CHAPTER 49 Biomechanics and Assessment of the Painful Shoulder
INTRODUCTION
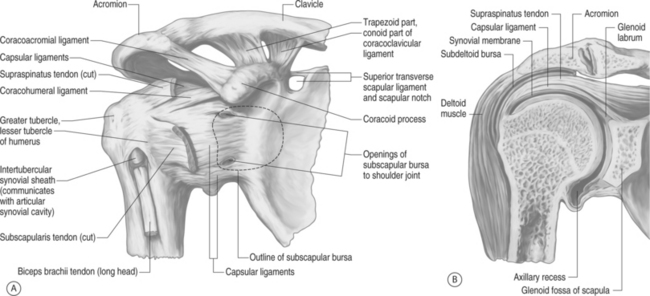
Spinal pain itself is complex in nature. To add another dimension to the diagnostic dilemma, the shoulder itself is among the most complex of all the body’s joints (Fig. 49.1). The shoulder is composed of four joints: the glenohumeral (GH), the acromioclavicular (AC), the sternoclavicular (SC), and the scapulothoracic (ST). It entails anywhere from 22 to 26 individual muscles and/or muscle slips, which are utilized for a combination of stability, power, and control of elevation and rotation. The shoulder is unique in that it is highly mobile, with an estimated 16 to 17 thousand positions in which the upper extremity may be placed, while necessarily exhibiting a concurrent lack of bony stability. The arm can move through approximately 180 degrees in elevation, 150 degrees of internal and external rotation, and flexion and extension or anterior and posterior rotation in the horizontal plane of approximately 170 degrees.1 The very interaction of the musculature both as agonist and antagonist must be coordinated for even the simplest motions in order for there to be an effective movement. An understanding of the anatomy and biomechanics of the shoulder is essential for clinicians who treat spinal disorders, as well as for other orthopedic practitioners.
ANATOMY
Sternoclavicular joint
Four ligaments and an intra-articular disc stabilize the sternoclavicular joint, which is mobile about all three axes (x, y, and z planes). The interclavicular ligament provides restraint to medial clavicular motion superiorly. It interconnects one medial clavicle to the other medial clavicle via its attachment to the sternum. However, this ligament may be absent or nonpalbable in 22% of individuals.2 The interclavicular ligament is taut when the arm is brought to the side. There are anterior and posterior capsular structures that prevent motion in the anterior and posterior planes; of the two, the anterior is the stronger restraint. The costoclavicular ligaments, which run obliquely and laterally from the first rib to the clavicle, provide for stabilization inferiorly. The posterior capsular structure is the strongest stabilizing force that resists downward motion, and the anterior structure resists superior motion of the medial clavicle.
Glenohumeral joint
The glenohumeral joint is what the layman and many in the healthcare field think of as the ‘shoulder joint.’ Although this joint is considered a ball (humerus) and socket (glenoid) joint, the socket covers only one-quarter of the humeral head.3–5 This ratio was initially calculated by the following simple formula, known as the glenohumeral index:
Maximum diameter of the glenoid:maximum diameter of humeral head
Saha recalculated the ratio to 0.6 in the transverse plane and 0.75 in the sagittal plane.6 Maki and Gruen further refined the ratio to 0.58 and 0.86 in a presentation to the Orthopedic Research Council in 1976.
Three different types of glenohumeral articulations have been identified, and in each case the humeral head is classified as being smaller, equal to, or larger than the radius of curvature of the glenoid.6,7 This difference is believed to impact a variety of shoulder instability patterns. A smaller glenoid surface diameter is necessarily a smaller effective contact surface for the humeral head and is thus a more unstable configuration.6,8,9 In the coronal plane, the articular surface of the glenoid comprises an arc of approximately 75 degrees, whereas the articular surface of the humeral head is roughly 120 degrees, or one-third of a sphere.
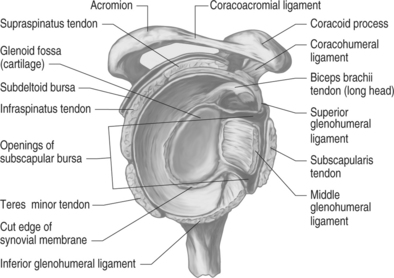
The glenoid labrum increases coverage about the humeral head by nearly 100%, and doubles the depth.10 The glenoid labrum is composed of dense fibrous connective tissue, and serves not only to increase the surface area and depth of the glenoid, but also to increase the structure’s load-bearing ability.11 The labrum is a structure which appears to be fibrocartilagenous in structure when examined superiorly but, as one approaches the inferior surface, is almost capsular in appearance. There are wide variations in labral anatomy among individuals, and there is no correlation between labral depth and glenoid size. Two aspects of labral anatomy that are fairly consistent are that the most stable, largest portion is the anterior and inferior area, and that the labrum itself acts to physically double the depth of the socket for the humeral head.
