Romagnoli, R, et al. Liver transplantation for symptomatic centrohepatic biliary cystadenoma. Clin Res Hepatol Gastroenterol. 2011; 35(5):408–413.
Bogert, JN, et al. Education and imaging. Hepatobiliary and pancreatic: Mucinous cystadenoma of the biliary tree. J Gastroenterol Hepatol. 2010; 25(7):1332.
Choi, HK, et al. Differential diagnosis for intrahepatic biliary cystadenoma and hepatic simple cyst: significance of cystic fluid analysis and radiologic findings. J Clin Gastroenterol. 2010; 44(4):289–293.
Seo, JK, et al. Appropriate diagnosis of biliary cystic tumors: comparison with atypical hepatic simple cysts. Eur J Gastroenterol Hepatol. 2010; 22(8):989–996.
Yu, J, et al. Hepatobiliary mucinous cystadenoma and cystadenocarcinoma: report of six cases and review of the literature. Hepatogastroenterology. 2010; 57(99–100):451–455.
Limongelli, P, et al. Cystic tumors of the biliary tract: a complete excision is crucial. Int Surg. 2009; 94(2):136–140.
Del Poggio, P, et al. Cystic tumors of the liver: a practical approach. World J Gastroenterol. 2008; 14(23):3616–3620.
Delis, SG, et al. Intrahepatic biliary cystadenoma: a need for radical resection. Eur J Gastroenterol Hepatol. 2008; 20(1):10–14.
Mourra, N, et al. Clinical challenges and images in GI. Extrahepatic biliary cystadenoma with mesenchymal stroma. Gastroenterology. 2008; 134(5):1295. [1637].
Levy, AD, et al. From the archives of the AFIP. Benign tumors and tumorlike lesions of the gallbladder and extrahepatic bile ducts: radiologic-pathologic correlation. Armed Forces Institute of Pathology. Radiographics. 2002; 22(2):387–413.
Mortelé, KJ, et al. Cystic focal liver lesions in the adult: differential CT and MR imaging features. Radiographics. 2001; 21(4):895–910.
Gabata, T, et al. Biliary cystadenoma with mesenchymal stroma of the liver: correlation between unusual MR appearance and pathologic findings. J Magn Reson Imaging. 1998; 8(2):503–504.
Singh, Y, et al. Multiloculated cystic liver lesions: radiologic-pathologic differential diagnosis. Radiographics. 1997; 17(1):219–224.
Buetow, PC, et al. Biliary cystadenoma and cystadenocarcinoma: clinical-imaging-pathologic correlations with emphasis on the importance of ovarian stroma. Radiology. 1995; 196(3):805–810.

 . These findings in a patient with no other known tumor could be considered sufficiently diagnostic of a biliary cystadenoma to warrant resection without further evaluation.
. These findings in a patient with no other known tumor could be considered sufficiently diagnostic of a biliary cystadenoma to warrant resection without further evaluation.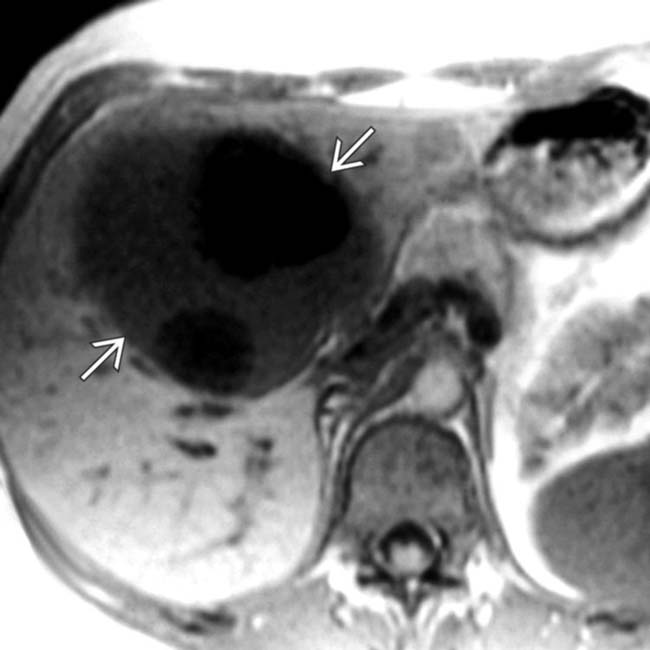
 with cyst contents having features characteristic of fairly simple fluid. There is slight heterogeneity of the signal that varies between some of the cyst compartments.
with cyst contents having features characteristic of fairly simple fluid. There is slight heterogeneity of the signal that varies between some of the cyst compartments.
