher et al. have described the contributions the columns make to resistance of axial loading and compression. If two of the three columns are disrupted, the structural integrity of the spine, specifically its ability to resist axial loading, is severely compromised by as much as 80% (Fig. 125.1).1
As much as two-thirds of the disc is located in the anterior column. This characteristic accounts for the fact that destruction of the anterior anulus can result in as much as 90% loss of rigidity or a decrease in resistance to torque (Fig. 125.2).1
Haher et al. describe the center or axis of rotation of the spine as having no anatomic location. This is because its position is not static, but instead changes depending on the motion induced. The properties of the various spinal materials, as well as pathologic changes such as fractures and ligament sprains and muscle strains, also influence and alter the location of the axis of rotation.1
Because the axis of rotation is changing on a moment-to-moment basis, Haher et al. refer to it as the ‘instantaneous axis of rotation’ (IAR).1 The location of the spinal structures in relation to the IAR determines the amount of torque these structures will produce or resist. A two-dimensional study of the location of the IAR in the cervical spine revealed its location to be anterior to the neural canal in both flexion and extension. In the lumbar spine, this was observed to be located in the inferior disc of the observed vertebra.27
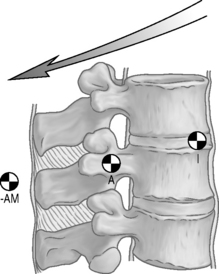
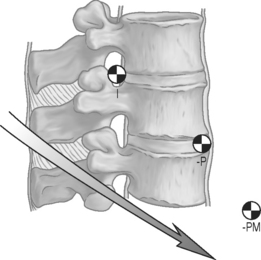
With injury to one of the columns, the IAR moves yet again. Haher et al. examined the effects of destruction of two of the three columns on the location of the IAR. Destruction of the anterior and middle column caused the IAR to move inferior and posterior with flexion (Fig. 125.3). When the posterior and middle columns were destroyed the IAR moved inferior and anterior during extension (Fig. 125.4).1
The disc has been shown to be important in resisting rotation or torsional forces, and consequently when damaged, limits the lumbar spine’s ability to resist those forces.1 Haher et al. noted the importance of the anulus to resist rotation was greater than that of the Z-joints alone.1 They also noted that damage to the posterior and middle column resulted in a loss of rotational stability of 35% while damage to the anterior column resulted in a loss of rigidity to torsion by as much as 90% (Fig. 125.2). Disc disease or damage to the structures located anteriorly would significantly alter the ability of the lumbar spine to resist torsional forces.1,28 Haher et al. also notes the importance of the disc to resist lateral flexion as well. The importance of the zygapophyseal joints seems to be in the coupled motions, which occur at the spinal segments.1
The location of the IAR and its change in position with injury to the various columns is clinically relevant. The muscles farthest from the IAR have the greatest mechanical advantage in various planes of movement. The knowledge of the IAR location as well as the anatomical location of various muscle groups can help to direct the training and rehabilitation of the spine to protect from overload of the various structures.1 Haher et al. describe the use of this knowledge in optimizing athletic performance. If spinal rotation is limited or compromised, changing an athlete’s technique may not be beneficial, while physical therapy to restore rotation would be.1
BIOMECHANICS OF SPORTS-SPECIFIC INJURIES
The cervical spine
Injuries to the cervical spine from athletic activity have been estimated to account for 5–10% of the 10 000 annual cervical spine injuries in the United States.4 Higher-risk sports are football, wrestling, gymnastics, diving, ice hockey, downhill skiing, and rugby.4,9,25
Fractures, dislocation, spinal cord injury
Cervical spine injuries can result in fracture dislocation of the vertebrae, ligament disruption, disc injury, nerve root injury, and spinal hemorrhage. Spinal hemorrhages from sports-related trauma have only been reported in the cervical spine, and not in the thoracic or lumbar spine.25 All cases of quadriplegia, without spinal stenosis, reported by the National Center for Sports Injury Research, were the result of fracture dislocation of the cervical spine.25 This fact emphasizes the need for proper on-field management of suspected cervical spine injuries in order to prevent further damage from an unstable spine.25
The predominant mechanism of cervical spine injury in American football has been identified by Torg, in conjunction with the National Football head and neck injury registry, as one of axial loading.4,5,29 Axial loading has also been implicated as the primary mechanism of injury in the cervical spine for other sports such as diving and ice hockey.5–7 In diving this generally occurs with diving in shallow water, while in hockey it often occurs with being checked from behind into the boards. Work done by other researchers evaluating the ability of hyperflexion and hyperextension movements to cause cervical spine fractures failed to show an occurrence of cervical spine fracture and dislocation.5