The glenohumeral joint allows for three distinctly different types of motion: spinning, sliding, and rolling. Spinning is when the contact point on the glenoid remains the same, but the contact point of the humeral head is changing. Sliding occurs when the contact point on the glenoid is changing, but that of the humerus remains the same. This generally occurs in unstable joints, and in extremes of motion in normal joints. The third type of motion, rolling, is when the contact points on both the glenoid and humeral head change.12
Anatomically, the proximal humerus is separated into four parts: the articular surface, the greater tuberosity, the lesser tuberosity, and the diaphyseal shaft. In relation to the shaft, there is a 45-degree medial angulation to the humeral head, and a 30-degree retroversion relative to the transcondylar axis of the distal humerus. The intertubercular groove lies between the greater and lesser tuberosities, and it is here that the tendon of the long head of the biceps lays.13 This tendon is held in place not only by the coracohumeral ligament, but also by the transverse humeral ligament. During shoulder abduction, the humeral head slides on this tendon. If the biceps tendon should rupture, anterior translation of the humeral head is subsequently increased.14
Utilizing an elegant approach, Johnson noted in 1937 that in order for the upper limb to maximally elevate, the humerus must externally rotate.15 Initially, research pointed to a physical obstruction caused by the coracoacromial arch to the greater tuberosity of the humeral head. By 1976, it was realized that this movement provides for loosening of the inferior ligaments of the glenohumeral joint while simultaneously allowing for optimal articulation with the glenoid.16 Thus, full arm elevation combined with external rotation is a position of greater stability than full elevation alone. This is due to a combination of relative laxity and stability of the three glenohumeral ligaments, intrinsic muscular forces, and negative intracapsular pressure.17
The ligamentous restraints of the glenohumeral joint are the inferior glenohumeral ligament (IGHL), the middle glenohumeral ligament (MGHL), and the superior glenohumeral ligament (SGHL) (Fig. 49.2). These glenohumeral ligaments, which insert onto the glenoid labrum and humeral neck, have often been described as ‘capsular thickenings.’15 This ‘capsular-ligamentous’ complex is the major static stabilizer of the shoulder, and although all of the ligaments are necessary for proper function, the IGHL is the most essential component of this complex. Studies have shown that the shoulder joint capsule possesses greater elasticity and twice the strength of that of similar structures within the elbow.19 The superior, middle, and inferior glenohumeral ligaments are considered the anterior glenohumeral ligaments.
The coracohumeral ligament, which runs laterally from the coracoid process to insert upon the superior–anterior aspect of the humeral head, is the most consistent of the ligaments of the shoulder capsule.20 In addition to providing an anterior stabilizing force to the biceps tendon, it also renders stability to the shoulder, particularly when the arm is in the dependent position.21
The superior glenohumeral ligament lies beneath the coracohumeral ligament, and has been found to contribute little to the stability of the glenohumeral joint. It also is a relatively constant structure, and arises from the tubercle of the glenoid, inserting upon the lesser tuberosity of the proximal humerus. The long head of the biceps tendon originates posteriorly to the SGHL. In concert with the superior tilt of the glenoid, the SGHL provides passive resistance to inferior subluxation and dislocation of the humerus.22
The middle glenohumeral ligament exists underneath the subscapularis muscle, and its presence is the most variable of the glenohumeral ligaments.20 Its origin is at the supraglenoid tubercle at the superior glenoid and anterior superior labrum, and inserts with the subscapularis muscle at the lesser tuberosity of the humerus. This ligament provides the majority of resistance to anterior humeral head displacement.20,23 It may measure up to 2 cm wide, and as much as 4 mm in thickness.24
The thickest of the glenohumeral ligaments is the inferior glenohumeral, which originates from most of the anterior glenoid labrum, and inserts on the inferior margin of the humeral head articular surface. The IGHL is the main static stabilizer in the abducted arm, and it reinforces the inferior capsule.25,26
A fundamental knowledge of the anatomy of the IGHL is instrumental in understanding the pathophysiology behind recurrent anterior humeral dislocation. When the humeral head dislocates in an anterior direction, the associated detached bone–labral complex essentially renders the IGHL an incompetent structure. The IGHL is composed of an anterior and posterior band with an axillary pouch in between.27 The anterior band serves as the major stabilizer of the glenohumeral joint when the arm is in abduction and external rotation.25 In this position, the anterior band appears to fan out, while the posterior band becomes cordlike. With the arm in internal rotation, the anterior band becomes cordlike, while the posterior band spreads into a fan shape to support the joint.
