Basic Principles: Radiologic Techniques and Radiation Safety 1
Radiologic Techniques in the Intensive Care Unit
Radiation Exposure and Radiation Safety
Communication, Reporting of Findings, and Teleradiology
Radiologic Techniques in the Intensive Care Unit
C. Schaefer-Prokop
Radiologic examinations in the intensive care unit (ICU) are most commonly performed at the bedside. They consist mainly of portable chest radiographs, followed by ultrasound scans. Projection radiographs of the skeleton are only rarely obtained. Much as in other clinical settings, computed tomography (CT) has assumed an expanding role in the ICU. CT scans are obtained at an increasingly early stage for addressing diagnostic problems of the chest and abdomen. This relates to the generally higher diagnostic efficiency of CT over other modalities, the capabilities of modern scanners in the detection of vascular pathology (pulmonary embolism, intestinal ischemia), and the use of CT for image-guided interventions (e. g., abscess drainage).
The following typical problems are encountered in the diagnostic imaging of ICU patients:
 Patients have limited ability to cooperate with the examiner.
Patients have limited ability to cooperate with the examiner.
 Imaging conditions are more difficult than in the radiology department (chest imaged in a supine or sitting position, limited access for ultrasound scans, etc.).
Imaging conditions are more difficult than in the radiology department (chest imaged in a supine or sitting position, limited access for ultrasound scans, etc.).
 Radiographic interpretation is often hampered by superimposed foreign materials (dressings, metal implants, catheters, tubes, wires).
Radiographic interpretation is often hampered by superimposed foreign materials (dressings, metal implants, catheters, tubes, wires).
 Radiographic equipment is frequently limited (portable radiography machine), and images are obtained without automatic exposure control.
Radiographic equipment is frequently limited (portable radiography machine), and images are obtained without automatic exposure control.
 If the patient is taken to the radiology department (e. g., for CT, MRI, DSA), the gain in diagnostic information must be weighed against the increased risk of transporting the patient.
If the patient is taken to the radiology department (e. g., for CT, MRI, DSA), the gain in diagnostic information must be weighed against the increased risk of transporting the patient.
Radiographic Equipment
The following basic radiological equipment should be available in the ICU:
 a portable radiography machine
a portable radiography machine
 storage phosphor cassettes, or cassette-based direct detectors with a 35 × 43 cm format—may be used as a grid-film cassette or with a Bucky device for inserting standard film cassettes
storage phosphor cassettes, or cassette-based direct detectors with a 35 × 43 cm format—may be used as a grid-film cassette or with a Bucky device for inserting standard film cassettes
 radiation protection aprons (lead equivalency of 0.25–0.5 mm) and protective gloves
radiation protection aprons (lead equivalency of 0.25–0.5 mm) and protective gloves
 portable radiation screens for some applications
portable radiation screens for some applications
 viewboxes or video monitors for viewing images (large enough for viewing and comparing two or three large-format films)
viewboxes or video monitors for viewing images (large enough for viewing and comparing two or three large-format films)
 ultrasound scanner with documentation system
ultrasound scanner with documentation system
The number of radiography machines and the scope of accessory equipment will depend on the number of ICU beds and on special hygienic requirements. Larger units and suites should be equipped with their own film processor or digital reader device. A portable fluoroscopy machine with its own table should be available in a separate examination room. Portable CT scanners have been tested under study conditions but have not come into practical use due to technical limitations.
Conventional Film–Screen Radiography
Conventional film–screen radiography has been replaced by digital radiography in almost all ICUs and is mentioned here only for completeness. A conventional cassette contains the x-ray film and a pair of intensifying screens placed at the front and back of the cassette. These film–screen combinations are characterized by their spatial resolution and dose requirement, which determine the speed rating of the system (50, 100, 200, 400, 800, or 1600). Faster systems require a lower radiation dose but also sacrifice some degree of spatial resolution. Film– screen combinations with a speed rating of 400 (“400 systems”) are used for radiographs in ICU patients and for most applications in emergency medicine, while 100 or 200 systems are used only in the evaluation of limb injuries (traumatology). Imaging with a scatter-reduction grid provides higher image quality than filming without a grid. While the use of a grid requires a higher exposure level (dose is generally increased by a “grid factor” of 2–3), this can be partially offset by using a higher tube voltage (120 kV instead of 80 kV for chest films).
