Gil-Bello, D, et al. Calcification in biliary hamartomatosis. Br J Radiol. 2012; 85(1012):e99–101.
Desmet, VJ. Ductal plates in hepatic ductular reactions. Hypothesis and implications. III. Implications for liver pathology. Virchows Arch. 2011; 458(3):271–279.
Venkatanarasimha, N, et al. Imaging features of ductal plate malformations in adults. Clin Radiol. 2011; 66(11):1086–1093.
Drenth, JP, et al. Congenital fibrocystic liver diseases. Best Pract Res Clin Gastroenterol. 2010; 24(5):573–584.
Hughes, NR, et al. An immunohistochemical profile of the so-called bile duct adenoma: clues to pathogenesis. Am J Surg Pathol. 2010; 34(9):1312–1318.
Orii, T, et al. Cholangiocarcinoma arising from preexisting biliary hamartoma of liver—report of a case. Hepatogastroenterology. 2003; 50(50):333–336.
Mortele, B, et al. Hepatic bile duct hamartomas (von Meyenburg Complexes): MR and MR cholangiography findings. J Comput Assist Tomogr. 2002; 26(3):438–443.
Allgaier, HP, et al. Ampullary hamartoma: A rare cause of biliary obstruction. Digestion. 1999; 60(5):497–500.
Semelka, RC, et al. Biliary hamartomas: solitary and multiple lesions shown on current MR techniques including gadolinium enhancement. J Magn Reson Imaging. 1999; 10(2):196–201.
von Schweinitz, D, et al. Mesenchymal hamartoma of the liver—new insight into histogenesis. J Pediatr Surg. 1999; 34(8):1269–1271.
Cheung, YC, et al. MRI of multiple biliary hamartomas. Br J Radiol. 1997; 70(833):527–529.
