Basics of medical therapy
The treatment of skin disease includes topical, systemic, intralesional, radiation and surgical modalities. Specific treatments are detailed below. First is an overview of dermatological therapies.
Topical therapy
Topical treatment has the advantage of direct delivery and reduced systemic toxicity. It consists of a vehicle or base, which often contains an active ingredient (Table 1).
| Drug | Indications | Pharmacology |
|---|---|---|
| Corticosteroids | Eczemas, psoriasis, lichen planus, discoid lupus erythematosus, sunburn, pityriasis rosea, mycosis fungoides, photodermatoses, lichen sclerosus | Mode of action is through vasoconstrictive, anti-inflammatory and antiproliferative effects; medication is available in different strengths; side-effects need to be considered |
| Antiseptics | Skin sepsis, leg ulcers, infected eczema | Chlorhexidine, benzalkonium chloride, silver nitrate and potassium permanganate are used |
| Antibiotics | Acne, rosacea, folliculitis, impetigo, infected eczema | Chlortetracycline, neomycin, bacitracin, gramicidin, polymixin B, sodium fusidate and mupirocin; resistance and sensitization are problems Metronidazole is used for rosacea |
| Antifungals | Fungal infections of the skin, Candida albicans infections | Nystatin, clotrimazole, miconazole, econazole, terbinafine, ketoconazole, sulconazole and amorolfine |
| Antiviral agents | Herpes simplex, herpes zoster | Aciclovir, penciclovir |
| Parasiticidals | Scabies, lice | Benzyl benzoate, permethrin and malathion for scabies; malathion, permethrin and phenothrin for lice – applied as a lotion or shampoo |
| Coal tar | Psoriasis, eczema | Presumed anti-inflammatory and antiproliferative effects; available as creams, shampoos and in paste bandages |
| Dithranol | Psoriasis | Antiproliferative effects; available as creams, pastes and ointments |
| Vitamin D analogues | Psoriasis | Calcitriol, calcipotriol and tacalcitol inhibit keratinocyte proliferation and promote differentiation |
| Keratolytics | Acne, scaly eczemas | Salicylic acid, benzoyl peroxide and tretinoin |
| Retinoids | Acne, psoriasis | Isotretinoin (acne), tazarotene (psoriasis) |
| Topical immunomodulators (calcineurin inhibitors) | Atopic eczema (and off-licence use in other diseases) | Tacrolimus and pimecrolimus |
Vehicles are defined as follows:
 Lotion. A liquid vehicle, often aqueous or alcohol based, which may contain a salt in solution. A shake lotion contains an insoluble powder (e.g. calamine lotion).
Lotion. A liquid vehicle, often aqueous or alcohol based, which may contain a salt in solution. A shake lotion contains an insoluble powder (e.g. calamine lotion).
 Cream. A semisolid emulsion of oil-in-water; contains an emulsifier for stability and a preservative to prevent overgrowth of micro-organisms.
Cream. A semisolid emulsion of oil-in-water; contains an emulsifier for stability and a preservative to prevent overgrowth of micro-organisms.
 Gel. A transparent semisolid, non-greasy aqueous emulsion.
Gel. A transparent semisolid, non-greasy aqueous emulsion.
 Ointment. A semisolid grease or oil, containing little or no water but sometimes with added powder. No preservative is usually needed. The active ingredient is suspended rather than dissolved.
Ointment. A semisolid grease or oil, containing little or no water but sometimes with added powder. No preservative is usually needed. The active ingredient is suspended rather than dissolved.
 Paste. An ointment base with a high proportion of powder (starch or zinc oxide) producing a stiff consistency.
Paste. An ointment base with a high proportion of powder (starch or zinc oxide) producing a stiff consistency.
Therapeutic properties of the vehicle
Lotions evaporate and cool the skin and are useful for inflamed or exudative conditions, e.g. for wet wraps (p. 37). The high water content of a cream means that it mostly evaporates; it is also non-greasy and easy to apply or remove. Ointments are best for dry skin conditions such as eczema. They rehydrate and occlude, but being greasy are difficult to wash off and are less acceptable to patients than creams. Pastes are ideal for applying to well-defined surfaces, such as psoriatic plaques, but are also hard to remove.
Quantities required
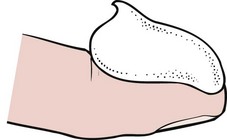
One application to the whole body requires 15–20 g of ointment. The adult face or neck requires 1 g, trunk (each side) 3 g, arm 0.5 g, hand 0.5 g, leg 3 g and foot 1 g. A useful guide for patients is the ‘fingertip unit’ (FTU) – the amount of cream or ointment that can be applied to the terminal phalanx of the index finger (Fig. 1). One FTU equals 0.5 g. The weekly amount required for the twice-daily use of an emollient in an adult is 250 g. Doctors often underestimate the quantities needed.
Pharmacokinetics
The ability of a drug to penetrate the epidermis depends on several factors. These include:
Dressings and hospital admission
Bandages impregnated with tar are sometimes helpful for leg ulcers and eczema. Many types of paraffin gauze, hydrocolloid and alginate dressing are now available for leg ulcers (p. 73).