Codman’s paradox
While seated or standing, have the arm resting at the side with the medial epicondyle of a flexed elbow facing the midline of the trunk; take the arm to a position flexed forward to 90 degrees. Next, abduct the arm 90 degrees so that the epicondyle is then pointing perpendicular to the coronal plane. Then, bring the arm back to the side to its initial position. After performing these motions, the medial epicondyle is no longer facing medially towards the trunk, but is rather rotated away from the body in an ‘anterior’ position all without the humerus ever being actively axially rotated.15
Discussions have abounded surrounding this concept. It has been noted that the angular rotations involved with this movement do not add up to the concluding position, and that they are thus sequence dependent. The sequence of these complex rotations is what allows this phenomenon to occur. In aerospace terminology, these rotations are called the ‘Eulerian angles’ of yaw, pitch, and roll.10
Scapulothoracic joint
The scapulothoracic joint can be thought of as the base that stabilizes the shoulder girdle. Jobe and Pink28 have likened it to a seal balancing a ball on its nose. If that seal is able to stand still it can balance a ball for a lengthy time; however, if the seal is unable to obtain a stable position the ball will fall. This basic premise of strength at the base of the shoulder or core stabilization as referred to in spine rehabilitation is quite similar and will be discussed later. As noted above, the only bony attachment site of the scapula to the axial skeleton is at the acromioclavicular joint. Therefore, it is the muscular attachments, the scapulothoracic muscles, that are referred to as the scapular stabilizers. It is these muscles that act to position the scapula to the proper orientation on the thoracic cage for a given shoulder motion. These muscles include the trapezius, levator scapulae, serratus anterior, pectoralis minor, and rhomboids (major and minor). Shoulder abnormalities can stem from weakness or tears of one or all of these muscles. Disorders may also result from neuropathic abnormalities such as entrapment of the suprascapular nerve or compression of the dorsal scapular or long thoracic nerve, resulting in neuropraxia, neurotmesis, or axonotmesis. Space-occupying masses such as cysts or tumors as well as arthritic spurs and bony deformity in the glenohumeral joint can also result in abnormalities of function of the scapular stabilizers and hence the scapulothoracic joint.
BIOMECHANICS
The relative motion between the scapulothoracic articulation and the glenohumeral joint during shoulder abduction is termed the scapulothoracic rhythm.17,29–31 Over the entire arc of abduction, the glenohumeral joint moves more than the scapulothoracic joint; however, this difference is large at the beginning of abduction, and minimal at the end range of motion. Glenohumeral motion is much greater than scapulothoracic motion for the first 30 degrees of abduction; this ratio has been reported as ranging from 4:1 to 7:1.16,32 Over the subsequent 30–180 degrees of shoulder abduction there is less asymmetry between glenohumeral motion and scapulothoracic motion, and the ratio is then closer to 5:4.
The arc of full arm elevation involves anterior rotation of the scapula by about 6 degrees, with subsequent posterior rotation of the scapula on the order of 16 degrees until the arm is at its final resting position. That is, 10 degrees posterior to it’s starting position.33 In addition to these movements, there is also a simultaneous forward tilt of the scapula by 20 degrees.10,34
The articulation of the humeral head with the glenoid portion of the scapula was found by Saha6 to be posteriorly oriented by an average of 7 degrees in relation to the body of the scapula. This apparently minor retroversion is thought to be an important element of the static restraint system. It has been clinically correlated that those individuals with less retroversion have a greater tendency towards recurrent anterior dislocation at the glenohumeral joint. While there is agreement that there is a wide array of the amount of retroversion within individuals, there is still no consensus with regards to the clinical relevance, or in research with regards to these variations and their part in instability of the joint.
Resting muscle tension appears to account for much of the stability about the shoulder girdle. The base of the shoulder girdle is the scapula, and three groups of muscles concordantly maintain its stability: the posterior, intrinsic, and extrinsic groups.35 The scapulohumeral stabilizers comprise the posterior group of muscles, consisting of the trapezius, levator scapulae, rhomboids, and serratus muscles. This group helps to provide a stable base of rotation for glenohumeral motion, and maintains the glenoid in a position of maximal congruency with the humeral head, thus maintaining the proper length–tension relationship of the glenohumeral musculature.36,37 The intrinsic groups of muscles are the glenohumeral stabilizers and include the rotator cuff musculature: the supraspinatus, infraspinatus, teres minor, and subscapularis. Dynamic stability about the shoulder is dependent upon muscular forces generated by these muscles and those surrounding the scapulothoracic joint.38 The deltoid is the primary muscle of the extrinsic group, with biceps and triceps being secondary extrinsic muscles. These muscles comprise the primary positioners of the humerus and forearm.38
Inman and associates first described the concept of a ‘force couple’ in 1944.13 They described the dynamics of multiple forces passing across and through the shoulder during active motion to allow for any desired arm position. For example, their theory noted that if the deltoid were to pull the humerus superiorly, then the subscapularis, infraspinatus, and teres minor would act as a single functional unit to counteract any shearing forces that the deltoid placed upon the glenohumeral joint. This would then allow the humeral head to maintain itself in a congruent alignment to the glenoid by simultaneously depressing the humeral head and allowing the head to rotate about the glenoid.