Principe, A, et al. Bile duct hamartomas: diagnostic problems and treatment. Hepatogastroenterology. 1997; 44(16):994–997.
Iha, H, et al. Biliary hamartomas simulating multiple hepatic metastasis on imaging findings. Kurume Med J. 1996; 43(3):231–235.
Lev-Toaff, AS, et al. The radiologic and pathologic spectrum of biliary hamartomas. AJR Am J Roentgenol. 1995; 165(2):309–313.
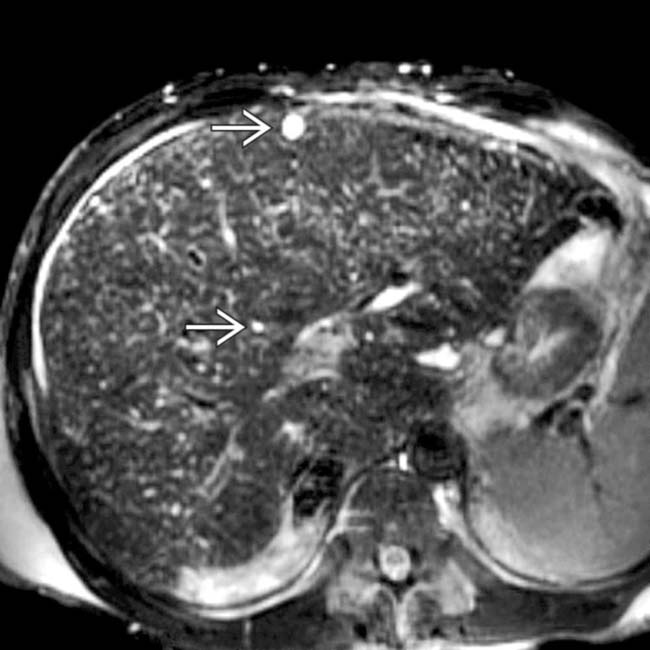
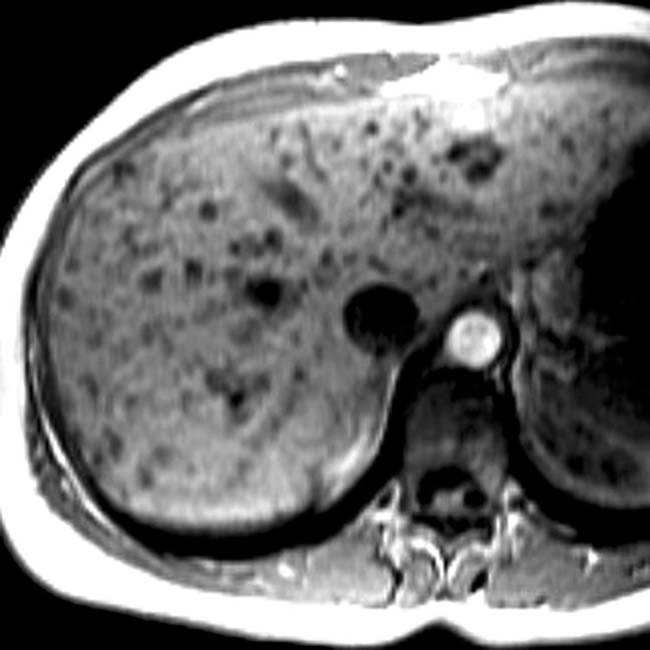
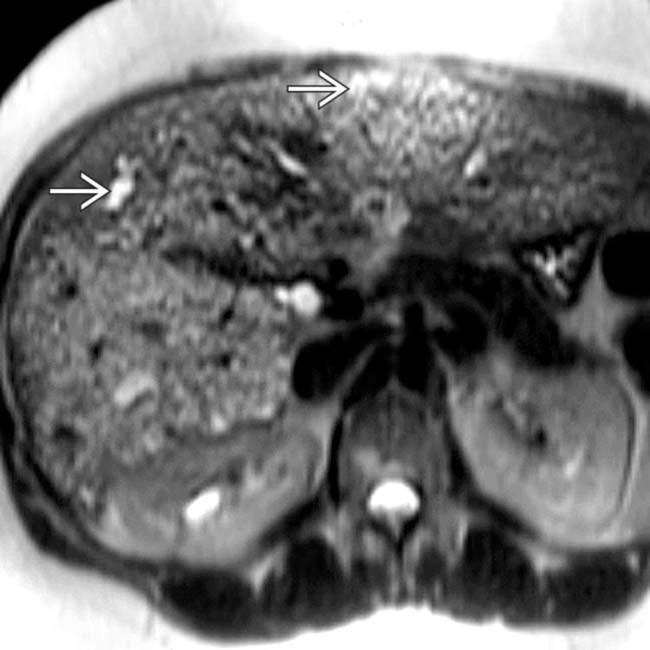
 , representing biliary hamartomas. This patient also had evidence of congenital hepatic fibrosis on imaging and liver biopsy, both part of the congenital hepatic and renal fibropolycystic disease spectrum.
, representing biliary hamartomas. This patient also had evidence of congenital hepatic fibrosis on imaging and liver biopsy, both part of the congenital hepatic and renal fibropolycystic disease spectrum.
 that do not communicate with the (normal) biliary tree. This feature helps to distinguish biliary hamartomas from Caroli disease.
that do not communicate with the (normal) biliary tree. This feature helps to distinguish biliary hamartomas from Caroli disease.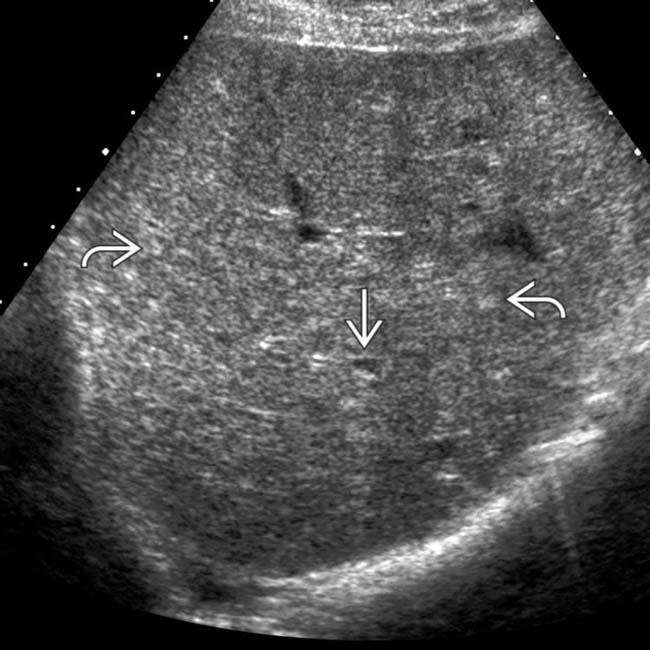
 throughout the liver and 1 of ∼ 10 cyst-like lesions
throughout the liver and 1 of ∼ 10 cyst-like lesions  , though even these have small foci of echogenicity within the wall. MR on this patient showed many more cystic-appearing biliary hamartomas.