Axial loading occurs when a force is directed through the vertex of the head. In football, when the cervical spine is flexed 30 degrees, the energy-absorbing lordotic curve is eliminated (Fig. 125.5). The cervical spine is then unable to absorb the sudden axial load from the player in motion striking another player or object. The momentum of the player’s head must then be rapidly decelerated, while at the same time the player’s body continues its forward momentum. This results in the compression of the straightened cervical spine between the decelerated head and the forward momentum of the body. Ultimately, the cervical spine’s integrity fails, resulting in buckling of the cervical spine in a flexion direction with the end result being fracture and/or dislocation, most often at C4, C5, or C6, with subsequent spinal cord damage.4,5,9,29 The normal cervical spine can withstand loads up to 4450 Newtons before compression failure occurs.4 In 1976, rules were changed to ban the high-risk methods of spear tackling and head butting. This has decreased the incidence of quadriplegia from 35 per year to 1–6 incidents per year.4 In the rugby scrum, eight players bind together in prescribed positions to oppose an identical formation of the opposing team. In this situation, the mechanism of axial compression combined with flexion and rotation was shown to result in fracture dislocations at the C4–5 and C5–6 levels.30,31 As with football, the governing bodies of various rugby associations have made recommendations to depower the scrum and to control the point of engagement. This has resulted in decreased cervical spine injuries in the most vulnerable front row players.
The fracture pattern resulting from axial loading is one of a teardrop fragment (fracture off the anterior inferior corner of the vertebral body). Torg notes that if this fracture occurs in isolation, permanent neurologic sequelae usually do not occur. If, however, the teardrop fracture occurs with a sagittal vertebral body fracture and fractures of the neural arch, permanent neurologic involvement is often present.9,29 Initially the forces in axially loaded segments can be absorbed by the discs, vertebrae, and paravertebral muscles.29
Transient quadriplegia or cervical cord neurapraxia
Neurapraxia is a temporary paralysis which occurs after a collision with either another player or the ground. The symptoms resolve quickly, often within 10–15 minutes but occasionally as long as 24–36 hours later, but there is no residual impairment.5 The symptoms associated with this phenomenon include both sensory and motor findings. Sensory symptoms include burning pain, numbness, tingling, and loss of sensation. Motor findings can range from weakness to complete paralysis. Athletes so affected do not have cervical pain at the time of injury and radiographs are without evidence of fracture or subluxation.29
This injury has been associated with a group of athletes with developmental spinal stenosis.4,25,29 Torg et al. identified the association of cervical neurapraxia with developmental stenosis in an evaluation of 32 patients with this phenomenon; all had cervical stenosis at one or more levels.29 Herniated nucleus pulposus and spondylosis can also narrow the anteroposterior (AP) diameter of the spinal canal.
In a hyperflexion or hyperextension injury, the cord can be transiently compressed. In hyperextension the posterior inferior portion of the superior vertebral body and the lamina of the vertebra below create a ‘pincer’ effect on the cord. The same can occur with hyperflexion, although in this instance the lamina of the superior vertebra and the superior aspect of the vertebra below approximate to compress the cord.4,29,31,32
Torg et al. introduced the concept of the ‘Torg ratio’ in 1986 as a way to identify developmental stenosis. This was based on plain radiographs in which the AP diameter, measured at the midpoint of the posterior aspect of the vertebral body to the nearest point on the spinolaminar line, is divided by the sagittal diameter of the vertebral body. A ratio of 0.80 or less was considered to be a developmentally stenotic canal.33
Since the original description of the Torg ratio, studies by Cantu et al. and Herzog et al. have shown a high percentage of false-positive Torg ratios in asymptomatic football players. This was attributed to the larger vertebral bodies noted in larger athletes.34,35