Digital Radiography
Digital radiography has become the mainstay for image acquisition and documentation in ICUs and emergency rooms owing to its technical advantages.
The advantages of digital technology relate to organizational aspects (digital data format with capabilities for data transfer and image distribution to multiple users) and its lack of sensitivity to underpenetration and poor contrast due to exposure errors. These advantages are based on the digital data format, image processing including automated signal normalization, and the greater dynamic range of digital detectors compared with x-ray film.
Computed radiography (CR), or storage phosphor radiography, is the current standard in intensive care radiology. Mobile flat-panel or direct radiography (DR) systems have recently become available in the 35 × 43 cm format. The advantage of DR is the greater dose efficiency of the system, which permits ca. 50% dose reduction during the examination.
Computed radiography. CR (Fig. 1.1a) is comparable in its handling to a daylight system. It is a cassette-based system that requires a special reader device. The detector consists of a photostimulable storage phosphor plate housed in an aluminum cassette. After the plate has been exposed, the cassette is placed into the reader. The radiographic image can either be printed on film (hard copy) or displayed on a video monitor (soft copy).
Direct detector units. Direct detector units (Fig. 1.1b) consist of the imaging cassette, which contains the detector and is hardwired to the readout unit by an electric cable. This means that the technician must take the readout unit to the patient’s bedside along with the rest of the system, which will naturally affect workflow and organizational details. The advantage of DR over CR is its higher dose efficiency, which allows for a significant dose reduction (30–50%, depending on the patient’s condition). Another advantage is the direct availability of the image on the readout unit, which provides immediate feedback on imaging parameters.
Fig. 1.1 a, b Equipment for digital radiography.
a Computed radiography.
b Flat-panel system for direct radiography.
Radiation Exposure and Radiation Safety
A. Stadler
Issues of medical radiation safety are rarely a priority concern in emergency and ICU patients, even though the patients may be exposed to considerable dose levels. One problem is that trauma patients in particular must often undergo comprehensive imaging protocols that involve high individual doses during the acute phase of treatment. Another problem is that even low individual doses per examination may well produce a significant cumulative exposure when continued over a period of weeks.
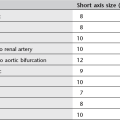
Radiation Exposure to Patients and Staff
The supine anteroposterior (AP) chest radiograph is the most common imaging examination in the ICU, especially in patients on long-term ventilation. More than 100 radiographs may be taken during a prolonged stay in the ICU. While various dose values have been reported in the literature, the effective dose in all cases was less than 0.2 mSv per radiograph. CT examinations expose patients to significantly higher effective dose values than chest radiographs (Table 1.1). The values listed in the table are only approximations, however, as the effective dose depends strongly on equipment and examination parameters.
Assessment of Patient Risk
A portable chest radiograph generally exposes the patient to more radiation than a film taken on a wall-mounted cassette holder, depending on the selected parameters (Table 1.2). This is due mainly to the shorter film–focus distance (FFD) at the bedside and the use of an AP rather than posteroanterior (PA) projection (increasing the effective dose to females by a factor of 1.9, to males by a factor of 1.6). The dose increase associated with the use of a scatter-reduction grid (grid cassettes) can be partially offset by a higher kilovoltage setting.
The risk coefficients defined by the ICRP (International Commission on Radiological Protection) in 1991 are useful for estimating the bioeffects of radiation. The likelihood that a 30-year-old individual will develop a radiation-induced malignancy is estimated at 5% per sievert(4.5%/Sv for solid cancers, 0.5%/Sv for leukemia; ICRP 60; see also Table 1.5). The latent period for developing leukemia is ca. 15 years compared with 40 years for other malignant diseases. This latent period is a particular concern in older individuals. Based on the above percentages, an ICU patient who receives 100 chest radiographs (total dose of 0.02 Sv based on single doses of 20 μSv) will have an additional 0.1% risk for developing a malignant disease (Table 1.3). Since approximately one in four people will develop a malignancy during their lifetime, the chest radiographs in the above example will increase the risk from 25% to 25.1%.