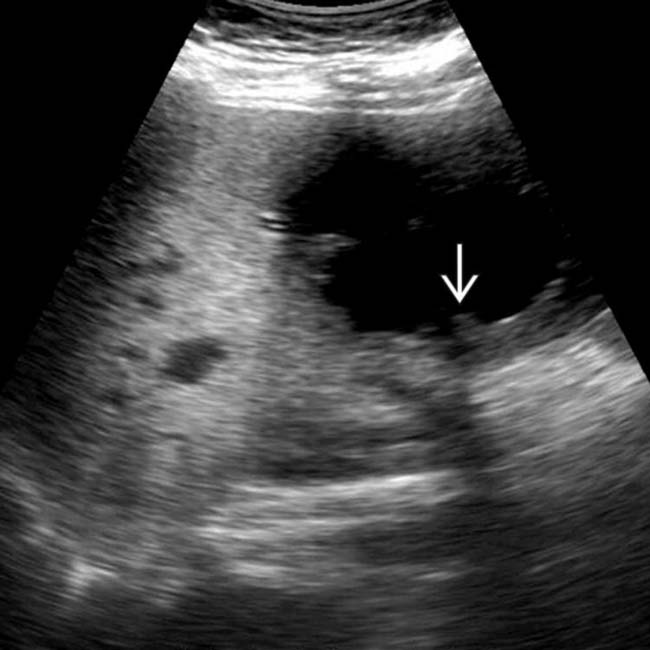
 within 1 of the larger cystic spaces strongly suggests a neoplastic etiology.
within 1 of the larger cystic spaces strongly suggests a neoplastic etiology.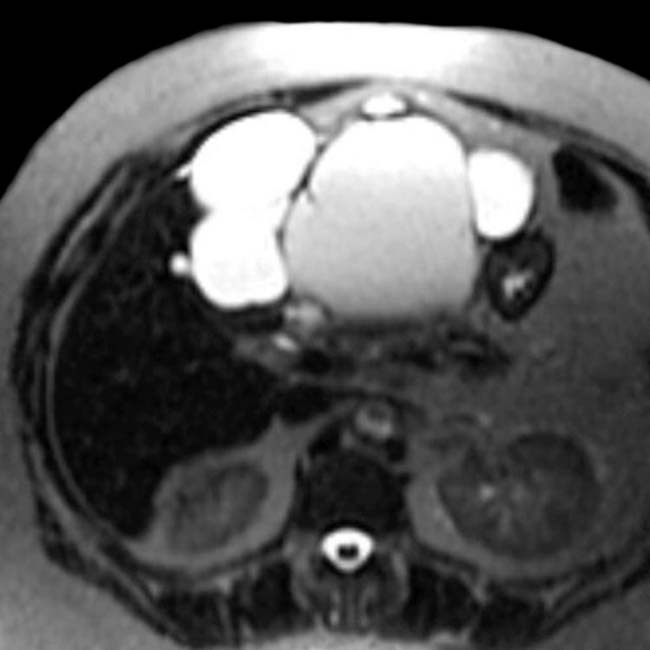

 within 1 of the larger cystic spaces, strongly suggesting a neoplastic etiology. This proved to be a biliary cystadenoma with foci of cellular atypia in the mucosal lining.
within 1 of the larger cystic spaces, strongly suggesting a neoplastic etiology. This proved to be a biliary cystadenoma with foci of cellular atypia in the mucosal lining.