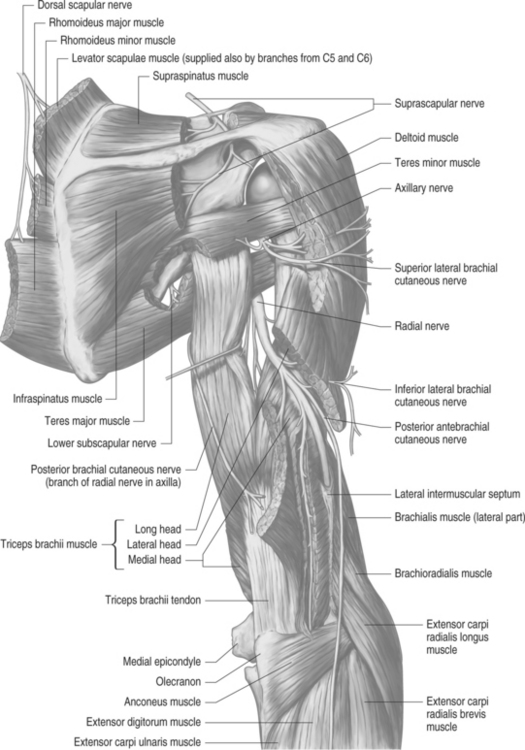
NERVE SUPPLY
Innervation of the shoulder complex (Fig. 49.3) is mainly via the C5 through C7 nerve roots, via the brachial plexus. Because of its proximity to many bony structures, the great mobility about the shoulder and neck, and superficial location, the brachial plexus is particularly susceptible to traumatic injury.39 The branches that come off of the lateral cord of the brachial plexus, the lateral pectoral nerve and musculocutaneous nerve, are those that are most essential to shoulder function. The musculocutaneous nerve passes through the coracobrachialis muscle, several centimeters below its insertion when leaving the axilla.40
The upper and lower subscapular nerves are also important branches off the posterior cord of the brachial plexus with regards to innervation of the subscapularis muscle. Also from the posterior cord arises the thoracodorsal nerve (also known as the middle subscapular nerve), which supplies the latissimus dorsi, and travels along the lateral border of the scapula.40
The axillary nerve, after obtaining its contributions from the C5 and C6 nerve roots, travels along the inferior portion of the subscapularis muscle, and is a large terminal branch of the posterior cord of the brachial plexus. It winds around the surgical neck of the humerus to supply the teres minor and deltoid muscles, and terminates as the upper lateral brachial cutaneous nerve and supplies skin sensation over the inferior half of the deltoid and adjacent areas of the arm.38 This intimate association with the humeral neck places the axillary nerve in a potentially compromising position, as it is susceptible to injury from trauma to the area or from surgical procedures about the shoulder.41
The suprascapular nerve, after receiving its innervation from the C5 and C6 nerve roots from the upper trunk of the brachial plexus, travels along the superior border of the scapula in the suprascapular notch, eventually supplying the supraspinatus and infraspinatus muscles. The transverse scapular ligament is a potential entrapment site and may compress the suprascapular nerve as it crosses through the scapular notch.40
The innervation of the glenohumeral joint is mainly from the axillary nerve, suprascapular nerve, and the lateral pectoral nerves.42
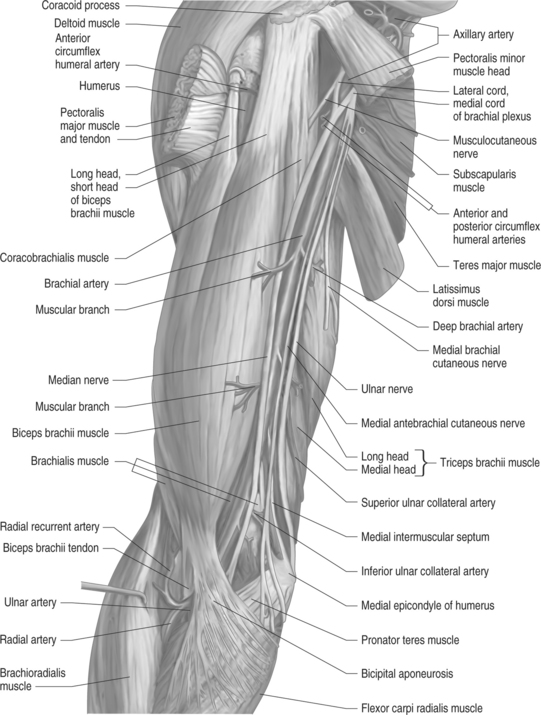
VASCULAR SUPPLY
The arterial supply of the entire upper limb comes from the subclavian artery, which becomes the axillary artery after crossing the first rib, and continues into the arm as the brachial artery (Fig. 49.4).43 The axillary artery extends between the first rib and the lower border of the teres major muscle, and gives off branches to the thoracic wall and its covering muscles, as well as to the shoulder and upper part of the arm. There are six named branches off of the axillary artery.43
Venous drainage is mainly by the axillary vein, which is joined by the cephalic vein, lying between the deltoid and pectoralis major muscles, and two brachial veins. The upper end of the cephalic vein is the only superficial vessel of any size in the shoulder region.43
Many anatomic variations may be found at the cervicothoracic junction, some which can compress neurovascular structures to generate a variety of thoracic outlet syndromes (TOSs).39 There are three distinctly different pathophysiologic types of thoracic outlet syndrome.44 The most common type of TOS may also be referred to as costoclavicular syndrome, and presents without neurologic or vascular anomalies, but with symptoms of pain and/or paresthesias in the arms. The symptomatology is felt to be a direct result of brachial plexus compression between the clavicle and a normal first rib.39 A second type of TOS is neurologic TOS, in which weakness and sensory deficits stem from stretch and/or compression of the lower trunk of the brachial plexus. Some anatomic variations that may be responsible for the neurologic TOS are an accessory cervical rib with or without an associated fibrous band, an enlarged cervical transverse process, an abnormal first rib, hypertrophy of the anterior scalene muscle (termed scalenus anticus syndrome), and hyperabduction syndrome.4 The third type of TOS is vascular, and consists of narrowing of the subclavian artery as it angles over the first rib in patients with a well-developed cervical rib. In this case there are often signs of vascular compromise such as intermittent blanching of the fingers or entire hand, and rarely, frank ischemia, and gangrene. Neurologic symptoms should be absent in this purely vascular type of TOS.39
