6 Beginning the learning experience
Preparing for the placement
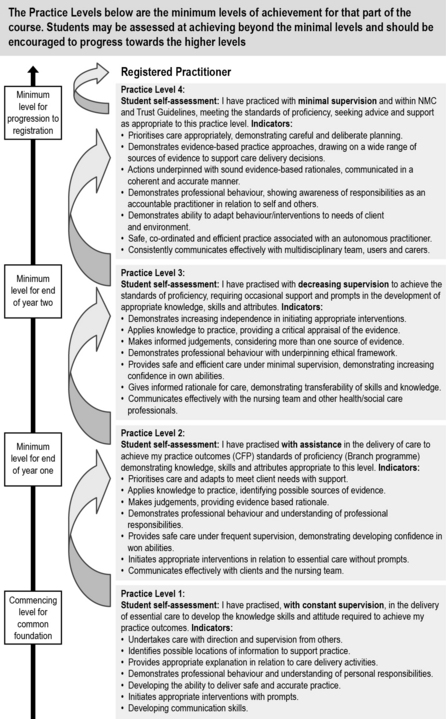
Although all student nurses are required to meet the NMC standards for pre-registration nursing education (NMC 2010) before progressing to registration, each university has a different method of assessing the level of competency. Benner’s (1984)From Novice to Expert and Bondy’s (1983) ‘skills escalator’ are examples of commonly used assessment strategies. Other universities may have an ‘achieved’ or ‘not achieved’ system. The NMC stipulated that this is not a sufficiently robust method and all pre-registration nursing providers will be expected to introduce a rigorous clinical assessment strategy, in which to measure the NMC Competencies.
Bondy (1983) (Fig. 6.1) uses four levels of achievement, and as students progress through their placements, they have minimum levels to achieve from 1–4. They can, however, meet a higher level in some outcomes or competencies if their mentor assesses they are working at that level. In each placement, they must meet the minimum level or the outcome/competency is not achieved. The levels are indicated in the ongoing achievement record on the corresponding ‘assessment results’ sheet for that semester. The level achieved for each outcome/competency should be recorded rather than merely a tick in the box.
Planning and preparation are competencies in their own rights and, as well as being essential to starting any new placement, learning these organisational and prioritising skills will be worthwhile throughout your training and in your professional role as a registered nurse. Levett-Jones and Bourgeois (2007) offer excellent advice and guidance for students prior to, during and after placements.
Roberts (2010) outlines key things you can do to prepare before starting a clinical placement. These include making sure you attend your planned clinical skills and simulated learning sessions and also, if an opportunity is planned into the timetable, undertaking some additional practice in the clinical skills classroom, either on your own or with a colleague (make sure your skills tutors are aware that you are doing so).
A good example is the online clinical skills resource written by Docherty and McCallum (2009), available at:
http://www.oup.com/uk/orc/bin/9780199534456/01student/checklists/(accessed May 2011)
http://www.nottingham.ac.uk/nursing/practice/ (accessed November 2011).
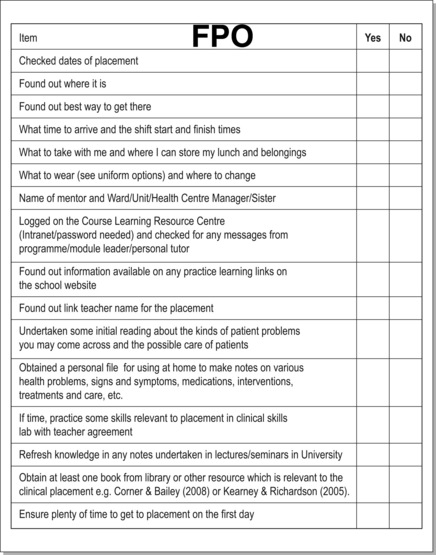
A good way to dispel your fears is to make contact with your placement area. Many universities have placement details on the internal Web pages and this can be a good starting point for finding out about the area. Phone or e-mail the placement and arrange to speak with your mentor. You may use the placement checklist in Figure 6.2 to remind you of things to find out or do before starting your placement.
An induction may include the following:
• Introduction to the placement and overview of the services offered.
• Chemotherapy and radiotherapy overview and safety features.
• Understanding spiritual distress in patients and the impact on the professional team.