The use of magnetic resonance imaging (MRI) to directly evaluate the spinal canal and available space has led to the description of functional stenosis. Cantu notes that computed tomography (CT)-myelogram or MRI can be used to assess the normal ‘functional reserve’ or the space surrounding the cord. This space contains the cerebrospinal fluid (CSF), which provides a protective cushion around the cord.34 Cantu’s use of MRI evidence of functional stenosis and increased risk of catastrophic neurologic injury has not yet been demonstrated in a population-based study. Nonetheless, it has been suggested that the presence of functional stenosis in an athlete with a prior episode of transient quadriparesis is a strong contraindication to further participation in collision sports.34,36
Researchers have also noted that in those athletes with spinal stenosis who sustained a fracture dislocation injury, there was no instance of complete neurologic recovery, while in athletes without spinal stenosis and fracture dislocation there have been instances of complete recovery.34
Spear-tacklers spine
This refers to a collection of findings, which include developmental cervical spinal stenosis, loss of cervical lordosis, and evidence of prior cervical spine injury (i.e. disc bulges/herniations, healed compression fracture and evidence of spinal instability). The combination of these findings combined with an illegal spear-tackling technique increases the risk of neurologic injury.4
Burners or stingers
Burners or stingers were thought to occur from cervical nerve root neuropraxia.4,25,37 Needle electromyographic studies have also shown injuries to the cords and trunks of the brachial plexus as well as injuries to peripheral nerves.34,38
Symptoms can include a transient occurrence of lancinating burning-type pain radiating down the involved upper extremity with or without muscle weakness. The muscles most often involved are the deltoid, biceps, supraspinatus, and infraspinatus.4,25 This can last for minutes or several days and only occurs unilaterally.4,25,37,38 This phenomenon is estimated to occur in as many as 50–65% of all college football players per year.4,37 The football players most vulnerable to burners are defensive backs.38
There are two mechanisms of injury noted. The first involves a traction injury to the brachial plexus, which usually occurs from a combination of lateral neck flexion away from the involved side and shoulder depression: for example, lateral neck flexion left with depression of the right shoulder.4,25,37,38 The second mechanism of injury involves a compression of the nerve root within the foramen, most often from the head and neck in an extended and side-bent position, while being driven down toward the ipsilateral shoulder.25,37,38 This results in pinching of the nerve root within the foramen.4,25,37,38
Levitz et al. looked at a group of athletes with chronic, recurrent burners which they defined as having ‘1) a chronic, recurrent neurapraxia or axonotmesis or both of a nerve root associated with prolonged weakness, 2) time loss from practice and games, and 3) recurrence.’37 The mechanism of injury in these individuals is one of cervical spine extension and lateral deviation towards the involved side.37
In their study, Levitz et al. also noted a high incidence of cervical canal stenosis, reversal of the normal cervical lordosis, disc disease, and foraminal narrowing secondary to osteophyte formation. They further suggest that while acute burners may well be due to a brachial plexus traction injury, chronic burners are more likely due to nerve root or dorsal ganglion compression within the foramen secondary to disc changes.37
Meyer et al. confirmed a similar finding. They noted that in athletes sustaining chronic stingers, the predominant mechanism was one of extension with lateral compression towards the ipsilateral shoulder. Their findings also demonstrated a higher incidence of cervical canal narrowing in symptomatic versus asymptomatic football players.39 The mechanism of injury for the younger player appears to be one of traction or stretch injury to the brachial plexus. In the older collegiate or professional players the mechanism is a pinching of the nerve root within the neural foramen.25,37,38
In athletes with chronic or repeated stingers, persistent proximal arm weakness and pain may develop. In these individuals the use of a cervical roll and or high shoulder pads in conjunction with retraining in proper tackling and blocking techniques should be instituted. If symptoms persist despite these interventions, a change of position or complete stoppage of play may be necessary.4,25
The lumbar spine
Low back pain in the athlete is a fairly common occurrence, with studies noting an overall incidence of low back pain in 27% of collegiate football players and 50% of football interior lineman.28,38 The lifetime incidence of low back pain in football players is 10–15% during participation years.28 In intercollegiate sports, the injury rates for low back pain over a 10-year period were highest for the sports of football and gymnastics.