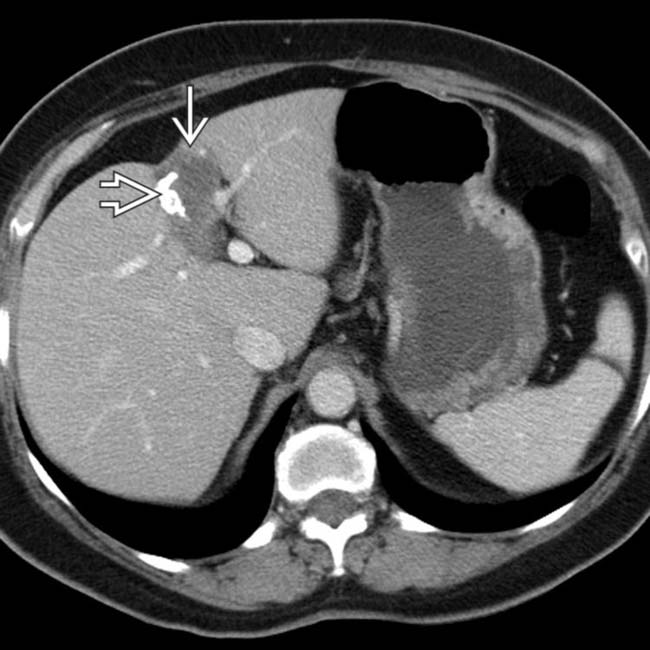
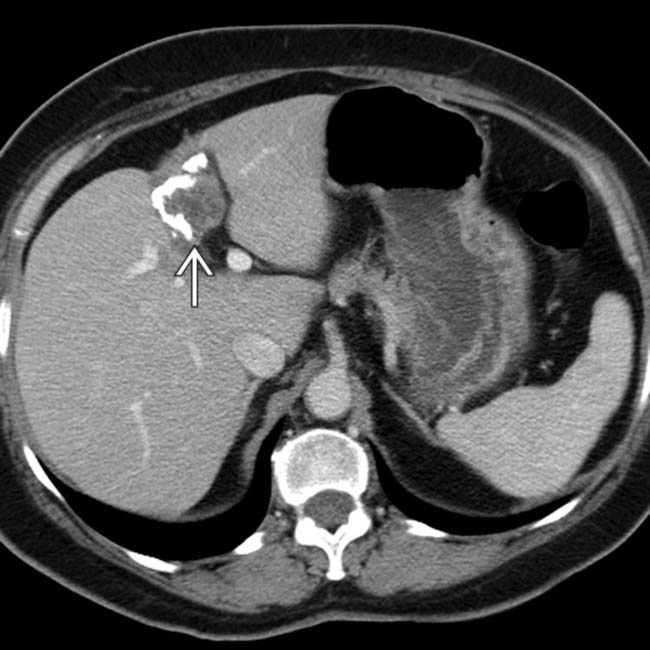
 with foci of coarse calcification
with foci of coarse calcification  .
.
 , which was clearly separate from the gallbladder. This was interpreted as an “indeterminate mass” with a recommendation for follow-up, but no differential diagnosis nor recommended interval for follow-up was provided.
, which was clearly separate from the gallbladder. This was interpreted as an “indeterminate mass” with a recommendation for follow-up, but no differential diagnosis nor recommended interval for follow-up was provided.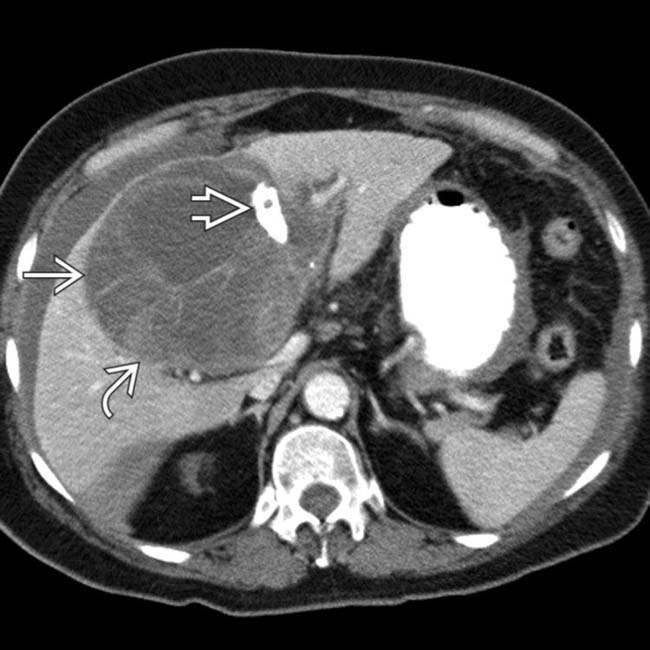
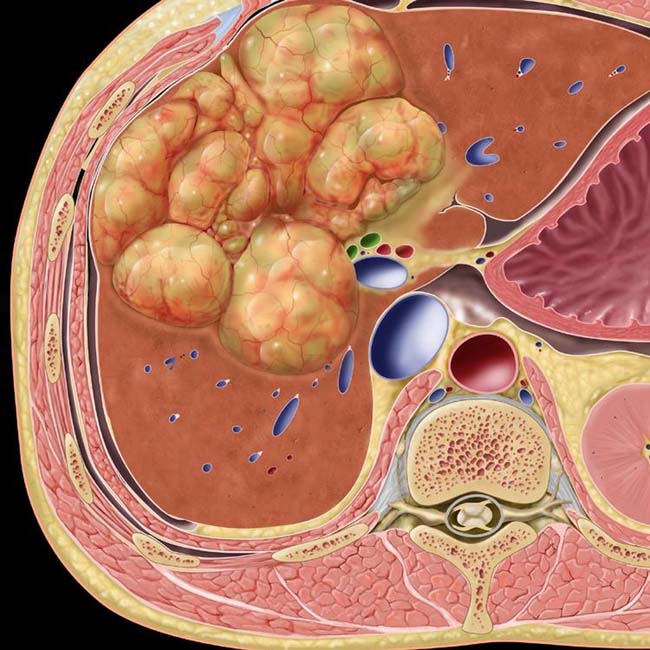
 with mural nodularity and solid components
with mural nodularity and solid components  as well as focal calcifications