, though even these have small foci of echogenicity within the wall. MR on this patient showed many more cystic-appearing biliary hamartomas.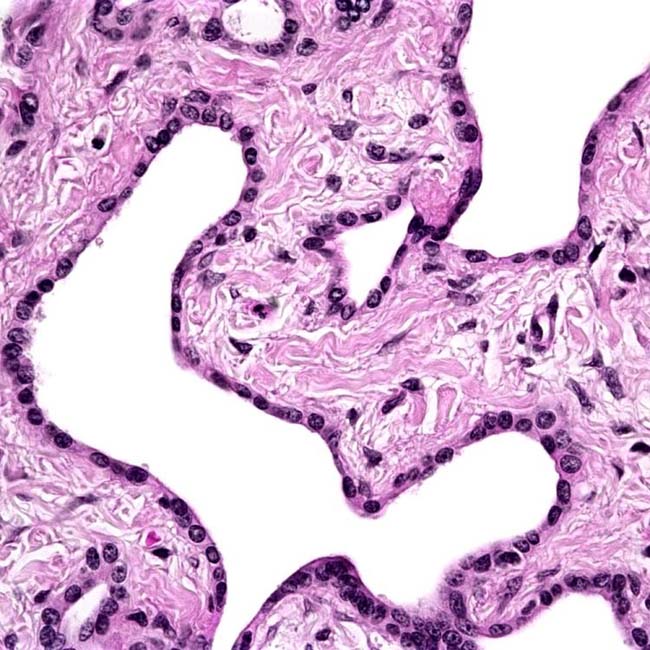

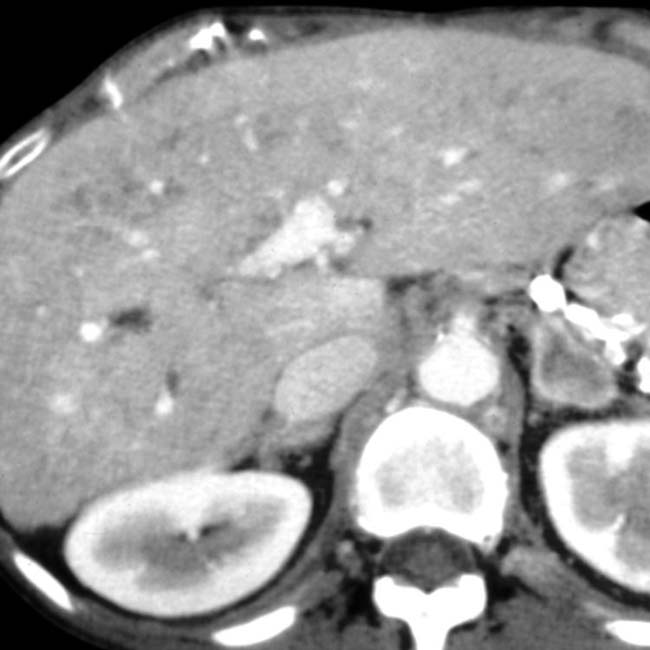
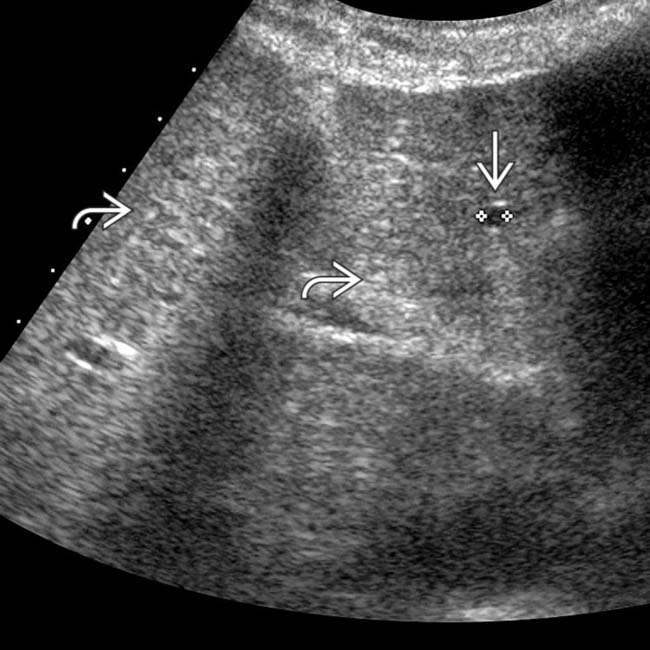
 throughout the liver. Incidental note is made of surgical clips
throughout the liver. Incidental note is made of surgical clips  from the prior nephrectomy. These biliary hamartomas should not be mistaken for metastases.