Low back pain can result from muscle strains, ligament sprains, spondylolysis with or without spondylolisthesis, disc disease, radiculopathy, facet syndrome synovitis, sacroiliac joint dysfunction, and myofascial pain syndromes.38,40–42 These injuries are the result of excesses of axial compression, tension, rotational torque, or shear forces. Examples of sports involving high compressive loads are football, rugby, and weightlifting. Baseball, golf, tennis, basketball, soccer, and boxing are associated with high rotational or shear forces. Tensile or bending stresses are associated with swimming, gymnastics, and rowing.42,43
In general, hyperextension will tend to result in posterior element injury, while flexion causes increased stress to the Z-joints posteriorly or the disc anteriorly.41 Injuries to the lumbar spine can occur with acute compressive loads or with repetitive microtrauma.41,44 Lumbar strain/sprain injuries involve injury to the lumbar muscles and ligaments, respectively. These can occur from repetitive muscular contraction41 or from a sudden extension–contraction to the unprepared spine resulting in muscle and ligament disruption.40
Athletes who undergo a sudden change in training intensity or duration, or change in skill technique, may be at increased for these types of injuries.41
Fractures
Fractures of the lumbar spine are most often compression-type fractures as a result of sudden axial loading.9 This has been noted in snowmobiling and tobogganing.1,9,45 These injuries will often occur at the T12 and L1 vertebrae. In snowmobiling, these injuries have occurred following a sudden drop into a hole or hitting a bump.9,45 A burst fracture of the thoracolumbar spine can occur from a vertical impact from below.8 Compression fractures of the thoracic and lumbar spine have also occurred in football players.28
Fractures of the spinous process and transverse process can occur as well. Transverse process fractures may occur from sudden forceful contraction of the quadratus lumborum or psoas. Fracture of the spinous process may occur from a direct blow to the area.45 Both of these fractures have occurred in football players.28
Vertebral endplate fractures with subsequent herniation of the nucleus pulposus into the vertebral body may occur in the younger athlete. This is due to the relative weakness of the endplate versus the disc in the skeletally immature athlete. With a rapid compressive load, the young disc can better withstand compression than the endplate, and ultimately the endplate fails.1,9,28,40 This endplate defect is referred to as a Schmorl’s node. This can be seen in weightlifters and football players.40
Lumbar disc disease
Lumbar disc disease and herniations can occur with a flexion and lateral bending preload followed by rapid compression load.1 These types of movement can be seen in football, rugby, skiing, and weightlifting.1 Tears to the anulus without disc herniation were noted with flexion and torsion motions.1,12,41
The anterior lumbar intervertebral disc resists rotation and torque. An annular tear significantly compromises the disc’s ability to resist these motions.1,41 In sports requiring increased rotational stress, such as tennis and baseball, repetitive loading of the disc with both rotational and hyperextension motions results in fissuring and weakness of the anulus.1,41,45
Hainline describes three theories to explain lumbar disc pathology in tennis players. The first possibility involves excess fatigue in either underconditioned or overworked lumbar paraspinal muscles with subsequent transfer of kinetic stress to the ligaments. Because of the ligament’s limited ability to withstand these stresses, the loads are consequently transferred to the discs. Inadequate stability from weakened muscles and ligaments imparts an increased shearing effect on the caudal lumbar discs. The second explanation speaks to the nature of the serve, which requires repetitive rotational forces combined with hyperextension. This can result in excess annular shear forces and subsequent tears. Finally, he notes that tennis players who have experienced these injuries may have a hereditary predisposition to them.41
Football imparts a series of repetitive flexion, extension, and torsion movements coupled with axial loading moments to the lumbar spine.28 A study of interior lineman showed higher levels of disc degeneration compared to other positions.28 Gatt et al. studied offensive lineman while they were hitting a blocking sled, and evaluated loads at the L4–5 segment. The blocking sequence imposes compression, shear, and lateral bending forces to the lumbar spine. The Gatt et al. study found extraordinary compressive forces averaging 8679 N±1965 N.28,46
To reiterate, the lumbar disc is the prime stabilizer to rotational forces and is more important than the Z-joint in resisting rotation. Damage to the lumbar disc compromises its ability to resist rotation, leading to instability as well as placing more weight-bearing load on the Z-joints.1,27,41
Spondylolysis
Spondylolysis is a defect of the pars interarticularis, either congenital or acquired.28,38,40,44,47,48 Higher rates of spondylolysis have been noted in gymnastics, football, power/weightlifting, tennis, figure skating, and hockey,38,47,48 while another study reported higher rates occurring in weightlifting, judo, rugby, and football.43 The incidence of spondylolysis has been estimated to be 3–6% in the general population,38,47,48 with males affected 2–3 times as often as females.48 As well, higher incidences are noted in athletes overall.47,48 In football 15% of high school and college players had spondylolysis, while interior lineman had incidence rates as high as 50%.28