as well as focal calcifications  . The presence of higher-than-water-density fluid in the peritoneal cavity suggests that the mass has ruptured.
. The presence of higher-than-water-density fluid in the peritoneal cavity suggests that the mass has ruptured.
 , calcification, and exudative or hemorrhagic ascites.
, calcification, and exudative or hemorrhagic ascites.
 with its mural nodularity and coarse calcification, along with complex ascites due to spontaneous rupture of the cystic tumor.
with its mural nodularity and coarse calcification, along with complex ascites due to spontaneous rupture of the cystic tumor.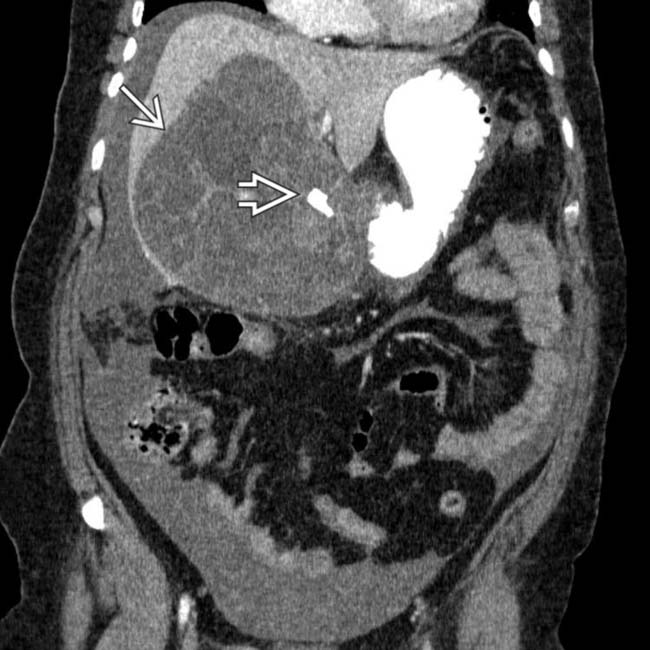
 and the focal calcification
and the focal calcification  . At surgery (right trisegmentectomy), a ruptured biliary cystadenocarcinoma was confirmed. This lesion could have been resected 5 years earlier with much less morbidity and with a better prognosis.