Topical steroids
A summary of the indications for topical treatment with corticosteroids is given in Table 1. The relative potencies of the more commonly prescribed preparations are shown in Table 2.
| Potency | Example (generic name) | Proprietary name (UK) |
|---|---|---|
| Mild | Hydrocortisone 1% and 2.5% | Efcortelan, Mildison (U-Cort USA) |
| Moderately potent | Clobetasone butyrate 0.05%Fludroxycortide 0.0125%Alclometasone dipropionate 0.05% | Eumovate (UK and USA)HaelanModrasone (Aclovate USA) |
| Potent | Betamethasone valerate 0.1%Betamethasone dipropionate 0.05%Fluocinolone acetonide 0.025%Fluocinonide 0.05%Fluticasone propionate 0.05%Hydrocortisone butyrate 0.1%Mometasone furoate 0.1%Triamcinolone acetonide 0.1% | Betnovate (Valisone USA)Diprosone (UK and USA)Synalar (UK and USA)Metosyn (Lidex USA)Cutivate (UK and USA)Locoid (UK and USA)Elocon (UK and USA)Adcortyl (Aristocort, Kenalog USA) |
| Very potent | Clobetasol propionate 0.05%Diflucortolone valerate 0.3%Halcinonide 0.1% | Dermovate (Temovate USA)Nerisone Forte (UK and Canada)Halciderm Topical (Halog USA) |
Side-effects of topical steroid therapy
The use of topical steroids carries the potential for harmful side-effects. These include:
 atrophy of the skin – thinning, erythema, telangiectasia, purpura and striae (p. 114)
atrophy of the skin – thinning, erythema, telangiectasia, purpura and striae (p. 114)
 induction of acne or perioral dermatitis, and exacerbation of rosacea
induction of acne or perioral dermatitis, and exacerbation of rosacea
 atypical fungal infection (tinea incognito); bacterial or viral infections may be potentiated
atypical fungal infection (tinea incognito); bacterial or viral infections may be potentiated
 allergic contact dermatitis, resulting from a component of the preparation or the steroid itself
allergic contact dermatitis, resulting from a component of the preparation or the steroid itself
 systemic absorption – suppression of the pituitary–adrenal axis, Cushingoid appearance, growth retardation
systemic absorption – suppression of the pituitary–adrenal axis, Cushingoid appearance, growth retardation
 tachyphylaxis – reduced responsiveness to the steroid after prolonged use.
tachyphylaxis – reduced responsiveness to the steroid after prolonged use.
Systemic therapy
Systemic treatments are used when topical treatment is ineffective, for serious skin diseases and for infections. Details are given in Table 3.
| Group | Drug | Indications |
|---|---|---|
| Corticosteroids | Prednisolone usually | Bullous disorders, connective tissue disease, vasculitis |
| Cytotoxics | MethotrexateHydroxycarbamideAzathioprine, mycophenolate mofetil | Psoriasis, sarcoidosis, eczemaPsoriasisBullous disorders, chronic actinic dermatitis, atopic eczema |
| Biologics | Etanercept, infliximab, adalimumab, ustekinumab | Psoriasis unresponsive to other systemic agents, off-licence use in other diseases (p. 33) |
| Immunosuppressants | CiclosporinGold | Psoriasis, atopic eczema, pyoderma gangrenosumBullous disorders, lupus erythematosus |
| Retinoids | AcitretinIsotretinoinAlitretinoin | Psoriasis, other keratinization disordersAcneHand dermatitis |
| Antifungals | Griseofulvin, terbinafineKetoconazoleItraconazole, fluconazole | Fungal infectionFungal infection (Candida aIbicans too)Fungal infection, candidiasis |
| Antibiotics | Various | Skin sepsis, acne, rosacea |
| Antivirals | Aciclovir, valaciclovirFamciclovir | Herpes simplex, herpes zosterHerpes zoster, genital herpes simplex |
| Antihistamines | H1 blockers | Urticaria, eczema |
| Antiandrogens | Cyproterone acetate | Acne (females only) |
| Antimalarials | Hydroxychloroquine | Lupus erythematosus, porphyria cutanea tarda |
| Antileprotic | Dapsone | Dermatitis herpetiformis, leprosy, vasculitis |
Other treatments
Corticosteroids are sometimes injected directly into lesions (e.g. to treat keloids). Certain disorders respond to phototherapy (p. 47). Iontophoresis is a treatment for excess sweating of the palms in which a direct electric current is passed into skin in contact with tap water.
Cryotherapy, in which liquid nitrogen is applied to the skin, is extensively used in dermatology (p. 111). It is mainly employed for the treatment of benign or premalignant skin tumours.
Basics of medical therapy
 Correct diagnosis is essential to ensure appropriate treatment.
Correct diagnosis is essential to ensure appropriate treatment.
 Explain the treatment to the patient and preferably give a written handout; this aids compliance. The fingertip unit is a convenient way to indicate the amount of cream the patient should apply.
Explain the treatment to the patient and preferably give a written handout; this aids compliance. The fingertip unit is a convenient way to indicate the amount of cream the patient should apply.
 Use the simplest treatment possible; patients easily get mixed up if they have several different topical preparations to apply to different parts of the body.
Use the simplest treatment possible; patients easily get mixed up if they have several different topical preparations to apply to different parts of the body.
 Prescribe adequate amounts. Patients are often given too small quantities of their creams, ‘run out’ and return to the clinic no better because the treatment has been inadequate.
Prescribe adequate amounts. Patients are often given too small quantities of their creams, ‘run out’ and return to the clinic no better because the treatment has been inadequate.