from the prior nephrectomy. These biliary hamartomas should not be mistaken for metastases.
 that almost certainly represent biliary hamartomas. These have remained stable for years, and the patient is not immunosuppressed.
that almost certainly represent biliary hamartomas. These have remained stable for years, and the patient is not immunosuppressed.
 .
.
 , while there are innumerable tiny echogenic foci
, while there are innumerable tiny echogenic foci  throughout the liver that correspond to the smaller biliary hamartomas, which presumably contain relatively more fibrous tissue and less fluid.
throughout the liver that correspond to the smaller biliary hamartomas, which presumably contain relatively more fibrous tissue and less fluid.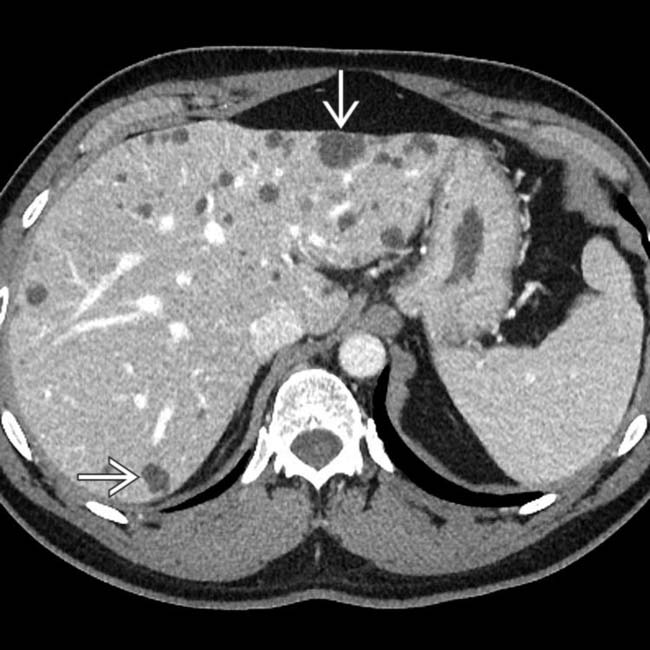
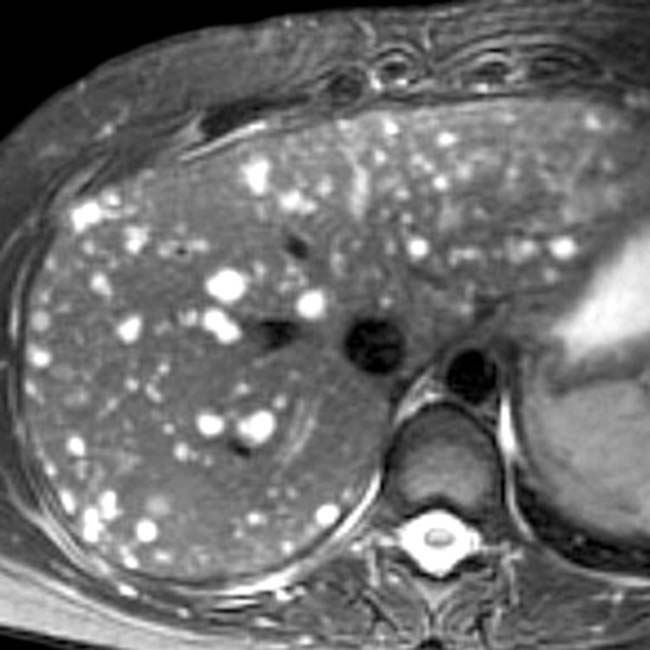
 . These are typical findings for biliary hamartomas and would be a very rare (unreported) feature of hepatocellular carcinoma (HCC).