. At surgery (right trisegmentectomy), a ruptured biliary cystadenocarcinoma was confirmed. This lesion could have been resected 5 years earlier with much less morbidity and with a better prognosis.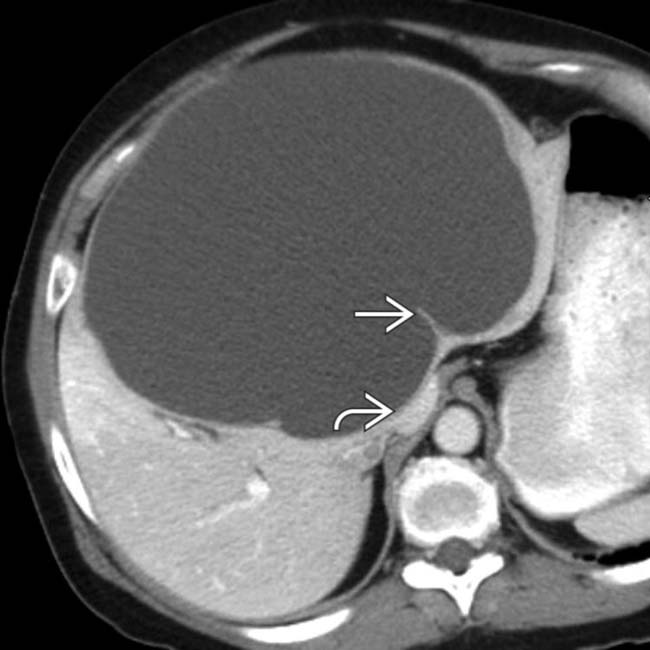
 . Note the proximity to, and mass effect on, the IVC
. Note the proximity to, and mass effect on, the IVC  and hepatic veins.
and hepatic veins.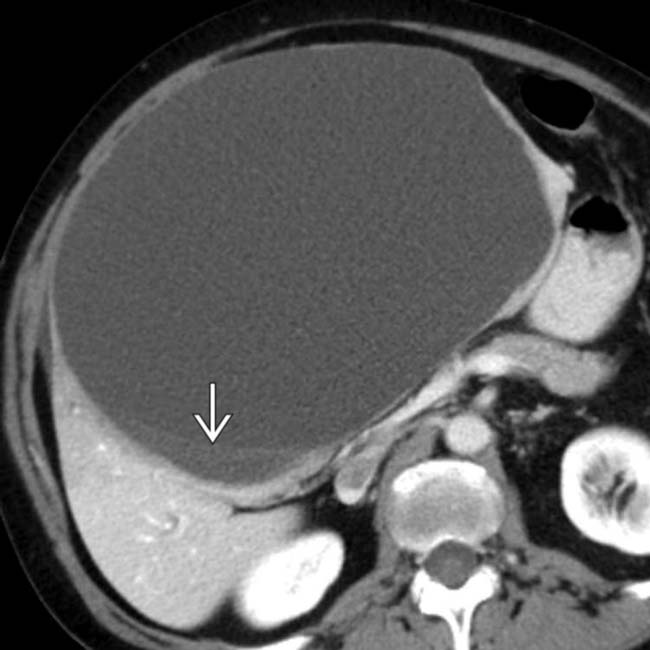
 . At surgery, the mass was resected, but a portion of the posterior wall could not be resected completely due to the adjacent large veins.
. At surgery, the mass was resected, but a portion of the posterior wall could not be resected completely due to the adjacent large veins.
 are visible.
are visible.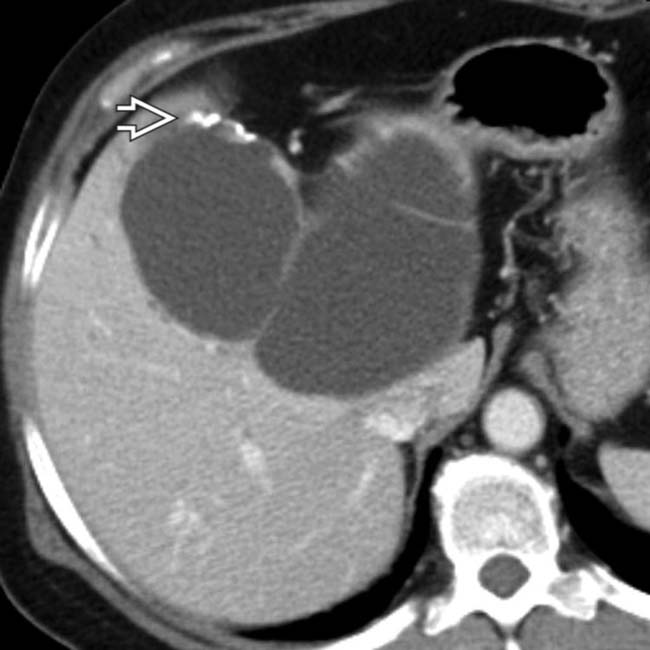
 and a multiseptate cystic mass very similar in size and appearance to the tumor seen before surgery. Incompletely resected biliary cystadenomas and cystadenocarcinomas often recur.