Rarely, Doppler ultrasound and duplex scanning can indicate that subclavian artery compression by the scalene muscles is the etiology of early fatigue, arm heaviness, and hand coldness in the upper extremity of well-conditioned athletes.45,46 When the shoulder is positioned in abduction and external rotation, these findings can be elicited in many asymptomatic individuals, as well as overhead athletes; therefore, this test is not considered specific. This is the basis behind ‘Adson’s maneuver,’ in which the examiner externally rotates and extends the patient’s test arm while palpating the radial pulse. The patient then extends and rotates the neck towards the test arm and takes a deep breath. Absence or diminishing radial pulse is felt to indicate vascular TOS caused by compression of the subclavian artery by the scalene muscles. As mentioned above, this test is non-specific and is thought to have a greater than 50% incidence of false positivity.47–49
Occasionally, symptoms may result from a subclavian artery aneurysm with thrombosis. In this case, embolization to the hand with severe ischemia may result.46 Compression of the axillary, posterior humeral circumflex, suprascapular, or subscapular arteries may all result in similar, localized symptoms.46
ASSESSMENT
Several authors have reported an approximately 5% incidence of pain referable to the cervical spine in patients presenting with shoulder pain.50–54 Slipman et al. reported of a case of extrinsically induced pain that included symptoms that all pointed to an intrinsic cause of pain. Despite diagnostic work-up for both shoulder and cervical spine etiologies, all signs pointed to an intrinsic pathology, but arthroscopic findings were minimal and postoperatively there was no change in symptoms. Repeat diagnostic studies of the cervical spine were performed and there was no change from the initial findings. A diagnostic selective nerve root block was then performed, providing complete relief of pain and immediate return of full range of motion.55 This case helps to illustrate that even though the entire work-up may point toward one etiology, when evaluating nonacute presentations of pain, perseverance may be needed to correctly diagnose and adequately treat the condition, and a referal for ‘chronic pain management’ may be premature.
In those patients with chronic shoulder symptoms, the history may be less helpful for several reasons. The duration of symptoms may lead to some forgetfulness on the part of the patient, blurring memory of some of the initial symptoms and treatment as well as other associated medical maladies at the onset. As noted above, loss of range of motion of the shoulder girdle, primarily at the glenohumeral joint, typically happens since the arm tends to be held in a pain-free, dependent position, mainly at one’s side. This lack of glenohumeral mobility demands an alteration of the basic biomechanics of the shoulder. The patient will have to substitute another aspect of the shoulder complex to allow overhead or other reaching motions. Typically, a greater contribution from the scapulothoracic joint is needed to achieve the elevation required to perform even simple activities of daily living.56
This alteration in the pattern of movement of the shoulder will therefore require an increase in contribution from the joints adjacent to the shoulder girdle proper. Whether there is a substitution pattern of the adjacent musculature, or if greater motion of the elbow is required to place the upper limb in a desired position, an increase in stress to these regions will lead to associated symptoms such as an epicondylitis of the elbow as the problem progresses.