. These are typical findings for biliary hamartomas and would be a very rare (unreported) feature of hepatocellular carcinoma (HCC).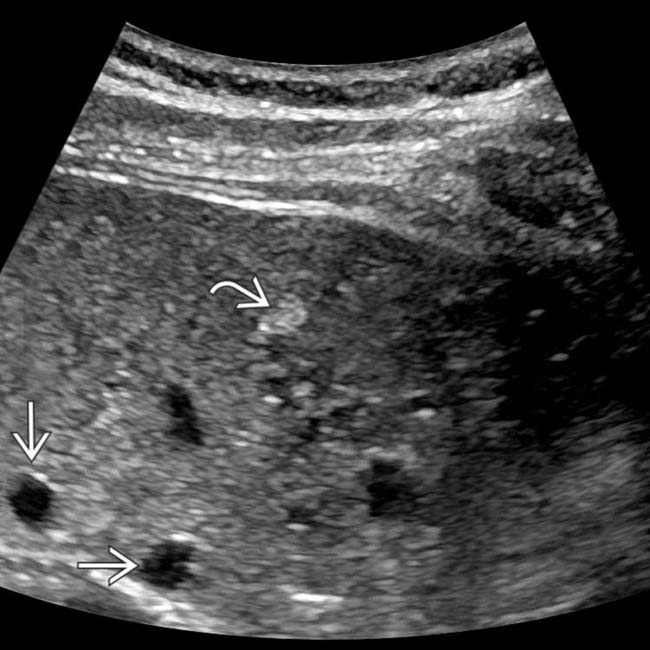
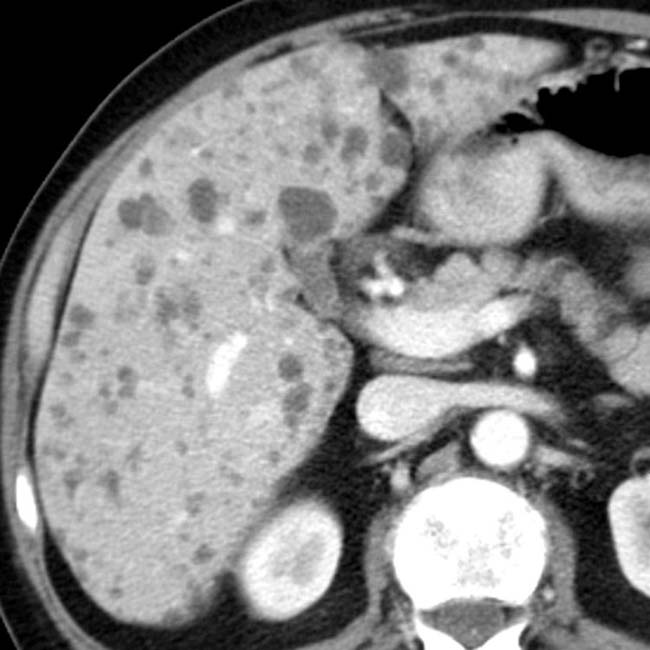
 and many more cystic lesions
and many more cystic lesions  . None of these lesions showed interval change on subsequent imaging studies over several years and likely represent biliary hamartomas.