and a multiseptate cystic mass very similar in size and appearance to the tumor seen before surgery. Incompletely resected biliary cystadenomas and cystadenocarcinomas often recur.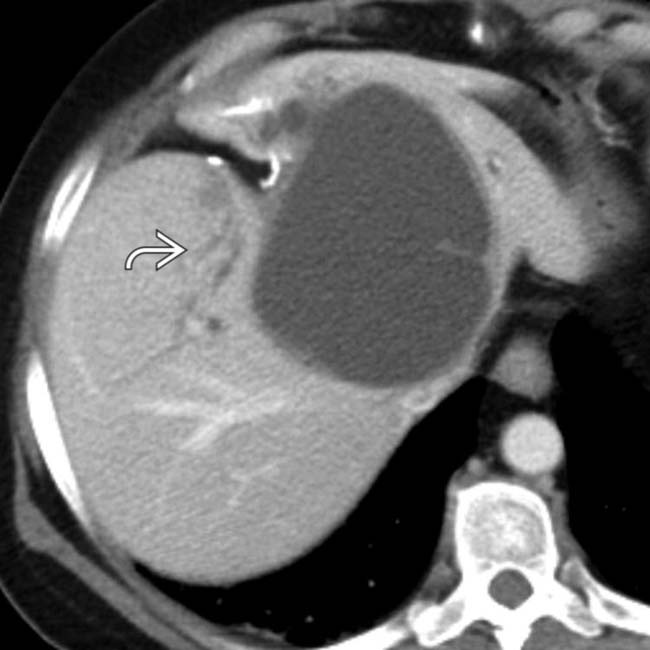
 , which can be considered a bad prognostic sign of invasion, and a malignant character of cystic hepatic tumors.
, which can be considered a bad prognostic sign of invasion, and a malignant character of cystic hepatic tumors.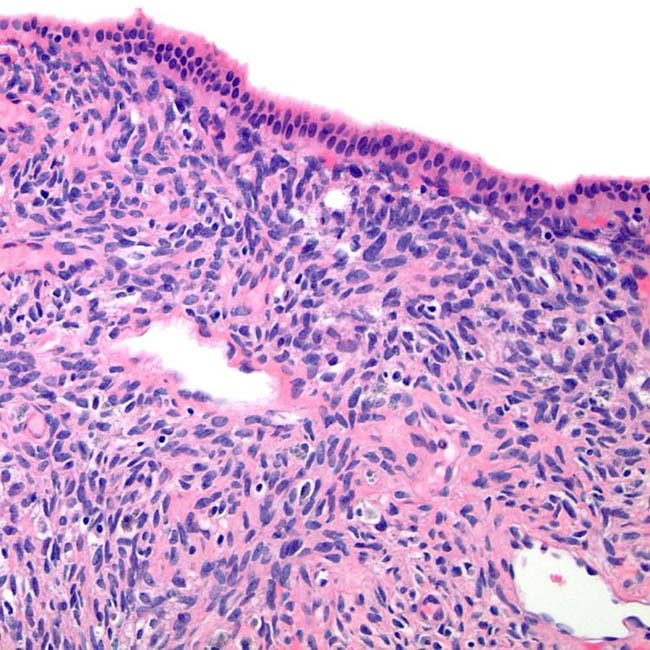




































































 within the cystic mass.
within the cystic mass.