While this defect was initially thought to be congenital, current theory now is one of acquisition from either a single sudden overload event or more commonly with repetitive loading.45,47,48 It is felt by many that the repetitive demands of various sporting activities places increased stress on the lumbar spine, thereby causing the higher rates of spondylolysis seen in athletes.44,47–49
The mechanism of repetitive lumbar flexion and extension causes excess load at the L5–S1 level with stresses greatest at the pars interarticularis.28,47,48 It is this repetitive loading which makes the pars more vulnerable to fatigue fractures under lower loads.47,48 The L5 vertebra is the most common level to sustain a spondylitic defect, with 85–95% off defects occurring at this level. The L4 level sustains 5–15% of such defects.47,48
Spondylolisthesis
Spondylolisthesis is defined as a sagittal plane translation of one vertebra over another. Anterolisthesis and retrolisthesis are terms frequently used to describe the direction of slippage of the superior vertebral body relative the one immediately below. It most often occurs at the L5–S1 junction and is a result of the loss of continuity of an intact pars articularis or a bilateral spondylolysis.9,38,40
The mechanism most often attributed to the development of spondylolisthesis is a fatigue fracture or stress fracture occurring bilaterally at the pars interarticularis with resultant forward slippage of the superior vertebra on the one below. The risk of progression of forward slippage has been studied and has been noted to be fairly small. In a study of 47 patients under the age of 16 with either symptomatic spondylolysis or spondylolisthesis over a 7-year period, only two individuals had a slip progress to more than 20%. Various studies of adolescents have shown the percentage of slip progression greater than 20% was 3–4% in these individuals with spondylolysis or low-grade spondylolisthesis.48 Also of note was that the increased tendency towards forward slippage was greatest in adolescents during their growth spurt. No specific increased risk for slip progression was noted with sports participation.48
The body mechanics associated with spondylolysis and spondylolisthesis is one of hyperlordosis in the lumbar spine with excessively tight hamstrings.28,48 Increased lumbar lordosis has been associated with tight hip flexors, tight thoracolumbar fascia, thoracic kyphosis, weak abdominals, and genu recurvatum.28,49
In general, injuries to the lumbar spine can occur from 1 of 3 forces occurring either alone or in combination. These are compression, tension, or torque (either shear or rotational).40,42 Compression or axial loading can lead to vertebral endplate fracture or ultimately vertebral body compression fracture. Sports associated with these forces are football and weightlifting.50,51 Running has been shown to produce compressive forces sufficient to decrease intervertebral disc height. Because the lumbar discs are dynamically loaded during running the decrease in disc height is greater than with static loading.52
Axial loading in combination with hyperextension places increased shear stress on the posterior elements, ultimately leading to a higher risk of spondylolysis and spondylolisthesis.40,42,47 Sports associated with these motions are football (offensive linemen),28,40,42,43,47,48 gymnastics,40,42,44,48,49 weightlifting, diving, volleyball,40,42,49 the throwing field events of track and field,40 high jumping, and pole vaulting.40
Rotational forces are associated with baseball and softball batting, throwing, golf, and tennis.2,20,40,42,43 Rotation forces initially place increased stress on the disc, but with continued rotation this shifts to the Z-joints.42
SUMMARY
Prevention and rehabilitation of spinal injuries involve application of these principles to the rehabilitation program. For example, restoration or correction of normal spinal curves helps the spine to absorb and disperse loads.4,5,9 Therefore, prior to return to play from an injury, athletes with cervical spine injuries should have restoration of normal cervical lordosis.4 Correction of hyperlordosis in the lumbar spine by addressing lack of flexibility in the hip flexors, thoracolumbar fascia, and weakness of the abdominal muscles can help prevent additional overload of the posterior elements.28 Proper strengthening of the cervical spine via cervicothoracic stabilization is important in both the rehabilitation and prevention of cervical spine injuries. These include scapular stabilization exercises as well as strengthening of the cervical intrinsic musculature.4,53
Strengthening of the trunk, lumbar spine, hip girdle muscles, and the lower extremity is important to ensure the transfer of forces from the lower extremities through the lumbar spine. Moreover, it prevents overload of structures due to a weak link in the kinetic chain. Core strengthening for sporting activities should involve training in three planes: sagittal, frontal, and transverse.16 Triplanar core strengthening accomplishes more than just simple muscular strengthening, but involves muscle reeducation, improvement of muscular endurance, and improvement in balance and proprioception.16
Finally, coaches and physicians should work together to instruct athletes on safe training techniques and proper skill mechanics in order to prevent injury, enhance performance, and prolong playing careers. When necessary, physicians should work with sporting officials and governing bodies to implement rules changes to decrease injury to players. This has helped to dramatically decrease the number of spinal cord injuries seen in football29 and rugby.6,7,30,31
