Massively dilated bile ducts (either diffuse or localized) filled with mucin
• CT/MR: Markedly dilated intra-/extrahepatic bile ducts with mural nodularity or discrete intraductal mass
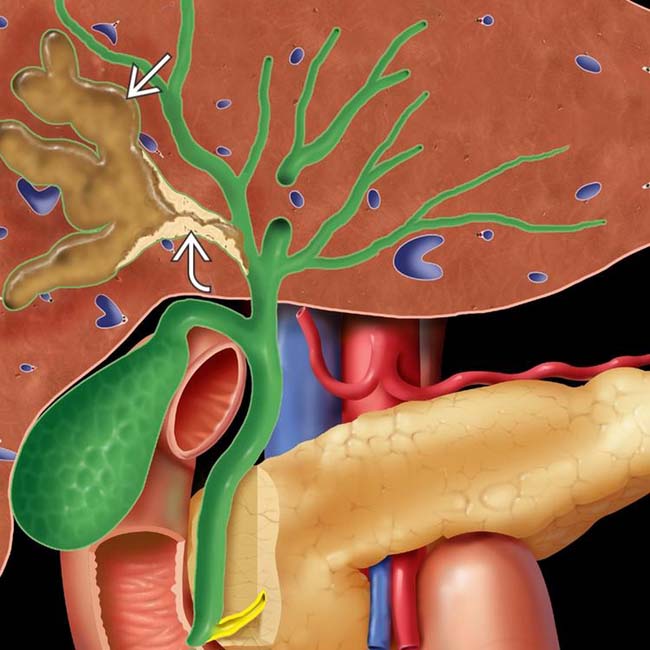
 , which are filled with mucin and contain a mucosal mass
, which are filled with mucin and contain a mucosal mass  arising from the ductal epithelium.
arising from the ductal epithelium.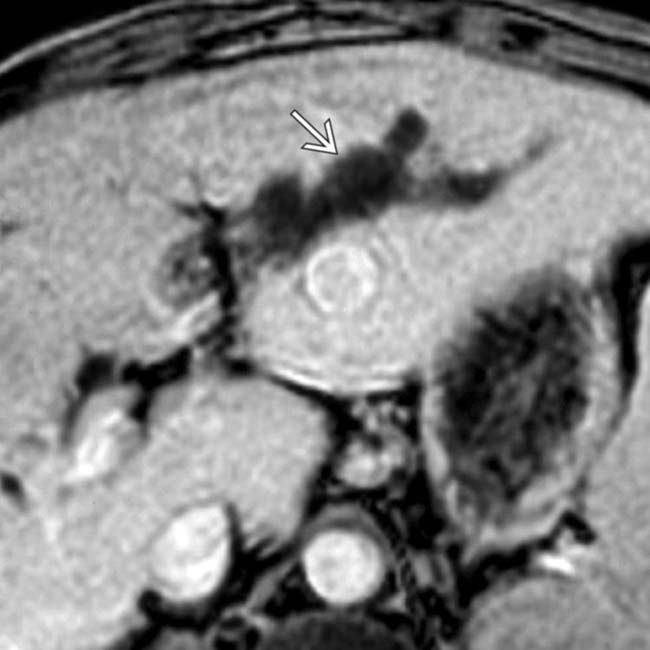
 , which proved to be biliary IPMN at surgery.
, which proved to be biliary IPMN at surgery.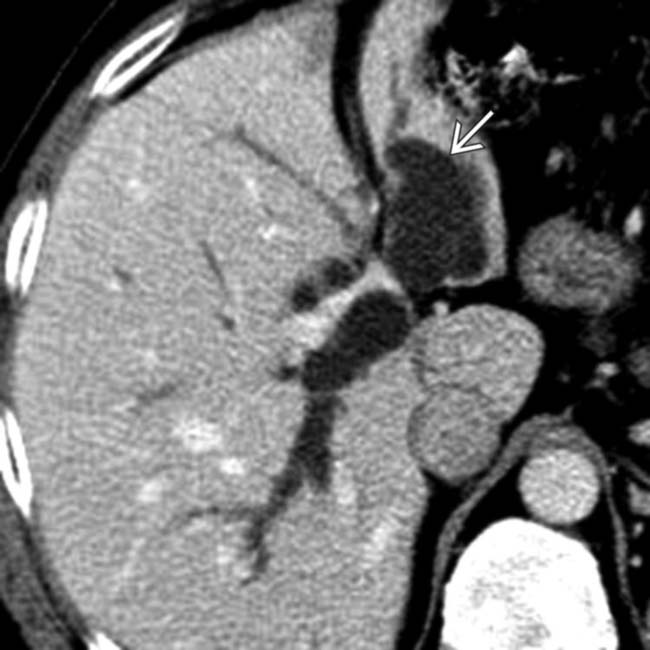
 greater than the right. ERCP and subsequent surgery revealed a left duct biliary IPMN.