Abnormalities seen on radiographic evaluation, as well as bone or soft tissue masses found clinically, need to be evaluated in a methodical and well-organized fashion.57 Both benign and malignant tumors may be found in and about the shoulder complex. The goals in treatment of malignant tumors are, in order of priority, preservation of life, limb, and function.57 Benign tumors found about the shoulder include osteoid osteoma, osteoblastoma, osteochondroma, enchondroma, giant cell tumors, chondroblastoma, eosinophilic granuloma, and synovial osteochondromatosis57. Malignant tumors include osteosarcoma, chondrosarcoma, Ewing’s sarcoma, and myeloma.57 In addition to malignant and benign tumors, there may also be various tumor-like conditions associated with the shoulder, such as aneurysmal bone cyst, simple bone cyst, fibrous dysplasia, and Paget’s disease of the bone.57
The assessment itself then turns to the physical examination. While no human is perfectly symmetrical, we do look for side-to-side differences in muscle mass, height and angulation of the shoulder, and motion of the scapula and arm during both passive and active range of motion. Watching the scapula itself is a superb way to evaluate for subtle pathologic findings. We observe not only the rotation of the scapula (rhythm) but its positional changes on the torso, such as how much it may move laterally, and its stability upon the torso.58 Glenohumeral impingement testing as well as compression testing of the acromioclavicular joint is performed. Manual muscle testing of all shoulder related and upper extremity musculature is performed bilaterally as well. Resistive testing to enhance subtle scapular instability may also be performed. Assessment of distal pulses, sensation, muscle stretch reflexes, and distal extremity muscle bulk is performed. Palpation of not only the bony prominences but also of the bicipital groove, posterior cuff structures, trapezius, latissimus dorsi, and parascapular muscles is also performed to assess for tender spots or myofascial trigger points to conclude the initial examination. Assessment for other etiologies may need to be performed either at the end of the shoulder evaluation or on an ensuing visit to ascertain for extrinsic causes of pain including spinal, peripheral nerve, or vascular etiologies.
Many times, radiating pain that has a dysesthetic quality emanates from a non-neurogenic cause. When assessing the scapula, weakness of the supporting musculature will allow the scapula to wing away from the thoracic cage, thus creating scapular instability. The rhomboids, upper trapezius, any of the four rotator cuff muscles, or paraspinal muscles may have been weakened from the initial injury. As noted earlier, when a muscle is chronically firing at 40% or more of MMT, fatigue will become a factor. Myofascial trigger points have been described in the literature since the mid-1800s.59 Trigger points presumably appear in these fatigued muscles and on cursory look may mimic either cervical or thoracic radicular symptoms. These symptoms may include, but are not limited to, paracervical radiating pain, radiating pain through the scapular body, and radiating pain about the thorax either anteriorly or posteriorly. As described by Simmons et al., both observation and hands-on experience are needed to help delineate these etiologies.60 Symptoms may be exacerbated by manual muscle testing as well. Observation of the scapula during resistive testing such as infraspinatus strength testing or a wall push-up may help in making the diagnosis.
Motor strength testing of the shoulder girdle and rotator cuff is very useful in the overall examination of the shoulder, but not in differentiating the etiology of symptoms. Typically, intrinsic shoulder pathology will lead to weakness in one or more of the muscles of the cuff, such as the supraspinatus or infraspinatus. When the parascapular musculature is weakened, there may be good to excellent strength within the rotator cuff itself, but there may be early fatigue or enhancement of scapular instability during resistive maneuvers. Direct palpation may yield areas over the rhomboids consistent with myofascial trigger points as well. In cases of chronic cervical spine disease, especially at the C5 and C6 levels, a similar result may be noted due to the effects of neurogenic damage affecting the shoulder girdle musculature, with resultant weakness.
Electrodiagnostic studies play an important role in evaluation of the painful shoulder. It has been shown that sensory loss, such as an axillary patch for axillary nerve injuries, is unreliable in the diagnosis of axillary nerve injury.61 Electrodiagnostic testing can delineate neuromuscular involvement, including severity, and help with prognostication. Appropriately timed studies are important in defining the degree of nerve compromise.62 Electrodiagnostic testing usually is not performed until wallerian degeneration has taken place, approximately 3 weeks after injury, unless there is suspicion of nerve transection, which can be identified within 1 day of the event. The most common nerve injury associated with shoulder pathology is axillary nerve injury. Axillary nerve injury is most commonly associated with traumatic anterior shoulder dislocation, resulting in a neuropraxia or axonotmesis caused by traction.61,63 Spontaneous recovery of axillary nerve function has been documented up to 7 months after injury.64
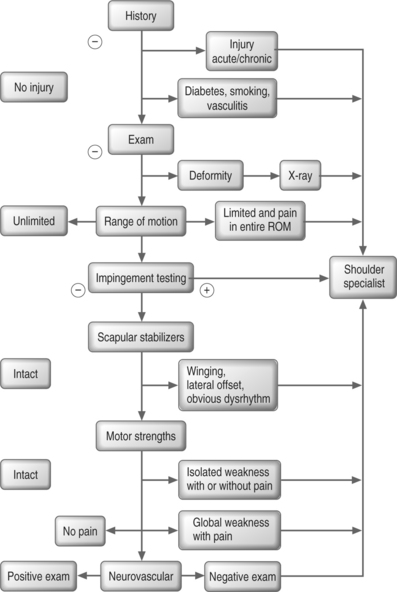
The shoulder examination may not be straightforward, even when performed by the most experienced of clinicians (Fig. 49.5) One must always be aware of extrinsic etiologies of pain in this region. The cervical spine is a primary extrinsic cause of pain and not all patients will present with ‘classic’ symptoms. A solid fund of knowledge in combination with an appropriately detailed diagnostic work-up is crucial to completely address a patient’s need for treatment and future prevention of both clinical symptoms and recurrence of pathology.
1 Steindler A. Kinesiology of the human body under normal and pathological conditions. Springfield, IL: Charles C. Thomas, 1955.