Thus, even in a setting of long-term intensive care involving multiple radiographic examinations, the patient will not face a significant additional cancer risk, especially when we consider the severity of the condition for which the patient is receiving intensive care.
Radiation Exposure during Pregnancy
Acute illness or injury in a pregnant woman, while rare, is a challenging management problem. One aspect of the problem concerns the use of roentgen rays and the resulting radiation exposure to the embryo or fetus. Antenatal exposure to ionizing radiation can potentially lead to two types of pathology: malignancies and malformations.
|
Type of examination |
Typical effective dose |
|
PA chest radiograph |
0.025 mSv |
|
AP chest radiograph |
0.06 mSv |
|
AP abdominal radiograph |
1 mSv |
|
Cranial CT |
2.3 mSv |
|
Thoracic CT |
8 mSv |
|
Abdominal/pelvic CT |
10 mSv |
|
Radiologic examinations |
Total dose |
Risk of a malignant disease |
|
20 Chest radiographs |
4 mSv |
0.02% |
|
5 Abdominal radiographs |
5 mSv |
0.025% |
|
3 Cranial CTs |
6.9 mSv |
0.0345% |
|
5 Thoracic CTs |
40 mSv |
0.2% |
|
5 Abdominal CTs |
50 mSv |
0.25% |
Malformations. It is generally agreed that antenatal radiation exposure must exceed a threshold value to induce malformations. Exposure below the threshold is not considered harmful, while exposure above the threshold within a certain time window (2nd to 15th week of gestation) may cause a developmental abnormality. The exact threshold is difficult to define, but a value of 100 mGy is generally assumed. Because the fetal dose from a single examination tends to be well below 50 mGy, even high-dose examinations should not cause fetal harm. As an example, one of the most common emergency examinations in pregnant patients, the CT detection of pulmonary embolism, will deliver a fetal dose less than 0.2 mGy. This dose is several orders of magnitude below the threshold value.
Management after radiation exposure. In pregnant women who have undergone a radiographic examination, it is often appropriate to ask whether pregnancy termination is necessary or should at least be considered, especially in cases where the pregnancy is not detected until after the examination. A three-stage concept should be used for assessing the level of exposure and deciding on further management:
1. Tables are used initially to make a gross estimate of the radiation dose to the uterus. If the gross estimate is less than 20 mSv, the physician indicates this in the patient’s record and notes also that there is no radiologic indication for terminating the pregnancy.
2. If the gross estimate exceeds 20 mSv, the dose should be estimated more precisely by taking into account the imaging technical parameters, equipment data, and patient data. If the revised estimate is less than 100 mSv, this is noted in the patient’s record. The patient is informed of the result, and again the physician does not recommend pregnancy termination.
3. If the estimate exceeds 100 mSv, the dose is calculated as accurately as possible based on all available information. If this confirms that the exposure exceeded 100 mSv, the physician consults with the patient and weighs the risk of continuing the pregnancy against the patient’s desire to have a child. Given the risks involved, the physician would support a desire to terminate the pregnancy. If the calculated exposure exceeds 200 mSv, the physician will usually recommend termination.
|
Low-dose examinations |
High-dose examinations |
|
Radiography of the limbs |
Pelvic radiography |
|
Chest radiography |
Abdominal radiography |
|
Thoracic CT |
Abdominal CT |
|
Cranial CT |
Abdominal fluoroscopy |
Again, it should be emphasized that below a uterine threshold dose of 100 mSv, the expectant mother may be assured that all emergency (noninterventional) radiologic examinations are safe. In all cases the imaging parameters should be documented in full detail. Ideally, patients should be given a dosimeter, especially in combined or interventional procedures, so that an accurate retrospective determination of uterine dose can be made with the help of a medical physicist.
There is no evidence that the use of nonionic contrast media poses a hazard to the fetus or embryo.
High-dose and low-dose examinations. Emergency radiologic examinations can be conveniently divided into high-dose and low-dose examinations (Table 1.4). Low-dose examinations may be performed without concern, whereas high-dose examinations should be based on rigorous patient selection criteria and should be weighed against alternative modalities (ultrasonography, MRI).