. None of these lesions showed interval change on subsequent imaging studies over several years and likely represent biliary hamartomas.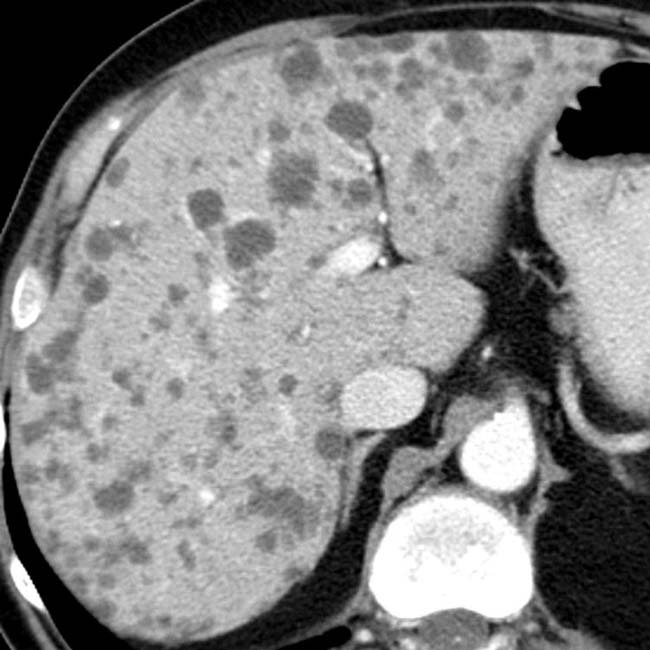

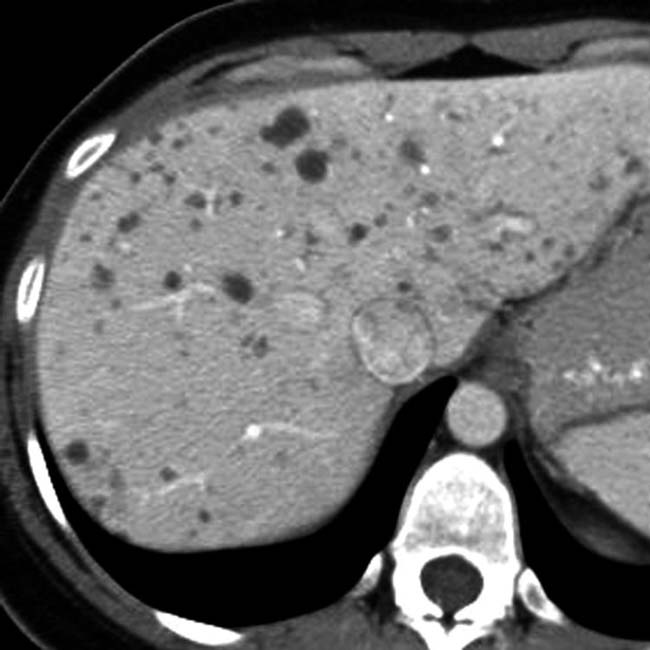
 throughout the liver, too small to permit accurate density measurements. In a healthy, nononcologic patient, they likely represent biliary hamartomas.
throughout the liver, too small to permit accurate density measurements. In a healthy, nononcologic patient, they likely represent biliary hamartomas.
 . This patient also had an enlarged, dysmorphic liver and supernumerary and enlarged hepatic arteries as signs of congenital hepatic fibrosis.
. This patient also had an enlarged, dysmorphic liver and supernumerary and enlarged hepatic arteries as signs of congenital hepatic fibrosis.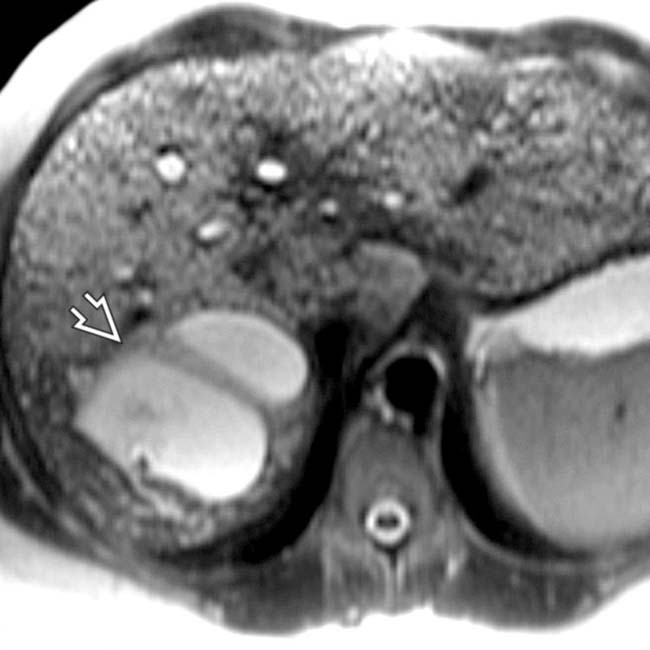
 that communicate with the biliary tree and represent aberrant bile duct cysts of Caroli disease. Congenital hepatic fibrosis, Caroli disease, and biliary hamartomas are all manifestations of fibropolycystic disease.
that communicate with the biliary tree and represent aberrant bile duct cysts of Caroli disease. Congenital hepatic fibrosis, Caroli disease, and biliary hamartomas are all manifestations of fibropolycystic disease.