• Opportunity to meet members of the wider multidisciplinary team, for example the chaplain and practice placement staff.
• Opportunity to explore areas of concern and personal feelings of anxiety.
What to expect in the first week
Within the first week
• Ward routines: visiting times; rest hour; protected meal times arrangements; meal times.
• What learning resources are available in the area: access to specialist resources; can resources be borrowed?
• Multidisciplinary team members in the clinical area: list their names and roles.
• Infection control policies: are flowers allowed in the area? What are the handwashing/rub facilities for visitors?
Mapping your own learning needs to NMC competencies
You will probably be undertaking either a programme of study where the course is clearly divided into a 1-year common foundation programme (CFP) and a 2-year branch programme, or one where there is no CFP and branch evident but still requires a programme of study which enables you to achieve outcomes (NMC 2010) which are field specific (adult, child, mental health and learning disability nursing).
Regardless of which NMC outcomes you are having to achieve on this placement, the principles remain the same. You must adhere to both the Guidance on Professional Conduct (NMC 2009) and The Code: Standards of Conduct, Performance and Ethics for Nurses and Midwives (NMC 2008). It is very important that you read these and discuss them with your personal tutor before undertaking placement learning and also your mentor when you meet for the first time.
Learning about the team
As well as being supported by a named mentor, there will be a number of other qualified nurses (now known as registrants) and other healthcare workers and professionals who will help facilitate your learning and will contribute to assessing your knowledge and skills while on placement. It is important for you to consider the specific roles and responsibilities of these individuals. This is covered in Chapter 7.
Key roles linked to student learning in practice
The mentor
Every student who is allocated by their university to gain a clinical placement learning experience has to have a named mentor who will be their main facilitator of learning, supervisor and assessor of their practice (mandatory requirement of the NMC 2008). All mentors should be experienced nurses who will have completed a course of mentorship preparation or have an equivalent qualification in their own field which is recognised as being appropriate to supervise and assess student nurses in practice (this latter individual will only be able to undertake the mentor role in specific placements and not at the major progression points within the new NMC (2010) guidance for curriculum delivery). Your mentor will be responsible for assessing your learning and competence in practice and your practice assessment document, as well as completing and signing your ongoing record of achievement (ORA) (Box 6.1), sometimes known as ongoing achievement record (OAR) (NMC 2007).
Box 6.1 Roles and expectations of you as the student and your mentor in relation to the assessment (ongoing record of achievement (ORA))*
The assessment process
Week 1
1. Student MUST negotiate with their mentor a time for their initial interview to discuss learning needs and goals and agree an action plan for achievement.
2. Student MUST share with their mentors their ORA from any previous placements and any action plans resulting from their last assessment of learning in practice.
3. Student will ensure that mentors are aware of any non-practice assessments they need to complete which may require their support for achieving, such as a client-focused assessment or evidence-based practice on a placement-specific topic.
4. Student may also have additional practice-based assessments to achieve in the placement, such as medicine management, handwashing skills or (ward/patient care) management.
Mid-point placement experience
5. Student and mentor will ensure that they meet to discuss progress at some point half way through their placement experience and also to determine if any actions from previous placement (ORA information) are being achieved. Evidence of progress will be gathered from a range of sources, including student skills record/practice assessment documents, other qualified nursing staff (registrants) and other health workers in direct contact on a regular basis with the student.
6. Student MUST receive constructive feedback from their mentor at this point and also on an ongoing basis. The mentor must ensure that the student is being taught new skills and gaining new knowledge through ongoing evaluation of learning and any deficit from their original agreed action plan can be re-negotiated if required. This mid-point meeting is an essential one for the student who may require additional support from their mentor to achieve successful completion of their practice assessment in this placement.
Final placement period
7. Student and mentor MUST meet during their final week of placement. (The importance of this final placement assessment will be critical for those students in their final placement as their practice will be required to be assessed by the ‘sign off’ mentor’). All evidence must be available about their progress on the placement and all documents available for discussion and signatures. Self-evaluation may be required as part of their practice assessment documents.
8. It is at this stage that the student has to offer clear evidence that they have achieved their goals, met the required NMC Competencies for the placement and a record made of their overall performance during their placement.