Radiation Exposure in Children
Children should be considered separately in the evaluation of radiation-induced risks. On the one hand, children are more radiosensitive than adults. For any given dose, the risk of developing a radiation-induced malignancy is several times higher in a newborn than in an adult (Table 1.5). Another consideration is that for any given examination such as cranial CT, the effective dose to a pediatric patient will be several times higher than the dose to an adult. As an example, the statistical risk of abdominal CT in a 1-year-old child is of the order of one induced cancer per 1000 examinations—a risk that is by no means negligible.
CT scans are most likely to cause significant radiation exposure in emergency radiology, especially during abdominal examinations. By comparison, the exposure from conventional radiographs is several orders of magnitude less. This emphasizes the importance of modifying the scan protocols in CT for dose optimization.
|
Age |
Risk (deaths/mSv) |
|
Newborn (4 weeks) |
18/100 000 |
|
Small child (2 years) |
13/100 000 |
|
Child (7 years) |
10/100 000 |
|
Adolescent (14 years) |
7.5/100 000 |
|
Adult (30 years) |
6/100 000 |
|
Adult (60 years) |
2.5/100 000 |
|
Adult (80 years) |
1.5/100 000 |
|
Average |
5/100 000 |
|
Age |
% of adult mAs dose |
|
< 6 months |
25 |
|
6 months to 3 years |
40 |
|
3–6 years |
65 |
|
> 6 years |
100 |
|
Body weight (kg) |
% of adult mAs dose |
|
|
|
Abdomen |
Chest |
|
< 15 |
15 |
15 |
|
15–24 |
25 |
25 |
|
25–34 |
40 |
35 |
|
35–44 |
60 |
50 |
|
45–54 |
80 |
75 |
|
< 54 |
100 |
100 |
The original dose can be reduced by almost half by decreasing the tube voltage to 80–100 kV. The smaller diameter of pediatric patients compared with adults allows for a significant reduction of the mAs while maintaining an acceptable signal-to-noise ratio (Tables 1.6, 1.7). Equipment manufacturers have offered increasingly optimized protocols in recent years. Regardless of this, it is absolutely essential to select patients carefully and to use alternative modalities (ultrasonography, MRI) whenever possible, especially in the pediatric age group.
Principles of Dose Reduction to Staff
The best way to avoid radiation exposure to staff is by following the distance squared law. For example, the radiation dose from laterally directed scattered radiation may equal 2 μGy at a distance of 1 m from the source, but falls to 0.5 μGy at a distance of 2 m. Thus, doubling the distance reduces the radiation dose by 75%.
The effect of lead aprons can be assessed in terms of their lead equivalency, which is indicated on the apron. An apron with a lead equivalency of 0.1 mm will reduce the radiation dose by half, while a value of 0.4 mm will reduce the dose by 90%.
Further dose reduction can be achieved by using lead screens in conjunction with the portable radiography machine.
Assessment of Risk to Staff
Various studies performed in ICUs and emergency rooms have consistently shown that even without a lead apron, staff exposure is reduced to a negligible level by keeping a minimum distance of ca. 1.5 m from the radiation source. When this rule is followed in the ICU, there is no need to interrupt nursing actions or medical procedures when a patient is admitted to the adjacent bay. At a distance of 3 m, the scattered radiation from a bedside chest radiograph is no greater than one hour’s exposure to natural environmental background radiation.
Regarding protection from scattered radiation when patients are admitted to the same room, regulations state that only cross-table projections require the use of a portable lead screen (while also maintaining a minimum distance of 1.5 m from the source tube).
Typical extrapolated values for nursing staff are less than 0.1 mSv/year. This is less than 10% of the permissible dose, which is 1 mSv/year for the general population, and less than 5% of the natural background radiation dose of 2.4 mSv/year. Studies performed in neonatal ICUs have indicated even lower levels of radiation exposure to nursing staff, other patients, and visitors.
