Bartholin Duct Cyst and Abscess
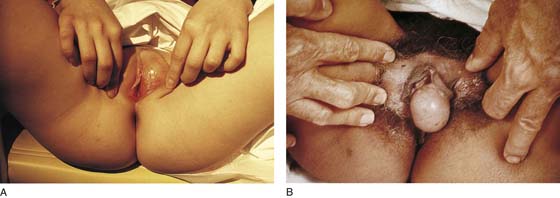
Frequently, gynecologists refer to obstruction of the Bartholin duct as a Bartholin gland cyst. The obstruction usually occurs at the surface (vestibule), and secretion of mucus by the gland leads to progressive dilation of the closed-off duct. As a consequence, the ballooned duct produces a swelling in the vestibule adjacent to the posterolateral margin of the hymenal ring (Fig. 66–1A). Pressure causes the swelling to be sensitive and even painful to touch (Fig. 66–1B). If the duct is colonized via vaginal or rectal flora, then the mucous cyst may become septic, producing a Bartholin duct abscess. This disorder is associated with cellulitis, erythema, and fever.
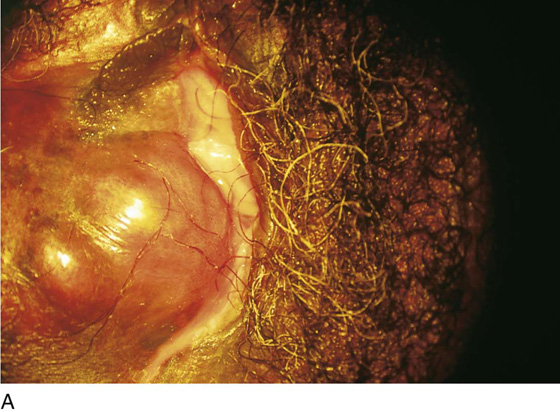
Treatment for a Bartholin cyst or abscess is drainage. A large opening should always be made in the cyst and its walls prevented from coapting and closing for 1 to 2 weeks. This may be accomplished by a variety of techniques, including marsupialization of residual margins of the open duct, insertion of a drain, and insertion of a Word catheter. The simplest technique is usually the best treatment regimen (Fig. 66–2A through C).
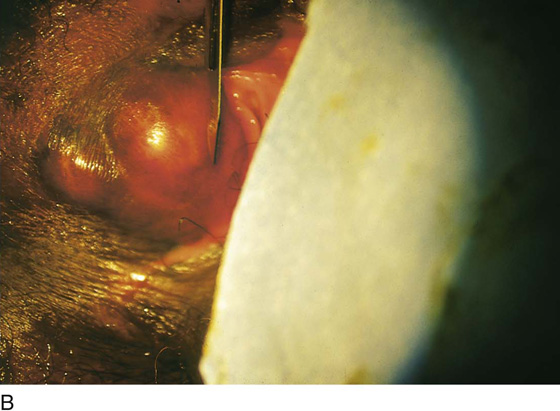
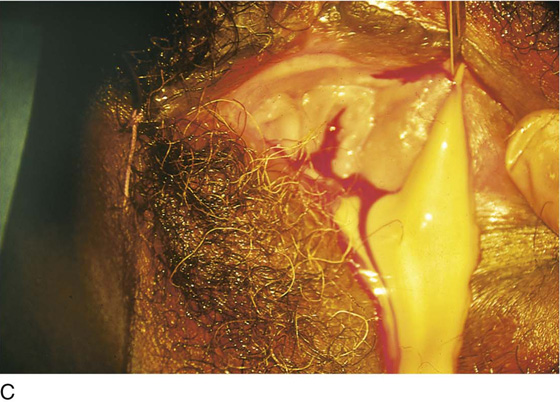
The patient may be anesthetized with general, regional, or local anesthesia. Two or three 0 Vicryl sutures are placed into the labia on the affected side and into the crural fold for retraction. The cystic swelling is incised vertically, and the draining interior fluid is cultured. Next, the skin and cyst wall are cut away, thereby greatly enlarging the opening (Fig. 66–3A through E). The cut edges are closed by a running lock stitch of 3-0 polydioxanone (PDS) or Vicryl. A small drain is sutured into the cavity with 3-0 chromic or plain catgut (Fig. 66–4). The patient is instructed to soak for 10 to 15 minutes in a tub bath to which 2 cups of salt (e.g., Instant Ocean sea salt) has been added twice per day for 1 to 2 weeks. She should rinse with fresh water after the soaking. The genital area may be blown dry with a hair dryer on the nonheat cycle or gently towel-dried.