2 Bearn JG. Direct observations on the function of the capsule of the sternoclavicular joint in clavicular support. J Anat. 1967;101:159-170.
3 Codman EA. The shoulder. Boston: Thomas Todd, 1934.
4 Bost FC, Inman VTG. The pathologic changes in recurrent dislocation of the shoulder. J Bone Joint Surg. 1942;24:595.
5 Steindler A. Kinesiology of the human body under normal and pathological conditions. Springfield, IL: Charles C. Thomas, 1955.
6 Saha AK. Dynamic stability of the glenohumeral joint. Acta Orthop Scand. 1971;42:491.
7 Sarrafian SK. Gross and functional anatomy of the shoulder. Clin Orthop. 1983;173:11.
8 Cyprien JM, et al. Humeral retrotorsion and glenohumeral relationship in the normal shoulder and in recurrent anterior dislocation (scapulometry). Clin Orthop. 1983;175:8.
9 Randelli M, Gambrioli PL. Glenohumeral osteometry by computed tomography in normal and unstable shoulders. Clin Orthop. 1986;208:151.
10 Morrey B, An K-N. Biomechanics of the shoulder. In: Rockwood CJ, Matsen F, editors. The shoulder. Philadelphia: WB Saunders; 1990:208-245.
11 Soslowsky LJ, Flatow EL, Bigliani LU, et al. Articular geometry of the glenohumeral joint. Clin Orthop Rel Res. 1992;19:26-34.
12 An K-N, Chao CYS. Kinematic analysis of human movement. Ann Biomed Eng. 1984;12:585.
13 Inman V, Saunders M, Abbot L. Observations on the function of the shoulder joint. J Bone Joint Surg. 1944;27:1-30.
14 Warner JP, McMahon PJ. The role of the long head of the biceps brachii in superior stability of the glenohumeral joint. J Bone Joint Surg [Am]. 1995;77:366-372.
15 Johnston TB. The movements of the shoulder joint: A plea for the use of ‘plane of the scapula’ as the plane of reference for movements occurring at the humero-scapular joint. Br J Surg. 1937;25:252.
16 Poppen N, Walker PS. Normal and abnormal motion of the shoulder. J Bone Joint Surg [Am]. 1976;58:195-201.
17 Dvir Z, Berme N. The shoulder complex in the elevation of the arm: a mechanism approach. J Biomech. 1978;11:219.
18 Warwick R, Williams PL, editors. Gray’s anatomy, 35th edn (British Edition), Philadelphia: WB Saunders, 1973.
19 Kaltsas DS. Comparative study of the properties of the shoulder joint capsule with those of other joint capsules. Clin Orthop. 1983;173:20.
20 De Palma AF, Callery G, Bennet GA. Variational anatomy and degenerative lesions of the shoulder joint. Am Acad Orthop Surg Instr Course Lect Ser. 1949;6:225-281.
21 Basmajian JV, Bazant FJ. Factors preventing downward dislocation of the adducted shoulder joint. J Bone Joint Surg [Am]. 1959;41:1182.
22 Terry GC, Hammon D, France P. Stabilizing function of passive shoulder restraints. Unpublished data from the Hughston Orthopaedic Clinic, Columbus, GA, 1988.
23 Moseley HE, Overgaard B. The anterior capsular mechanism in recurrent anterior dislocation of the shoulder. J Bone Joint Surg [Br]. 1962;44:913.
24 De Lorme D. die Hemmungs bander des Schultergelenks and ibrc Deductung fur die Schulter Luxationen. Arch fur Klin Chirurg. 1910;92:79.
25 Turkel SJ, et al. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg [Am]. 1981;63:1208.
26 Ouesen J, Nielsen S. Stability of the shoulder joint. Acta Orthop Scand. 1985;56:149.
27 O’Brien SJ, Arnoczsky SP, Warren RF, et al. The anatomy of the inferior glenohumeral ligament complex of the shoulder. Am J Sports Med. 1990;18:449.
28 Jobe FW, Pink M. Shoulder injuries in the athlete: The stability continuum and treatment. J Hand Therapy Ar. 1991;June:69-72.
29 Cleland J. Notes on raising the arm. J Anat Physiol. 1884;18:275.
30 Goss TP. The scapula: coracoid, acromial and avulsion fractures. Am J Orthop. 1996;25:106-115.
31 Nobuhara K. The shoulder: its function and clinical aspects. Tokyo: Igasu-Shoin, 1987.
32 Doody SG, Freedman L, Waterland JC. Shoulder movements during abduction in the scapular plane. Arch Phys Med Rehabil. 1970;51:595-604.
33 Perry J. Anatomy and biomechanics of the shoulder in throwing, swimming, gymnastics and tennis. Symposium on injuries to the shoulder in the athlete. Clin Sports Med. 1987;2:247.
34 Matsen FA, Craig TA. Subacromial impingement. In: Matsen F, Rockwood C, editors. The shoulder. Philadelphia: WB Saunders; 1990:623-647.