1 Haher TR, O’Brien M, Kauffman D, et al. Biomechanics of the spine in sports. Clin Sports Med. 1993;12:449-464.
2 Young JL, Casazza BA, Press JM, et al. Biomechanical aspects of the spine in pitching. In: Andrews JR, Zarins B, editors. Injuries in baseball. Philadelphia: Lippincott-Raven; 1998:23-35.
3 Wells MR. Biomechanics: an osteopathic perspective. In: Ward RC, et al, editors. Foundations for osteopathic medicine. 2nd edn. Philadelphia: Lippincott Williams & Wilkins; 2003:63-89.
4 Kim DH, Vaccaro AR, Berta SC. Acute sports-related spinal cord injury: contemporary management principles. Clin Sports Med. 2003;7:22.
5 Torg JS, Vegso JJ, O’Neill J, et al. The epidemiologic, pathologic, biomechanical, and cinematographic analysis of football-induced cervical spine trauma. Am J Sports Med. 1990;18:50-57.
6 Wetzler MJ, Akpata T, Albert T, et al. A retrospective study of cervical spine injuries in American rugby, 1970–1994. Am J Sports Med. 1996;24:454-458.
7 Wetzler MJ, Akpata T, Laughlin W, et al. Occurrence of cervical spine injuries during the rugby scrum. Am J Sports Med. 1998;26:177-180.
8 Sances A, Myklebust JB, Maiman DJ, et al. The biomechanics of spinal injuries. Crit Rev Biomed Eng. 1984;11:1-76.
9 White AA, Panjabi MM. Clinical biomechanics of the spine, 2nd edn. Philadelphia: Lippincott Williams & Wilkins, 1990.
10 Panagiotacopulos ND, Pope MH, Block R, et al. Water content in human intervertebral discs, Part II. Viscoelastic behavior. Spine. 1987;12:918.
11 Hochschuler S. The spine in sports. Philadelphia: Hanley and Belfus, 1990.
12 Adams M, Hutton WC. The relevance of torsion to the mechanical derangement of the lumbar spine. Spine. 1981;6:247-248.
13 Adams MA, Hutton WC. Prolapsed intervertebral disc. A Hyperflexion injury. Spine. 1982;7(3):184.
14 Crusco JJ, Panjabi MM. Euler stability of the human ligamentous lumbar spine. Part 1 Theory. Clin Biomechan. 1992;7:19-26. Part II, Experiment. 1992;7:27-32.
15 Granata KP, Orishimo KF. Response of trunk muscle coactivation to changes in spinal stability. J Biomechanics. 2001;34:1117-1123.
16 Akuthota V, Nadler SF. Core strengthening. Arch Phys Med Rehab. 85(Suppl 1), 2004.
17 McGill SM. Low back disorders: evidence based prevention and rehabilitation. Champaign, IL: Human Kinetics, 2002.
18 McGill SM. Low back stability: from formal description to issues for performance and rehabilitation. Exerc Sport Sci Rev. 2001;29(1):26-31.
19 Richardson C, Jull G, Hodges P, et al. Therapeutic exercise for spinal segmental stabilization in low back pain; scientific basis and clinical approach. Edinburgh: Churchill Livingstone, 1999.
20 Young JL, Herring SA, Press JM, et al. The influence of the spine on the shoulder in the throwing athlete. J Back Musculoskel Rehab. 1996;7:5-17.
21 Bogduk N, Anat D, Macintosh JE. The applied anatomy of the thoracolumbar fascia. Spine. 1984;9:164.
22 McGill SM, Norman RW. Potential of lumbodorsal fascia forces to generate back extension moments during squat lifts. J Biomed Eng. 1988;10:312-318.
23 Vleeming A, Pool-Goudzwaardmaard AL, Stoeckart R, et al. The posterior layer of the thoracolumbar fascia. Its function in load transfer from spine to legs. Spine. 1995;2:753-758.