greater than the right. ERCP and subsequent surgery revealed a left duct biliary IPMN.
 and subtle enhancing nodularity within the proximal left duct
and subtle enhancing nodularity within the proximal left duct  . Intraductal cholangiocarcinoma and background biliary IPMN were identified at histology. (Courtesy S. Yeon Kim, MD.)
. Intraductal cholangiocarcinoma and background biliary IPMN were identified at histology. (Courtesy S. Yeon Kim, MD.)IMAGING
General Features
Radiographic Findings
• ERCP
 Extrusion of clear mucin from patulous ampulla visible to endoscopist due to mucin hypersecretion by tumor
Extrusion of clear mucin from patulous ampulla visible to endoscopist due to mucin hypersecretion by tumor
 Extrusion of clear mucin from patulous ampulla visible to endoscopist due to mucin hypersecretion by tumor
Extrusion of clear mucin from patulous ampulla visible to endoscopist due to mucin hypersecretion by tumorDIFFERENTIAL DIAGNOSIS
Biliary Cystadenoma/Cystadenocarcinoma
CLINICAL ISSUES
Presentation
• Most common signs/symptoms

 , found to be a biliary IPMN.
, found to be a biliary IPMN.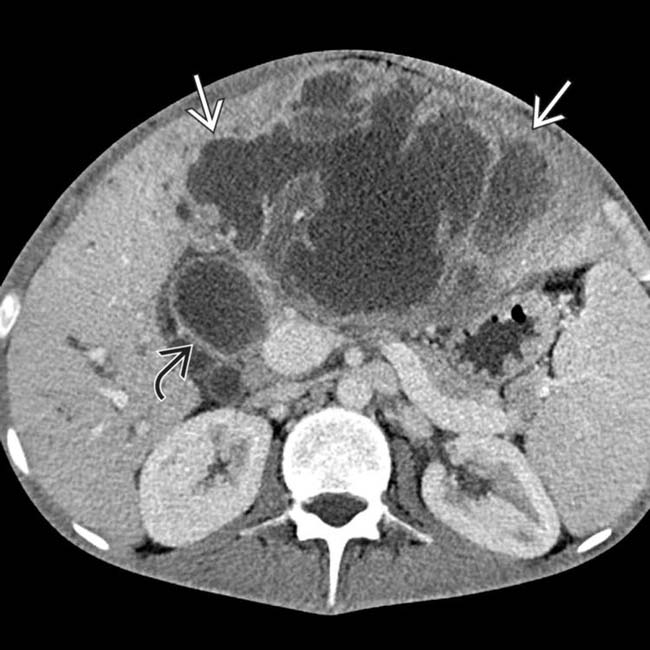
 with an irregular wall and contiguity with the biliary tree. Note the dilated common duct
with an irregular wall and contiguity with the biliary tree. Note the dilated common duct  , which communicates with the mass. This was found to be malignant degeneration of a biliary IPMN, with much of the “mass” representing dilated intrahepatic ducts filled with mucin.