9. Ongoing record of practice assessment may either indicate level of achievement (such as the Bondy skills escalator, discussed earlier) as assessed by the mentor, or a simple assessment of:
10. Student and mentor discuss the outcomes and agree subsequent actions according to university policies.
The sign off mentor
The role of the sign off mentor is to ‘sign off’ a student’s competence against the NMC standards at the end of their NMC approved programme (Levett-Jones & Bourgeois 2007). This role is undertaken in the final placement only, but this decision will be influenced by the decisions of previous mentors who have recorded and approved the student’s progress in their ORA in the previous placements. These mentors, as noted above, are critical to the assessment of the student’s ‘fitness to practise’ as a safe and effective qualified nurse, and they are responsible and accountable for providing the evidence on which the ‘sign off ‘ mentor makes their final assessment. To be a sign off mentor, the qualified nurse must have undertaken a further course beyond that of mentorship.
The practice education facilitator
Please refer to the full NMC guidance on issues of confidentiality and access to your ORA:
www.nmc-uk.org/Documents/Circulars/2007circulars/NMC%20circular%2033_2007.pdf (accessed May 2011).
In some areas there are practice education facilitators; this is a relatively new role in practice education. These facilitators provide support for mentors and act as a link between mentors and colleagues in universities (Carlisle et al 2009).
Link teacher
The link teacher role was introduced to strengthen links between education and service areas when nursing education was transferred into the higher education sector in the UK. Initially this role was key to the successful development of the learning environment in clinical practice, working with ward managers and mentors to develop placement learning opportunities and experiences for students as well as ensuring their quality. Of late, this role has become less visible but the link teacher still has a key role to play in ensuring that the areas which they link with support student learning (Arkell & Bayliss-Pratt 2007). You can check the identity of your placement link tutor through the placement learning information on your university Website and also when you arrive in your allocated placement.
The link teacher in many areas works closely with the practice education facilitators in ensuring good learning experiences for students, and some still retain ‘hands on’ clinical care and case loads. Some are also employed as lecturer–practitioners by NHS organisations, where they work half time in the university and half time in a clinical specialty (Buchan et al 2009)
The personal tutor
It is expected that all students are allocated a personal tutor, normally from their own field of practice such as mental health, learning disability, adult or children and young people’s nursing. Por and Barriball (2008:100) highlight that lecturers who undertook this role provided a range of activities from the ‘provision of pastoral care and acting as a referral agent to other services such as student support networks, to monitoring student progress and giving academic support when required’. The main type of support that most students required was linked to these issues.
Range of clinical skills available
There will be a variety of clinical skills including the essential skills clusters you can learn and become more confident in while on this placement. There will be opportunity to gain and develop general skills and experience in communication, decision making, leadership, nursing handover, discharge planning, referrals to other professionals and the ward round. These skills are transferable and you will take these into future clinical areas. They are revisited in Section 3.
Box 6.2 highlights some of the clinical skills you may undertake.
 General assessment of the patient
General assessment of the patient
 Prioritising planning and evaluating care
Prioritising planning and evaluating care
 Risk assessment: patient and environment
Risk assessment: patient and environment
 Subcutaneous injection technique
Subcutaneous injection technique
 Cannula care and extravasation management
Cannula care and extravasation management
 Care of central venous access lines
Care of central venous access lines
 Assessment and management of nausea and vomiting
Assessment and management of nausea and vomiting
 Assessment and management of pain
Assessment and management of pain
 Nutritional assessment (including body mass index)
Nutritional assessment (including body mass index)
Pick two skills from Box 6.2 that you feel confident in doing. Consider what experience you have had that has helped this confidence.
Ways of developing your confidence
If you feel confident and competent to teach another student, agree a learning goal with your mentor to do this and, don’t forget – make it ‘SMART’: specific, measurable, achievable, realistic and timely! (Fowler 1998:77.)
For example, you could teach a first year student nurse how to perform oral assessment or explain the World Health Organisation’s pain ladder (Box 6.3).
Box 6.3 World Health Organisation’s pain ladder
Specific – focuses on a very specific topic.
Measurable – it can be tested by question and answers to see how much the student understands about the assessment tool and process and by how the student performs the task.
Achievable – this is cancer/palliative care with patients who are experiencing different levels of pain. Explain to the first year student how the WHO ladder works. Remember not to over load them with information, instead relate the tool to a patient they have been caring for.