35 Speer KE, Garret WE. Muscular control of motion and stability about the pectoral girdle. In: Matsen FA, Fu F, Hawkins RJ, editors. The shoulder: a balance of mobility and stability. Rosemont, IL: AAOS; 1994:159-173.
36 Ellen MI, Gilhool JJ, Rogers DP. Scapular instability. The scapulothoracic joint. Phys Med Rehabil Clin N Am. 2000;11(4):755-770.
37 Dines DM, Lenison M. The conservative management of the unstable shoulder including rehabilitation. Clin Sports Med. 1995;14:707-816.
38 Moore KL. Clinically oriented anatomy, 3rd edn., Baltimore: Williams and Wilkins; 1992:522.
39 Ferrante MF. Medical management of chronic shoulder pain. In: Iannotti JP, Williams GRJr, editors. Disorders of the shoulder. Philadelphia: Lippincott Williams & Wilkins; 1999:1043-1073.
40 Hurley JA. Anatomy of the shoulder. In: Nicholas JA, Hershman EB, editors. The upper extremity in sports medicine. St. Louis: Mosby; 1995:23-38.
41 Bryan WJ, Schauder K, Tullos H. The axillary nerve and its relationship to common sports medicine shoulder procedures. Am J Sports Med. 1986;14:114.
42 Gardener E. The innervation of the shoulder joint. Anat Rec. 1949;102:1.
43 Hollinshead WH. The upper limb. In: Jenkins DB, editor. Hollinshead’s functional anatomy of the limbs and back. 8th edn. Philadelphia: WB. Saunders; 2002:63-219.
44 Steward JD. Focal peripheral neuropathies, 2nd ed. New York: Elsevier, 1993.
45 McCarthy WJ, Yao JS, Schafer MF. Upper extremity arterial injury in athletes. J Vasc surg. 1989;9:317-326.
46 Nuber GW, McCarthy WJ, Yao JST, et al. Arterial abnormalities of the shoulder in athletes. Am J Sports Med. 1990;18:514-519.
47 Baker CL, Liu SH. Neurovascular injuries to the shoulder. J Orthop Sports Phys Ther. 1993;18:360-364.
48 Jensen C, Rayan GM. Thoracic outlet syndrome: provocative examination maneuvers in a typical population. J Shoulder Elbow Surg. 1995;4:113-117.
49 Konin JG, Wiksten DL, Isear JAJr, et al. Special tests for orthopedic examination, 2nd edn. New Jersey: Slack, 2002.
50 Vecchio PR, Kavanagh BL, Hazelman RH, et al. Shoulder pain in a community-based rheumatology clinic. Br J Rheumotol. 1995;34:440-442.
51 Smith DL, Campbell SM. Painful shoulder syndromes: Diagnosis and management. J Gen Int Med. 1992;7:328-339.
52 Symonds MB. Accurate diagnosis and treatment in painful shoulder conditions. J Int Med Res. 1975;3:261-266.
53 Kessel L, Watson M. The painful arc syndrome. Clinical classification as a guide to management. J Bone Joint Surg. 1977;59:166-172.
54 Chard M, Hazelman B. Shoulder disorders in the elderly (a hospital study). Ann Rheum Dis. 1987;46:684-687.
55 Slipman CW, Shin CH, Ellen MI, et al. An unusual case of shoulder pain. Pain Phys. 2000;3(4):352-356.
56 Cuomo F. Diagnosis, classification, and management of the stiff shoulder. In: Iannotti JP, Williams GRJr, editors. Disorders of the shoulder: diagnosis and management. Philadelphia: Lippincott Williams & Wilkins; 1999:397-417.
57 Wirganowicz PZ, Eckardt JJ. Neoplasms of the shoulder girdle. In: Iannotti JP, Williams GRJr, editors. Disorders of the shoulder: diagnosis and management. Philadelphia: Lippincott Williams & Wilkins; 1999:929-947.
58 Kibler WB. The role of the scapula in the overhead throwing motion. Contemp Orthop. 1991;22:525-532.
59 Froreip. Ein Beitrag zur pathologie und therapie des rheumatismus. Weimar. 1843.
60 Simmons DG, et al. Myofascial pain and dysfunction. The trigger point manual, 2nd edn., Baltimore: Williams and Wilkins; 1999:21-45.
61 Blom S, Dahlback LO. Nerve injuries in dislocations of the shoulder joint and fractures of the neck of the humerus. Acta Chir Scand. 1970;136:461-466.
62 Dowdy PA, Ernlund LS, Warner JJP. Contracture and other complications. In: Warren RF, Craig EV, Altchek DW, editors. The unstable shoulder. Philadelphia: Lippincott-Raven; 1999:403-428.
63 Brown JT. Nerve injuries complicating dislocation of the shoulder. J Bone Joint Surg [Br]. 1952;34:526.
64 Hirsch S. Paralysis of the axillary (circumflex) nerve with spontaneous recovery after 7 months. JAMA. 1936;106:705.