, which communicates with the mass. This was found to be malignant degeneration of a biliary IPMN, with much of the “mass” representing dilated intrahepatic ducts filled with mucin.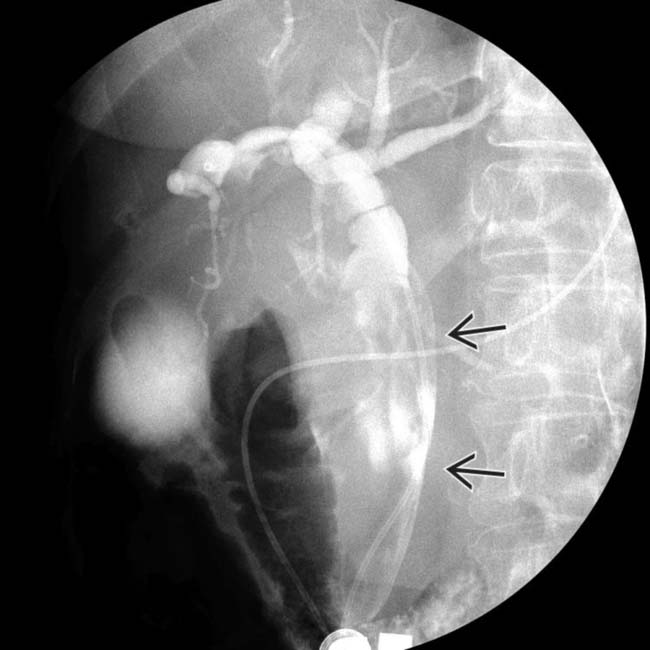
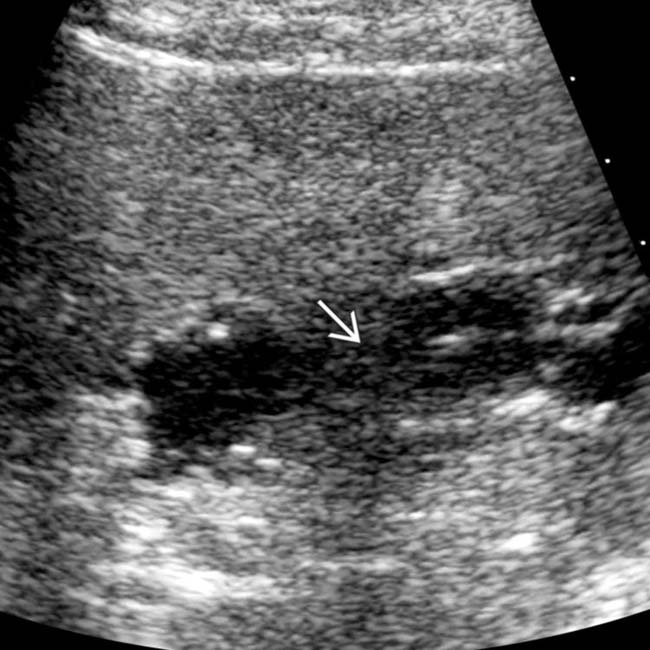
 within a dilated common duct. CECT (not shown) revealed marked asymmetric right and common bile duct dilatation. (Courtesy S. Yeon Kim, MD.)
within a dilated common duct. CECT (not shown) revealed marked asymmetric right and common bile duct dilatation. (Courtesy S. Yeon Kim, MD.)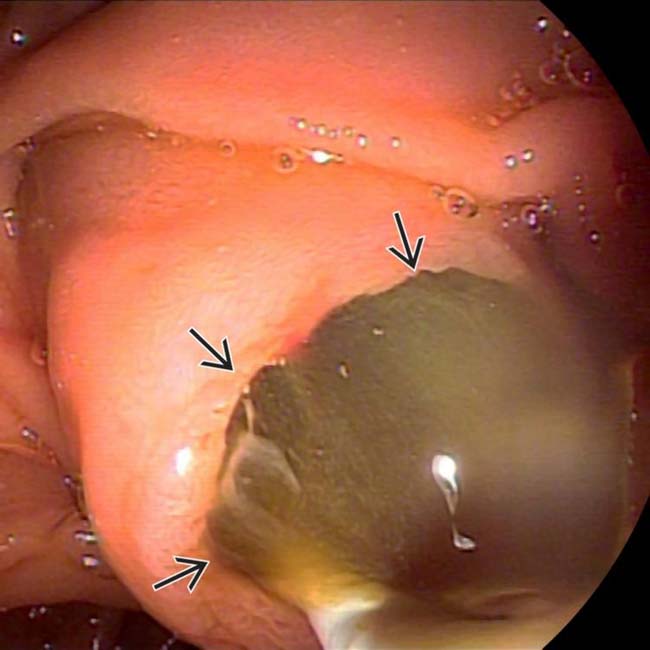
 draining from a patulous, bulging papilla. The final diagnosis after right hepatectomy and bile duct resection was biliary IPMN associated with invasive carcinoma. (Courtesy S. Yeon Kim, MD.)
draining from a patulous, bulging papilla. The final diagnosis after right hepatectomy and bile duct resection was biliary IPMN associated with invasive carcinoma. (Courtesy S. Yeon Kim, MD.)