Dose Reduction in Computed Tomography
The volume CT dose index (CTDIvol) is the most important radiation dose measure used in designing protocols for CT examinations. The CTDIvol indicates the average local dose within the scanned volume and is directly displayed on most modern scanners. It permits an immediate assessment of the relative dose delivered by the selected scanning protocol. The effect of technical factors such as pitch, mAs, kV, filtering, etc. is already included in the index. The dose-length product (DLP) also takes into account the scan length. This means that standard CT scanning protocols can be modified for dose optimization by documenting the dose indices displayed on the scanner and evaluating the diagnostic accuracy that is obtained. The approximate effective patient dose can be estimated by using “conversion factors” that additionally take into account the anatomical region that is scanned.
The following parameters are essential in achieving the desired dose reduction in CT:
 number of passes (biphasic studies, delayed scans)
number of passes (biphasic studies, delayed scans)
 scan length (preferably limited to the region of interest)
scan length (preferably limited to the region of interest)
 Patient dose is directly proportional to mAs. But as the mAs is decreased, image noise increases correspondingly. Often the mAs can be significantly reduced in thin patients and children compared with standard protocols.
Patient dose is directly proportional to mAs. But as the mAs is decreased, image noise increases correspondingly. Often the mAs can be significantly reduced in thin patients and children compared with standard protocols.
 The CTDI depends on the tube current. Reducing the voltage from 120 to 80 kV decreases the CTDI by a factor of 2.2. It is advisable to use a high kilovoltage, however, when scanning regions of high radiographic density in obese patients.
The CTDI depends on the tube current. Reducing the voltage from 120 to 80 kV decreases the CTDI by a factor of 2.2. It is advisable to use a high kilovoltage, however, when scanning regions of high radiographic density in obese patients.
 Greater slice thicknesses result in less image noise and allow for a reduction in mAs.
Greater slice thicknesses result in less image noise and allow for a reduction in mAs.
 Imaging with soft kernels will also reduce image noise, allowing for lower mAs values.
Imaging with soft kernels will also reduce image noise, allowing for lower mAs values.
 Wherever possible, the gonads and breasts should be outside the scanned region. This can often be achieved with careful positioning technique. The gonads should be protected with a leaded rubber apron or gonad shield. It is good practice in children to protect the unscanned body region (even outside the gonads) with leaded rubber shields.
Wherever possible, the gonads and breasts should be outside the scanned region. This can often be achieved with careful positioning technique. The gonads should be protected with a leaded rubber apron or gonad shield. It is good practice in children to protect the unscanned body region (even outside the gonads) with leaded rubber shields.
Dose Reduction in Digital Radiography
Computed radiography. Digital radiographic techniques are widely used in modern ICUs. The detector used in computed radiography (CR) is a storage phosphor plate housed in a rigid cassette. The dose efficiency of these detectors has been continuously improved in recent years. The latest generation of imaging plates (Fuji ST-Vn or comparable plates from other manufacturers) requires the dose for a conventional 400-speed film and provides an image quality that is superior in many respects to conventional radiographs.
While dose reduction in CR does not underexpose the image owing to automatic contrast and density control, it does lead to increased image noise and thus poorer structural contrast, especially in high-absorption regions like the mediastinum. Increasing the dose reduces image noise but does not improve the delineation of structures (under standardized study conditions) and does not add diagnostic information. Consequently, there is no rationale for using increased dose levels in CR.
The imaging dose cannot be visually assessed on the basis of film blackening as it can in conventional radiography, but image noise in CR provides feedback that is useful for dose evaluation.
Manufacturers also offer various types of data that serve as “dose indicators” (S values in Fuji-based systems, LgM values in Agfa systems, EI values in Kodak systems). These values may be based on the histogram of image pixel values (S value), they may indicate the dose-area product (Philips), or they may indicate deviations from the average imaging dose for that body region (Agfa). Their purpose is to permit a relative dose assessment while preventing the dose level from creeping upward or downward. This is a particular hazard with bedside radiographs in the ICU, which are taken without automatic exposure control.
Direct detector systems. Flat-panel direct detector systems give a direct readout of the dose-area product in mGy (patient entrance dose). These systems have recently come onto the market, and portable models are also available. Recent publications and our own experience indicate an option for 30–50% dose reduction compared with a 400 system, without causing a significant loss of image quality. Images acquired at conventional dose levels yield better quality in the high-absorption region of the mediastinum.