24 Moore KL. Clinically oriented anatomy, 3rd edn., Baltimore, MD: Williams & Wilkins; 1992:323-372.
25 Proctor MR, Cantu RC. Head and neck injuries in young athletes. Clin Sports Medicine. 2000;19(4):693-715.
26 Denis F. The three-column spine and its significance in the classification of the acute thoracolumbar spinal injury. Spine. 1983;8:817-831.
27 Haher T, Bergman M, O’Brien M. Effect of 3 columns on the instantaneous axis of rotation in flexion and extension. Spine. 1991;16:312-318.
28 Gerbino PG, d’Hemecourt PA. Does football cause an increase in degenerative disease of the lumbar spine. Curr Sports Med Rep. 2002;1:47-51.
29 Torg JS, Thibault L, Sennett B, et al. The pathomechanics and pathophysiology of cervical spinal cord injury. Clin Orthopaed Rel Res. 1995;321:259-269.
30 Milburn PD. Biomechanics of rugby union scrummaging. Sports Med. 1993;16:168-179.
31 Silver JR, Stewart D. The prevention of spinal injuries in rugby football. Paraplegia. 1994;32:442-453.
32 Silver JR. Injuries of the spine sustained during rugby. Br J Sports Med. 1992;26:253-258.
33 Torg JS, Pavlov H, Genuario SE, et al. Neurapraxia of the cervical spinal cord with transient quadriplegia. J Bone Joint Surg [Am]. 1986;68(13):54-70.
34 Cantu RC. Stingers, transient quadriplegia, and cervical spinal stenosis: return to play criteria. Med Sci Sports Exerc. 1997;29(Suppl 7):S233-S235.
35 Herzog RJ, Wiens JJ, Dillingham MF, et al. Normal cervical spine morphometry and cervical spinal stenosis in asymptomatic professional football players. Spine. 1991;16(Suppl 6):S78-S86.
36 Cantu RC. The cervical spinal stenosis controversy. Clin Sports Med. 1998;17:121-127.
37 Levitz CL, Reilly PJ, Torg JS. The pathomechanics of chronic, recurrent cervical nerve root neurapraxia. The chronic burner syndrome. Am J Sports Med. 1997;25:1.
38 Sherman AL, Young JL. Musculoskeletal rehabilitation and sports medicine. Head and spine injuries. Arch Phys Med Rehab. 1999;80:S40-S49.
39 Meyer SA, Schulte KR, Callaghan JJ, et al. Cervical spinal stenosis and stingers in collegiate football players. Am J Sports Med. 1994;22:158-166.
40 Alexander MJL. Biomechanical aspects of lumbar spine injuries in athletes: a review. Can J Appl Sport Sci. 1985;10(1):1-20.
41 Hainline B. Low back injury. Clin Sports Med. 1995;14:241-265.
42 Montgomery S, Haak M. Management of lumbar injuries in athletes. Sports Med Feb. 1999;27:135-141.
43 Ichikawa N, O’Hara Y, Morishita T, et al. An aetiological study on spondylolysis from a biomechanical aspect. Bri J Sports Med. 1982;16:135-141.
44 Hall SJ. Mechanical contribution to lumbar stress injuries in female gymnasts. Med Sci Sports Exer. 1986;18:599-602.
45 Bowerman JW, McDonnell EJ. Radiology of athletic injuries – football. Radiology. 1975;117:33-36.
46 Gatt CJ, Hosea TM, Palumbo RC. Impact loading of the lumbar spine during football blocking. Am J Sports Med. 1997;25:317-319.
47 Letts M, Smallman T, Afanasiev R, et al. Fracture of the pars interarticularis in adolescent athletes: A clinical-biomechanical analysis. J Pediatr Orthoped. 1986;6:40-46.
48 Standaert CJ, Herring SA. Spondylolysis: a critical review. Br J Sports Med. 2000;34:415-422.
49 Gerbino PG, Micheli LJ. Back injuries in the young athlete. Clin Sports Med. 1995;14:3.
50 Garbutt G, Boocock MG, Reilly T, et al. Physiological and spinal responses to circuit weight training. Ergonomics. 1994;37(1):117-125.
51 Granhed J, Jonson R, Hansson T. The loads on the lumbar spine during extreme weight lifting. Spine. 1987;12:146-149.
52 Ahrens SF. The effect of age on intervertebral disc compression during running. JOSPT. 1994;20:1.
53 Cross KM, Serenelli C. Training and equipment to prevent athletic head and neck injuries. Clin Sports Med. 2003;22:3.