 . An ERCP performed previously reported a mucus “plug.”
. An ERCP performed previously reported a mucus “plug.”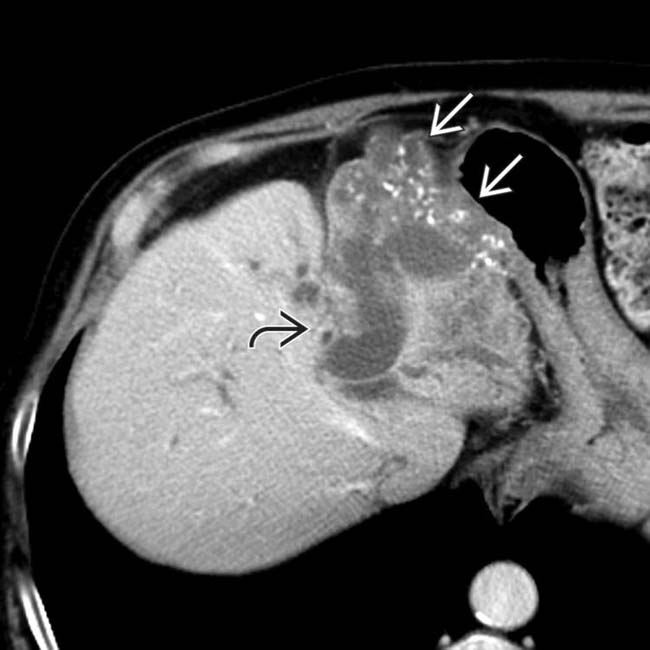
 , lobar atrophy, and calcifications
, lobar atrophy, and calcifications  . Biliary IPMN and mucinous adenocarcinoma were identified at left hepatectomy. Biliary IPMN is a premalignant lesion and is considered a precursor for papillary cholangiocarcinoma.
. Biliary IPMN and mucinous adenocarcinoma were identified at left hepatectomy. Biliary IPMN is a premalignant lesion and is considered a precursor for papillary cholangiocarcinoma.


























































 distended with mucin.
distended with mucin.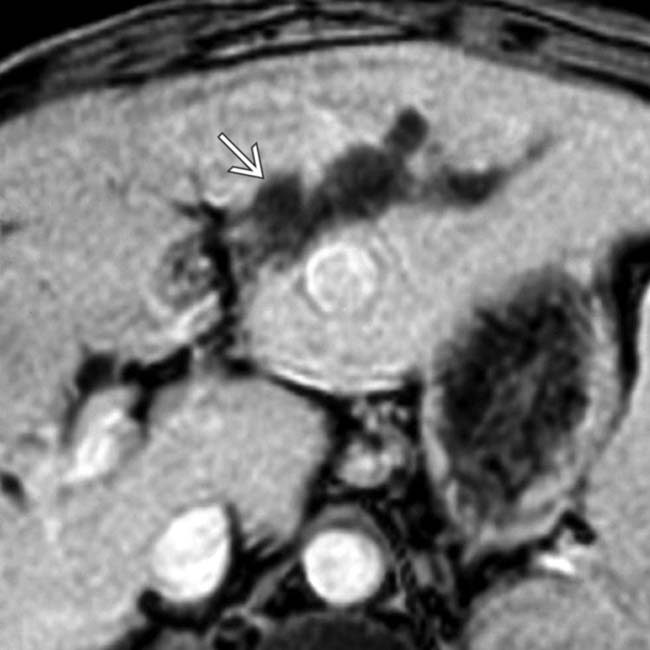
 .
.
 .
.