FIGURE 66–1 A. The obstructed duct of the Bartholin gland produces swelling in the vestibule. This will produce discomfort for the patient. In this case, no evidence of infection is noted. B. This cystic lesion is secondary to an obstructed Skene duct.
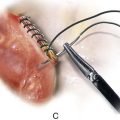
FIGURE 66–2 A. This woman was hospitalized with a painful vulvar mass, which failed to respond to administration of oral antibiotics. She had a past history of recurrent Bartholin duct cysts. This photo shows tremendous swelling of the left vulva and cellulitis extending into the mons. B. Drainage was accomplished by an incision into the mass at its most dependent, medial (vestibular) site. The operator’s finger is inserted into the abscess cavity to break up all septa to ensure complete drainage. Note: The finger is extended into the lower portion of the mons. C. A circular piece of skin has been excised (2-cm diameter), and the perimeter of the opening has been sutured via a running 0 Vicryl stitch. A through-and-through ¾-inch Penrose drain has been placed.
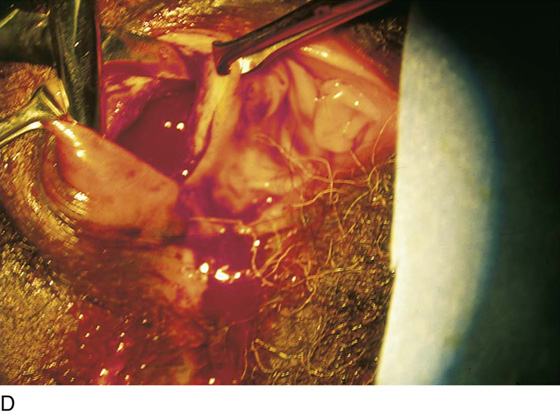
FIGURE 66–3 A. Another patient with a large Bartholin duct abscess, which distorts the vulva. B. The knife blade is prepared to cut the skin and penetrate the abscess cavity medially and dependently. C. Pus pours from the drainage site. D. A scissors is placed into the crater and spread open to break up any septa. E. The perimeter of the large opening (into the abscess cavity) is closed with a running 0 Vicryl suture.
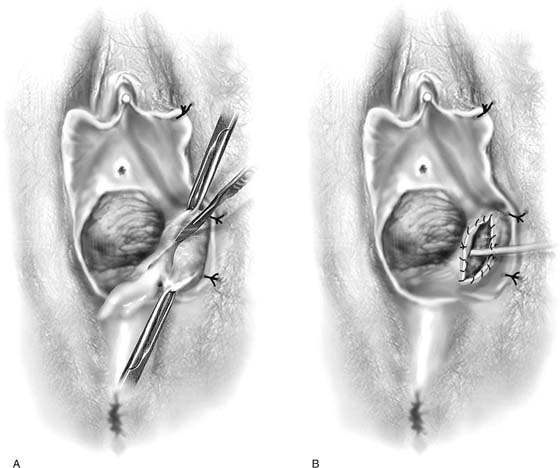
FIGURE 66–4 A. and B. The labia on the affected side are sutured back with 0 Vicryl to provide exposure. A vertical incision is made into the cyst. The edges of the incision are grasped with forceps and Allis clamps. The skin, together with a portion of the cyst lining, is widely cut away with a scalpel or Stevens scissors. The edges of the cut are sutured circumferentially with 3-0 Vicryl or polydioxanone (PDS). A drain is placed into the wound and secured with 3-0 chromic catgut. The cyst thus has been “marsupialized.”