Realistic – you may have been given a lecture and participated in a seminar at university about teaching others, and if this is your second or third year you should have more than a basic knowledge of what is required.
Timely – it can be achieved in the student’s placement experience regardless of length and you will be able to see impact of your teaching.
Expectations of being a student in practice placement
Professional conduct and behaviour: Fitness to practice
The full guidance can be found at:
http://www.nmc-uk.org/Students/Guidance-for-students/ (accessed November 2011).
http://www.nmc-uk.org/Nurses-and-midwives/Have-you-signed-up-for-the-NMC-newsletter/ (accessed November 2011).
http://www.nmc-uk.org/Students/Good-Health-and-Good-Character-for-students-nurses-and-midwives/ (accessed November 2011).
We hope that by now you are looking forward to this placement and feel you have really started to learn what it is about and what you might experience. Chapter 7 explores the cancer/palliative placement in more depth, helping to identify specific learning opportunities.
Arkell S., Bayliss-Pratt L. How nursing students can make the most of placements. Nursing Times. 2007;103(20):26–27.
Benner P. From novice to expert: excellence and power in clinical nursing practice. California: Addison-Wesley; 1984.
Bondy N.K. Criterion referenced definitions for rating scales in clinical education. Journal of Nursing Education. 1983;22(9):376–382.
Buchan J., O’May F., Little L. Review of models of employment for nursing roles which bridge practice and education: a report for NHS Scotland. NHS, Scotland: Project Report; 2009.
Carlisle C., Calman L., Ibbotson T. Practice based learning: the role of the Practice Education Facilitator in supporting mentors. Nurse Education Today. 2009;29(7):715–721.
Corner J., Bailey C. Cancer nursing: care in context, 2nd ed, Oxford: Wiley-Blackwell, 2008.
Docherty C., McCallum J.. Foundation clinical nursing skills. Online. Available at: Oxford:Oxford University Press ;2009. http://www.oup.com/uk/orc/bin/9780199534456/01student/checklists/ (accessed November 2011)
Fowler J. cited in Levett-Jones T, Bourgeois S (2009) The clinical placement: a nursing survival guide, 2nd ed. Edinburgh: Baillière Tindall; 1998.
Kearney N., Richardson A. Nursing patients with cancer: principles and practice. Edinburgh: Churchill Livingstone; 2005.
Levett-Jones T., Bourgeois A. The clinical placement: an essential guide for nursing students. Sydney: Churchill Livingstone; 2007.
Nursing and Midwifery Council. Ensuring continuity of practice assessment through the ongoing achievement record. Index Number: NMC Circular 33/2007. Online. Available at:. 2007. http://www.nmc-uk.org/Documents/Circulars/2007circulars/NMC%20circular%2033_2007.pdf (accessed May 2011)
Nursing and Midwifery Council. The code: standards of conduct, performance and ethics for nurses and midwives. Online. Available at:. 2008. http://www.nmc-uk.org/Nurses-and-midwives/The-code/The-code-in-full/ (accessed May 2011)
Nursing and Midwifery Council. Guidance on professional conduct for nursing and midwifery students. Online. Available at:. 2009. http://www.nmc-uk.org/Documents/Guidance/Guidance-on-professional-conduct-for-nursing-and-midwifery-students-September-2010.PDF (accessed May 2011)
Nursing and Midwifery Council. Standards for pre-registration nursing education. Online. Available at:. 2010. http://standards.nmc-uk.org/Pages/standards-download.aspx (accessed May 2011)
Por J., Barriball L. The personal tutor’s role in pre-registration nursing education. British Journal of Nursing. 2008;17(2):99–103.
Roberts D. Preparing you for clinical practice. In: Hart S., ed. (2010) Nursing: study and placement learning skills. Oxford: Oxford University Press; 2010:125–136.
Aston L., Wakefield J., McGowan R. The student nurse guide to decision making in practice. Maidenhead: Open University Press; 2010.
Davis N., Clark A., O’Brien M., et al. Learning skills for nursing students. Exeter: Learning Matters; 2011.
Nursing and Midwifery Council. Standards to support learning and assessment in practice. Online. Available at:. 2006. http://www.nmc-uk.org/Documents/Standards/nmcStandardsToSupportLearningAndAssessmentInPractice.pdf (accessed May 2011)