Communication, Reporting of Findings, and Teleradiology
M. Walz and C. Schaefer-Prokop
Ordering Examinations and Reporting Findings
Type of order. The orders for radiology services fall into two main categories: routine and emergency.
 Routine services can be smoothly integrated into the workflow of the ICU and require a one-time coordination of the departments involved. Persons should be available in the ICU to assist with setting up the equipment or taking the radiographs; other staff members may exit the area to avoid exposure.
Routine services can be smoothly integrated into the workflow of the ICU and require a one-time coordination of the departments involved. Persons should be available in the ICU to assist with setting up the equipment or taking the radiographs; other staff members may exit the area to avoid exposure.
 Emergency orders should be performed immediately and rely on the prompt availability of necessary staff and equipment, usually furnished by the radiology department.
Emergency orders should be performed immediately and rely on the prompt availability of necessary staff and equipment, usually furnished by the radiology department.
Content. A written or electronic request for radiology services should include all patient data, the desired examination, the radiology history, and the clinical problem with up-to-date clinical information. In women of child-bearing age, the order should note an existing or possible pregnancy or confirm that pregnancy has been excluded. This information forms the basis for a clinically meaningful radiology report while providing a justified indication for the examination itself. From an organizational standpoint, it is also important to designate a physician responsible for x-ray use—someone who is present on site, available at short notice, and authorized to give instructions to the radiologic technologist. A different physician may exercise this role on different days of the week or at different times of day (e. g., a radiology department physician during routine work hours, an ICU physician at night and on weekends). If the physician making the justified indication is in the radiology department, he or she must be able to rely on the clinical information that has been provided, and so a legally valid order signed by a physician is recommended.
Clinical information. The following clinical information is relevant to the interpretation of radiologic findings:
 patient’s history and condition (level of consciousness, mechanical ventilation)
patient’s history and condition (level of consciousness, mechanical ventilation)
 nature, course, and dates of previous operations, trauma, hemorrhage, aspirations, mass transfusions, shock, or adverse drug reactions
nature, course, and dates of previous operations, trauma, hemorrhage, aspirations, mass transfusions, shock, or adverse drug reactions
 nature, course, and dates of previous endoscopies, biopsies, or catheterizations of hollow organs, body cavities, vessels, or parenchymal organs
nature, course, and dates of previous endoscopies, biopsies, or catheterizations of hollow organs, body cavities, vessels, or parenchymal organs
 acute or preexisting impairment of cardiac, renal or cerebral function
acute or preexisting impairment of cardiac, renal or cerebral function
 current values for blood-gas analysis, blood pressure, and ventilation
current values for blood-gas analysis, blood pressure, and ventilation
 previous radiographs, including radiographs taken elsewhere
previous radiographs, including radiographs taken elsewhere
Reporting of findings. The protocols for interpreting images and reporting the findings are different for routine orders and emergency orders. While joint conferences in the ICU have proven best for routine services, emergency orders require direct reporting of findings because the results may have immediate therapeutic implications. Depending on circumstances, the findings may be reported by telephone, by direct conversation, in written form, or as a voice recording if an electronic dictation system is available. Other, digital options are the use of text blocks or a speech recognition system for the rapid creation of digitized text.
Conferences. Regular joint conferences are held to review relevant historical and clinical data, discuss current findings, and consider possible further diagnostic and therapeutic actions. Interdisciplinary clinical/radiologic/pathologic conferences for retrospective case analysis and the discussion of errors are a useful tool for quality assurance and improvement.
Information sharing. The frequent low specificity of morphologic findings in the chest underscores the importance of interdisciplinary cooperation in the care of ICU patients, as the interpretation of radiologic findings is greatly influenced by an awareness of clinical parameters such as fluid balance, ventilation therapy, and inflammatory markers.
The necessary flow of information between the clinician and radiologist is most effectively maintained by conducting regular joint rounds, but should also function when needed in response to acute problem cases. Clinical information plays a crucial role in intensive-care radiography, because image analysis must take into account not only the multitude of primary pathologic processes, but also any previous therapeutic and/or diagnostic measures, which may influence the detectability of findings and will definitely affect their interpretation.
Summary
Radiologic examinations in the intensive care unit (ICU) are most commonly performed at the bedside and consist mainly of portable chest radiographs followed by ultra-sonography. Digital radiography has almost completely replaced conventional film–screen radiography in this setting. Computed radiography has become the standard in ICUs and emergency rooms, and digital radiography machines have also become available in recent years.
Portable chest radiographs are associated with higher radiation exposure than films taken on a wall-mounted cassette holder, but even numerous examinations in ICU patients will not significantly increase their cancer risk.
Pregnant patients can safely undergo low-dose examinations in an emergency, whereas high-dose examinations should be subject to rigorous selection criteria.
Staff members in the ICU can avoid significant x-ray exposure by keeping a distance of at least 1.5 m from the radiation source.
A system must be in place in ICU for the immediate implementation of emergency radiologic orders. The radiologist must be provided with clinical information that is relevant to interpreting the radiologic findings. Emergency orders require the direct reporting of findings because the results may have immediate therapeutic implications. Hospital information systems can expedite and facilitate workflow by providing an efficient framework for distributing images and radiology reports.

 Digital radiography has almost completely replaced conventional film–screen radiography in ICUs.
Digital radiography has almost completely replaced conventional film–screen radiography in ICUs. Computed radiography is the standard in ICUs and emergency rooms; digital radiography machines have also become available in recent years.
Computed radiography is the standard in ICUs and emergency rooms; digital radiography machines have also become available in recent years.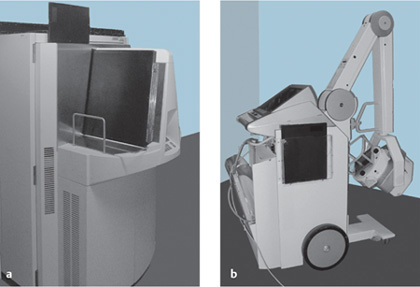
 Even numerous radiographic examinations do not pose a significant additional cancer risk in ICU patients.
Even numerous radiographic examinations do not pose a significant additional cancer risk in ICU patients. A portable chest radiograph exposes the patient to more radiation than a film taken on a wall-mounted cassette holder.
A portable chest radiograph exposes the patient to more radiation than a film taken on a wall-mounted cassette holder.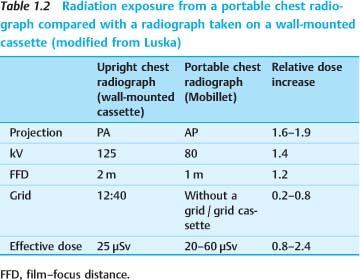
 The threshold uterine dose in pregnant patients is generally considered to be 100 mGy. Exposures below that level do not pose a risk to the fetus.
The threshold uterine dose in pregnant patients is generally considered to be 100 mGy. Exposures below that level do not pose a risk to the fetus. Low-dose examinations of pregnant patients may be performed without concern, whereas high-dose examinations should be subject to rigorous selection criteria.
Low-dose examinations of pregnant patients may be performed without concern, whereas high-dose examinations should be subject to rigorous selection criteria. Emergency abdominal CT examinations deliver the highest radiation dose to children, making it necessary to apply rigorous criteria in patient selection.
Emergency abdominal CT examinations deliver the highest radiation dose to children, making it necessary to apply rigorous criteria in patient selection. Staff members can avoid significant x-ray exposure by keeping a distance of at least 1.5 m from the radiation source.
Staff members can avoid significant x-ray exposure by keeping a distance of at least 1.5 m from the radiation source. A general dose reduction (< 400 speed) is not recommended for CR. Increasing the dose does not add diagnostic information and should be avoided.
A general dose reduction (< 400 speed) is not recommended for CR. Increasing the dose does not add diagnostic information and should be avoided. A system must be in place for the immediate implementation of emergency radiology orders in the ICU.
A system must be in place for the immediate implementation of emergency radiology orders in the ICU. A radiology report has high “evidential value” only when validated by a handwritten or digital signature.
A radiology report has high “evidential value” only when validated by a handwritten or digital signature.